Suning Teto Francine Laure and Bodzewan Emmanuel Fonyuy*
Registered Nurses-Bamenda, North West Cameroon
*Corresponding Author: Bodzewan Emmanuel Fonyuy, Registered Nurses-Bamenda, North West Cameroon.
Received: November 26, 2019; Published: December 10, 2019
Citation: Suning Teto Francine Laure and Bodzewan Emmanuel Fonyuy. “Breast Cancer Prevention: Assessment of the Knowledge and Practical Measures Employed by Young Female Adults in its Prevention”. Acta Scientific Paediatrics 3.1 (2020):15-23.
Cancer constitutes an enormous burden on society in more and less economically developed countries alike. Breast cancer arises when abnormal cellular growth occurs in certain structures and types of cells within the breast. The occurrence of cancer is increasing because of the growth and aging of the population as well as an increasing prevalence of established risk factors such as alcohol consumption, smoking, overweight, physical inactivity, reproductive and hormonal factors such as long menstrual history, recent use of oral contraceptives, and never having children.
The main objective was to assess the knowledge and practical measures employed by young female adolescents in the prevention of Breast Cancer in the College for Registered Nurses Bamenda.
A sample size of 76 young female adolescents aged 19-35 years from TSSRN Bamenda were recruited. A systematic random sampling method was used to collect primary data with the use of the structured questionnaire designed to obtain responses from the respondents.
Results show that, out of 76 respondents, 89.5% admitted they can differentiate a normal breast from an abnormal breast; among them, 41.3% said that an abnormal breast looks like a palpablehard mass/lump/nodule, 30.8% said breast/nipple larger than normal, 13.5% said asymmetrical breast, This shows that the majority of respondents know how an abnormal breast looks like.
As regards the signs and symptoms of Breast Cancer, 33.1% of the responses said inflammation of the breasts, 31.4% were thickening painless lump/nodules in the breasts on palpation, 15.7% were change in size, shape, and color of the breast, 14.0% were bloody discharges from the nipple.
After close analyses of the data collected, it can be deduced from the results that, 97.4% was aware of Breast Cancer and among those who were aware, 60.6% got it from knowledge acquired from school; 90.8% of them practiced BSE at home but 9.2% did not know how to do it. Almost the majority of respondents have an idea on Breast Cancer definition, predisposing factors, signs and symptoms, preventive measures but just few were not knowledge on Breast Cancer. Even though they have deficit knowledge, they thought that awareness can reduce Breast Cancer incident rate. In addition, 73.1% knew how to examine their breast through BSE and how to prevent Breast Cancer against 1.9% who did not know how to practice BSE at home.
Keywords: Breast Cancer; Knowledge; Prevention; Self-Breast Examination; Nodule; Mammography; Mastectomy
Cancer constitutes an enormous burden on society in more and less economically developed countries alike. The occurrence of cancer is increasing because of the growth and aging of the population as well as an increasing prevalence of established risk factors such as alcohol consumption, smoking, overweight, physical inactivity, reproductive and hormonal factors such as long menstrual history, recent use of oral contraceptives, and never having children (Arendt et al., 2010).
Giving birth to children and breastfeeding decrease the risk of breast cancer. Potentially modifiable risk factors include weight gain after 18years, being overweight/obese for post-menopausal breast cancer, uses of menopausal hormone therapy (combined estrogen and progestin), associated with urbanization and economic development. About 14.1 million new cancer cases and 8.2 million deaths occurred in 2012 worldwide. Over the years, the burden has shifted to less developed countries (Hussein A. Assi., 2013).
Breast cancer arises when abnormal cellular growth occurs in certain structures and types of cells within the breast (Arendt., et al. 2010). Breast cancer is the most common malignant cancer which occurs in both men and women, but it is far more common in women. Despite variances in risk factors, incidence rate of breast cancer in young women vary little between countries (Hussein A. Assi., 2013).
Breast cancer is the most frequently diagnosed cancer and the leading cause of cancer death among females worldwide, with an estimated 1.7 million cases and 521,900 deaths in 2012. Breast cancer accounts for 25% of all cancer cases and 15% of all cancer deaths among females. Most developed countries account for about one-half of all breast cancer cases and 38% of deaths. Rates are generally high in Northern America, Australian/New Zealand, Northern and Western Europe; intermediate in Central and Eastern Europe, Latin America, and the Caribbean; and low in most of Africa and Asia. International variation of breast cancer incidence rates reflects differences in the availability of early detection as well as risk factors.
According to the American Cancer Society, breast cancer remains the leading cause of cancer death among females in less developed countries (ACS, 2015). Incidence and mortality rate for breast cancer are decreasing in developed countries while in several less developed and economically transitioning countries, it is increasing because of adoption of unhealthy lifestyle and many environmental factors; breast cancer incidence rate has increased slightly among Africans (ACS, 2013).
According to the National Cancer Institute Surveillance (NCIS), epidemiology and end results data base, 2.7% of breast cancer occurs in women younger than 35 years of age (Deborah, 2008).
According to the latest WHO data published in 2017, breast cancer death in Cameroon reached 1.382/0.63 % of total deaths. The age adjusted death rate is 19.45 per 100,000 of population ranks Cameroon number 62 in the world.
There are several ways to prevent global burden of breast cancer. Firstly, maintaining a healthy body weight, increasing physical activity, minimizing alcohol intake and Breast Self Examination for lumps, tumors, masses, abdominal increase in size, discharges, are the best available strategies to reduce the risk of developing breast cancer. Secondly, early screening of the breast (Mammography) can often detect breast cancer at an early stage, when treatment is more effective and a cure is more likely (however, mammography screening is not perfect. Not all breast cancer will be detected by a mammogram and some Breast cancers that are screen-detected still have a poor prognosis. Sometimes mammography results in false-positive results as well as over diagnosis and overtreatment of some cancer. In spite of these limitations, numerous studies have shown that early detection with mammography save lives and increases treatment options. However, implementation of population-based organized mammography screening programs maybe cost-prohibitive in many less developed countries and is only recommended for those countries with a good health infrastructure that can afford long-term screening program). Finally, mastectomy can be done to avoid mortality cases from breast cancer. Substantial support for breast awareness and research findings has helped create advances in diagnosis and treatment of breast cancer. Breast cancer survival rate have increased and the number of death associated with this disease is steadily declining, largely due to factors such as earlier detection, a new personalized approach to diagnosis and better understanding of the disease.
The incidence of breast cancer in Cameroon is on the rise and accounts for a leading cause of mortality. An understanding of the knowledge and practices on Breast Cancer and Breast Self-Examination (BSE) are important first steps which will guide the designing of interventions aimed at raising awareness across the general population. A cross-sectional study was carried out in April 2016 involving 345 consenting female undergraduate students in the Higher Teachers Training College, Bambili, Cameroon.
What are the practical measures employed by young adults in the prevention of breast cancer?
To assess the knowledge and practical measures employed by young female adolescents in the prevention of Breast Cancer in the College for Registered Nurses Bamenda.
Young adults who are knowledgeable on the causes, risk factors, preventive measures and health consequences of breast cancer and who meticulously practice these preventives measures stand on lesser risk of developing Breast Cancer than those who do not.
The results of this study will bring out the knowledge gaps and the practical measures at the level of self-prevention by young female adolescents; it will equally help the health care providers to lay emphasis on these gaps and prevent the occurrence of Breast Cancer among them in the future.
The study was carrid out in the College for Registered NursesBamenda. It is situated in the Bamenda Health district (Azire Health Area, Nitop III) of the Bamenda II municipality in the Mezam Division of the North West Region of Cameroon.
The area has an undulating topography with Slopes and Valleys. It shares a common boundary with the Casualty Unit of the Bamenda Regional Hospital. The complex comprises not only the TSSRN Bamenda, but also the Training School for Laboratory Assistants, the Training School for Community Health Nurses and the Midwifery School.
It has the population of about 300 students with 7 classrooms (2018-2019 academic year). The Health Area is bounded to the North by Alakuma and Mulang Health Areas, to the South by Atuakom and Mbachongwa Health Areas, to the East by Ntamulung and Ntabag Health Areas, and to the West by Akumlam Health Area. The TSSRN Bamenda is headed by a Director who is answerable to the Regional Delegate for Public Health. He has as team members the Dean of Studies, the Chief of Finance and the Disciplinary Council Team made up of the staff of the institution.
The descriptive cross-sectional study design was used, in which the investigator collected data on the knowledge and practical measures employed by female adolescents in the prevention of Breast Cancer and their responses analyzed as per the study objectives.
The study population was all the young female adolescents aged 19-35 years schooling in TSSRN Bamenda. Those excluded in the study were boys, girls below 19 years, women above 35 years.
A sample size of 76 young female adolescents aged 19-35 years from TSSRN Bamenda were recruited. A systematic random sampling method was used in which every 5th multiple integer value of female students arriving the lecture hall in the morning was recruited for the study and the primary data collection questionnaire administered to them to complete and submit to the investigator.
Pre-testing was done in the Full Gospel Training School for State Registered Nurses Bamenda because it has the same standard and similar features as the TSSRN Bamenda. This was to ensure that the questions were clear and easily understood by the respondents. After pre-testing, the flaws (poorly framed questions) and lapses (incoherent responses) were corrected and the questionnaire was valid for data collection.
The instrument/tool for data collection was structured questionnaires designated to obtain written answers from the respondents. Opened-ended questions were structured to reflect the specific objectives of the study.
The questionnaire was divided into sub-sections as follows:
The questions was answered and the information collected by the investigator on the spot.
The primary data obtained from the respondents were analyzed using Microsoft Word and Microsoft Excel. The results was presented in frequency, tables, pie-charts, bar-charts, etc and interpreted accordingly.
In order to carry out this study, Authorization letters were obtained from the Regional Delegation of Public Health for North West Region as well as approvals from the Directors of different schools in the complex. Verbal consent was obtained from the respondents after giving them explanations on the purpose of the study and assuring them of strict anonymity and confidentiality of information collected from them.
Age of respondents
From table 1, it can be seen that, out of a total of 76 respondents recruited for the study, 58% were within the age range of 20-24 years, 35.5% were within 25-29 years, and 14.5% were within 30-35 years.
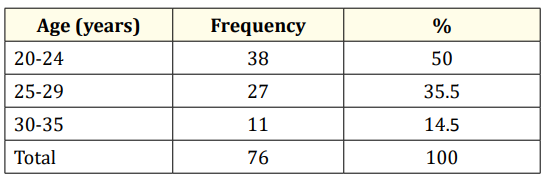
Table 1: Distribution of respondents according to age range.
From table 2, it can be seen that, out of 76 respondents recruited for the study, 31.6% were within the weight range of 50-59kg, 42.1% were within 60-69Kkg, 17.1% were within 70-79kg and 9.2% were from 80kg and above.
From the figure 1, it can be seen that, 26.3% were married while 73.7% were not married. No divorce case was registered.
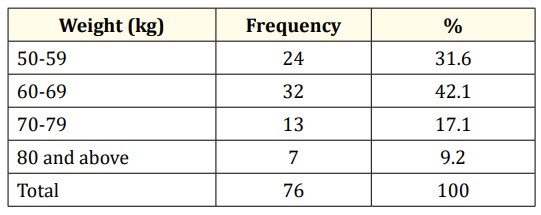
Table 2: Distribution of respondents according to weight.
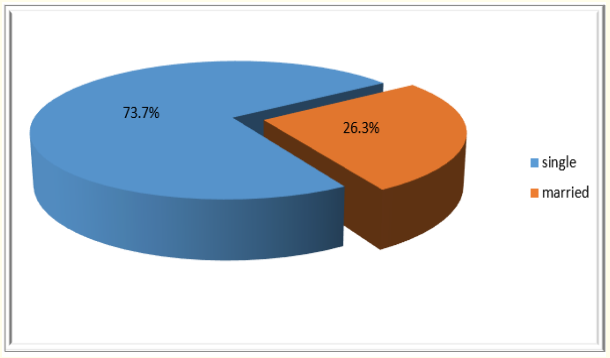
Figure 1: Distribution of respondents according to marital status
From the figure 2, 75.0% of respondents were not having children, 17.1% were having 1 child and 7.9% were having 2 children
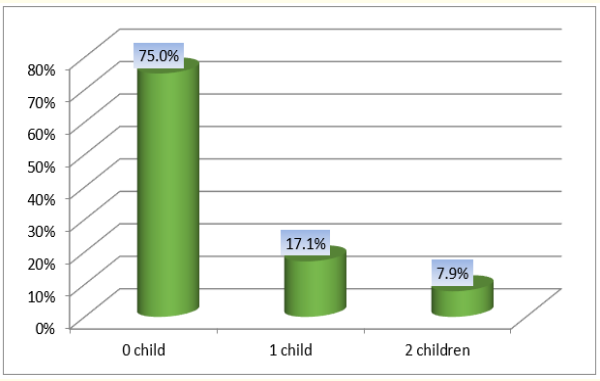
Figure 2: Distribution of respondents according to number of children alive.
The results from figure 3 show that, out of 76 respondents recruited, 97.4% have heard about Breast Cancer while 2.6% have never heard about Breast Cancer.
From figure 4, the results shows that 60.6% heard about Breast Cancer in school, 23.4% heard in the hospital, 10.6% heard via media and 5.3% heard from the community.
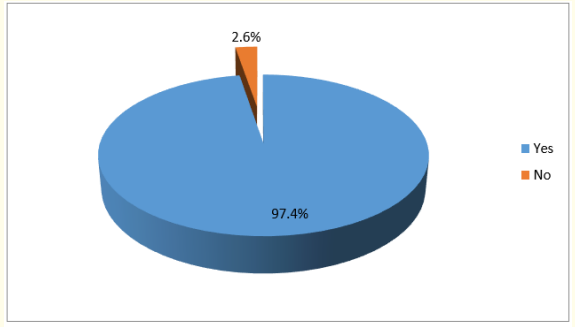
Figure 3: Distribution of respondents according to whether they have heard about breast cancer.
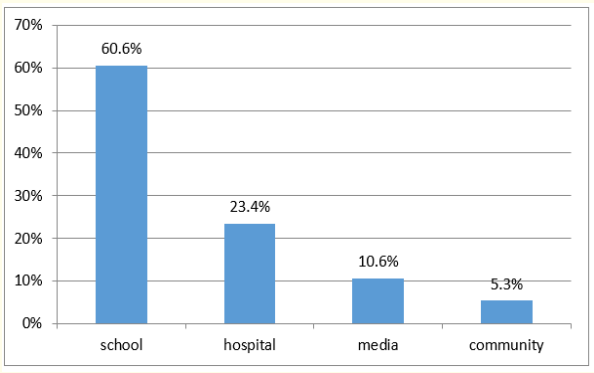
Figure 4: Distribution of respondents according to where they heard about breast cancer.
From table 3, it can be seen that 55.3% of respondents said that Breast Cancer were an abnormal growth of cells in the breast; 17.6% said the presence of nodule/lump in the breast; 14.1% said tumor of the breast; 8.2% said change in the size/shape of the breast/nipple; 2.4% said pitting/redness of the skin of the breast like the skin of an orange; 1.2% said pain in armpit/breast; and 1.2% said discharge from a nipple, possibly containing blood.
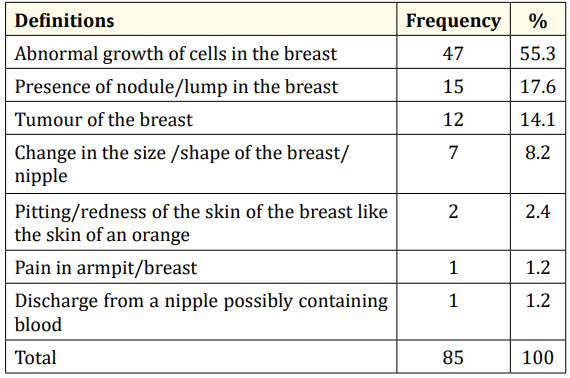
Table 3: Distribution of respondents according to their definition of Breast Cancer. Survey data (Suning, 2019).
The figure 5 shows that majority of respondents, (89.5%) said that they can differentiate a normal breast from an abnormal one while 10.5% could not differentiate.
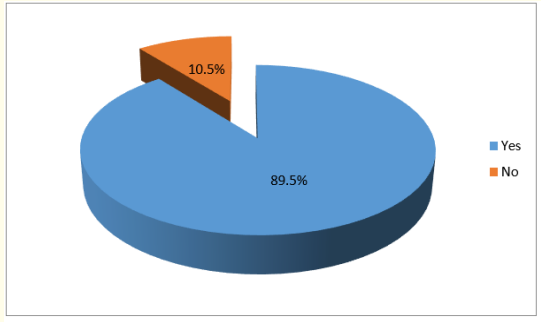
Figure 5: Distribution of respondents according to whether they can differentiate between normal and abnormal breast.
From the figure 6, it can be seen that, 41.3% of respondents said that an abnormal breast look like a palpable hard mass/lump/ nodule; 30.8% said breast/nipple enlarge than normal; 13.5% said asymmetrical breast; 11.5% said painful swollen breast; 2.9% said rash on the nipple.
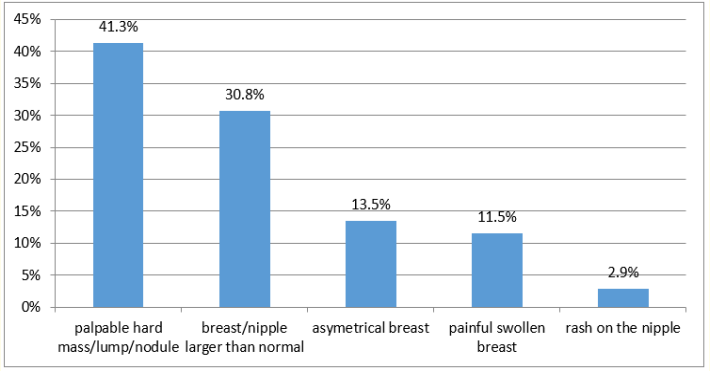
Figure 6: Distribution of respondents according to how they think an abnormal breast looks like.
From the table 4, 33.1% of the respondents said that symptoms of BC were inflammation of the breast; 31.4% said thickening painless lump/nodule/in the breast on palpation; 15.7% said change in size, shape, and color of the breast; 14% said bloody discharge from the nipple; 2.9% said rashes/lesions of the nipple/breast and another 2.9% said inverted nipple.
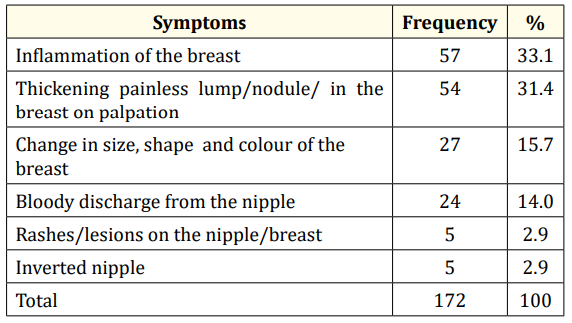
Table 4: Distribution of respondents according to their knowledge on symptoms of breast cancer.
From the table 5, 34.1% said they don’t know the cause of BC; 29.4% said chemical and exposure to radiation; 23.8% said unknown; 7.9% said mutation and genetic factors; 4.8% said breast abscess.
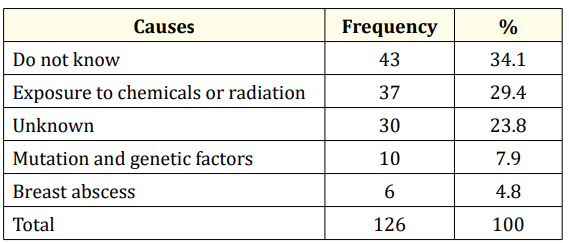
Table 5: Distribution of respondents according to their knowledge on causes of breast cancer
From table 6, 23.3% of respondents said that the risk factors of BC are poor life style; 18.0% said chemotherapy/radiation; 16.5% said hormonal factors; 15.8% said family history; 9.8% said high fitting breast wear/breast ironing; 5.3% do not know; another 5.3% said being a woman; 3.0% said no breastfeeding; 1.5% said early menarche; finally 1.5% said tattoo on the breast.
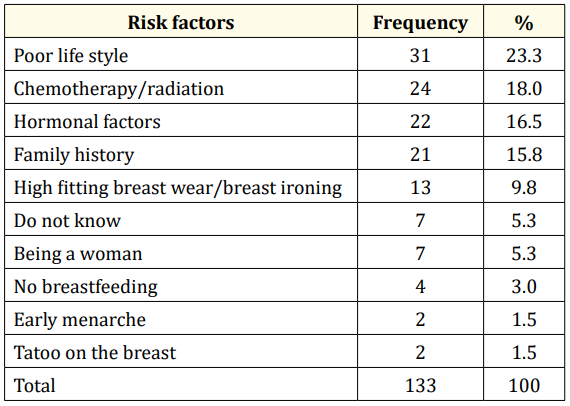
Table 6: Distribution of respondents according to their knowledge on the risk factors of breast cancer.
Responses of Respondents on if they know measures to prevent Breast Cancer.
From figure 7, the majority of respondents that is 90.8% said that they know measures to prevent BC while 9.2% said they did not know.
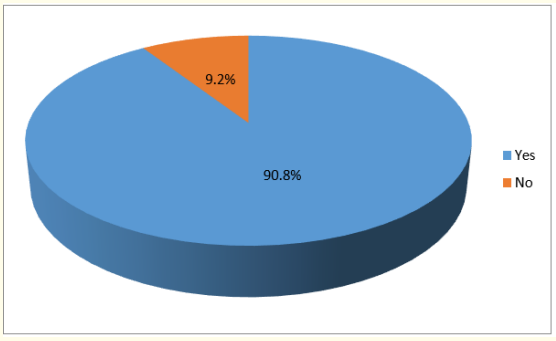
Figure 7: Distribution of respondents according to whether they know measures to prevent breast cancer.
From table 7, 46.5% of respondents said that the measures to prevent BC is BSE; 22.5% said healthy life style; 16.2% said avoid exposure to radiation; 4.2% said avoid high fitting breast wear; 3.5% said mammography; 2.8% said exclusive breastfeeding; 2.1% said avoid hormonal therapy for menopausal women; 1.4% said avoid deodorant spray and 0.7% said avoid plastic surgery
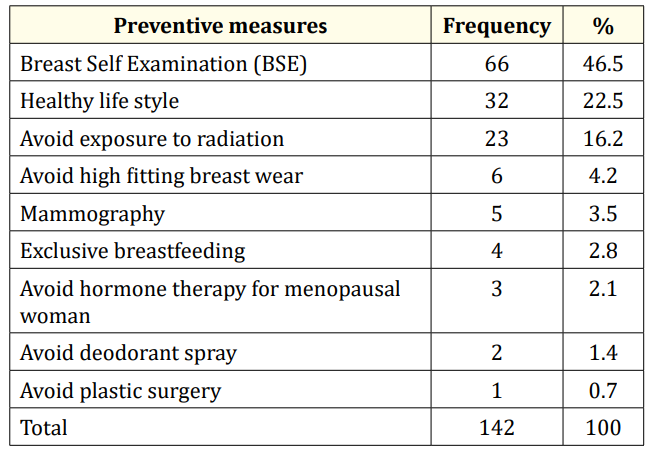
Table 7: Distribution of respondents according to their knowledge on measures to prevent breast cancer.
From figure 8, 68.4% of respondents said they know how to practice BSE at home while 31.6% said they didn’t know.
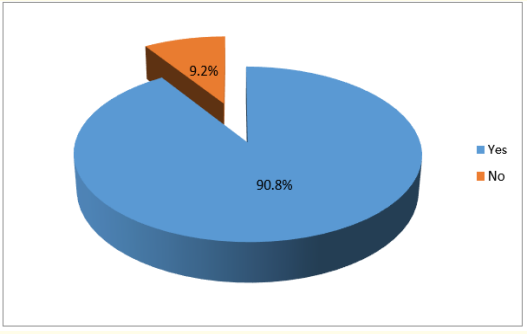
Figure 8: Distribution of respondents according to whether they practice BSE at home.
From table 8, 73.1% of respondents said that to practice BSE, lie in supine position/stand straight, left hand behind the occiput, use the right hand to check the left breast and vice versa, palpate with the palm in a circular manner to check for abnormalities. 25% said observation and palpation of the breast for lump, nodule and any abnormalities. 1.9% said when bathing, they touch or press the breast with fingers.
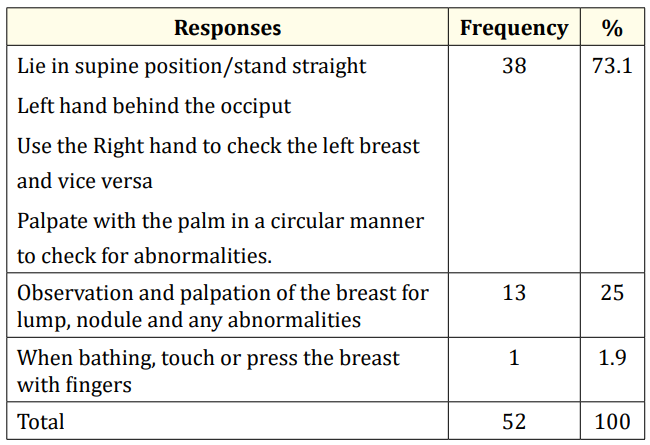
Table 8: Distribution of respondents according to how they practice BSE at home.
From table 9, 13.3% said they encountered no problem in the prevention of BC, 12.2% said time constraint, 17,8% said not being able to identify normal fatty tissue of the breast with a nodule/ lump/mass, 22.2% said difficulties to do BSE properly, 16.7% said forgetfulness, 3.3% said no access to a large mirror, 4.4% said lack of privacy in an overcrowded house, 8.9% said lack of interest and negligence, and 1.1% said fear to discover abnormal nodules.
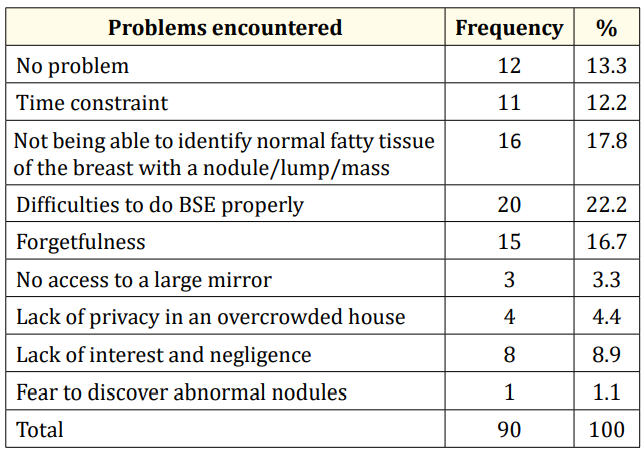
Table 9: Distribution of respondents according to the problems they face in the prevention of breast cancer.
From the table 10, 37% said that they need to have a proper education on Breast Cancer prevention, how to practice BSE properly, how often BSE should be done and the best time to do it. 8.7% said no additional information, 22.8% said that they need to know the real cause of BC and preventives measures other than BSE, 10.9% said that they need more education on risk factors of Breast Cancer and finally, 1.1% said if Breast Cancer can be treated.
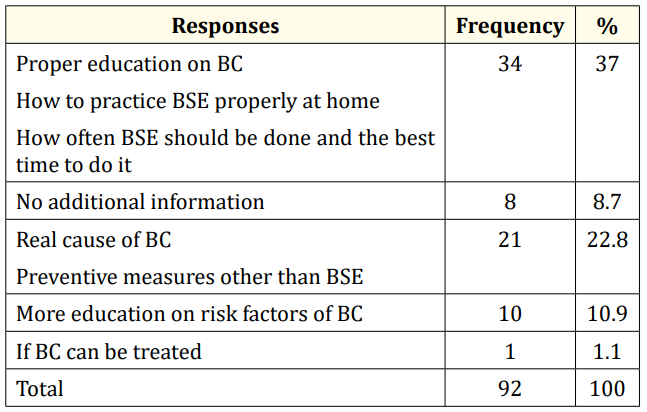
Table 10: Distribution of respondents according to the additional information they need from the health care providers to better prevent BC later on in life.
It was observed that, the majority of respondents that is 50% were between the age group of 20-24 years. This is obvious because the youths form the bulk of the population in any given community. This is why Rosses (2013) said that age was as an important factor in the prevention of Breast Cancer.
Also, 42.1% were having between 60-69kg while only 9.2% were having 80kg and above. This shows that the weight of the majority was relatively normal and according to Hussein A. Assi (2013), obesity increase risk of Breast Cancer.
Concerning marital status, it was observed that, 73.7% of the respondents were still single while only 26.3% were married.
Also, out of 76 respondents, 75% were not having child, 17.1% were having a child, and 7.9% were having two children. This shows that it was only the minority who practiced breastfeeding and according to Lancey., et al. (2009), breastfeeding has a protective effect against breast cancer.
According to figure 3, the majority 97.4% of respondents have heard about breast cancer probably because the incidence of Breast Cancer in Cameroon is on the rise and accounts for a leading cause of mortality. This is supported by American Cancer Society (2015) which stated that, Breast Cancer remains the leading cause of cancer death among females in less developed countries.
From figure 4, out of those who heard about Breast Cancer, 60.6% have heard about it in school, this is probably because the module pathology is taught from Year two and Breast Cancer features under reproductive system pathologies and cells and tissues pathologies.
From table 3, it was observed that, a greater proportion of respondents 55.3% knew the definition of Breast Cancer as an abnormal growth of cells in the breast, 17.6% said that it is the presence of nodule/lump in the breast, 14.1% said tumor of the breast, 8.2% said change in the size/shape of the breast/nipple, 2.4% said the pitting/redness of the skin of the breast like the skin of an orange, 1.2% said discharges from the nipple possibly containing blood. This shows that the majority of the respondents had an idea about Breast Cancer. This is in line with the National Cancer Institute (2011) that defined Breast Cancer as a Cancer that forms in the tissues of the breast. Also, American Cancer Society defines Breast Cancer as cancer that starts when cells in the breast begin to grow out of control. These cells usually form a tumor that can often be seen on an x-ray/felt as a lump (ACS, 2017).
From figure 5, it was observed that, out of 76 respondents, 89.5% admitted that they can differentiate a normal breast from an abnormal breast. Among them, 41.3% said that an abnormal breast looks like a palpable hard mass/lump/nodule, 30.8% said breast/nipple larger than normal, 13.5% said asymmetrical breast, 11.5% said painful swollen breast, 2.9% said rash on the nipple. This shows that the majority of respondents know how an abnormal breast looks like.
As regards to the signs and symptoms of Breast Cancer, 33.1% of the responses were inflammation of the breast, 31.4% were thickening painless lump/nodules in the breast on palpation, 15.7% were change in size, shape, and color of the breast, 14.0% were bloody discharges from the nipple, 2.9% were rashes/lesions on the nipple/breast, 2.9% were inverted nipple. This is supported by the center for disease control and prevention who said that the possible signs and symptoms of Breast Cancer include: -Lump in the
Breast/ Armpit
Concerning the causes of Breast Cancer, 34.1% of responses were empty, meaning that the majority don’t know what cause Breast Cancer this maybe because the exact cause of Breast Cancer remains unclear. This was supported by the National Breast Cancer Foundation (2016) who stated that “no one knows the exact causes of Breast Cancer.
According to table 6, out of 76 respondents, 23.3% of responses were poor lifestyle, 18.0% were chemotherapy/radiation, 16.5% were hormonal factors, 15.8% were family history, 9.8% were high fitting breast wear/breast ironing, 5.3% of responses were empty meaning that they have no idea, 5.3% were being a woman, 3.0% were breastfeeding, 1.5% were early menarche, and 1.5% were tattoo on the breast. This shows that Breast Cancer predisposing factors is divided into modifiable and non-modifiable. This was supported by CDC (2018) that states that risk factors for Breast Cancer include risk factors that you can change and the risk factors that you cannot change.
According to figure 7, the majority of respondents that is 90.8% said that they know measures to prevent Breast Cancer against the minority of 9.2% who said they don’t know. From table 7, 46.5% responses were BSE, 22.5% were healthy lifestyle, 16.2% were avoid exposure to radiation, 4.2% were avoid high fitting breast wear, 3.5% were mammography, 2.8% were exclusive breastfeeding, 2.1% were avoid hormone therapy for menopausal woman, 1.4% were avoid deodorant spray and 0.7% were avoid plastic surgery. This shows that the majority of respondents know measures to prevent Breast Cancer for, prevention is better than cure.
From figure 8, 90.8% of respondents practice BSE at home and only 9.2% do not ; according to National Breast Cancer Foundation reports (2014), all adults women of all ages are encouraged to perform BSE at least once a month.
As regard how the BSE can be practice to prevent Breast Cancer, 73.1% of the responses were: lie in supine position/stand straight left hand behind the occiput, use the right hand to check the left breast and vice-versa, palpate with the palm in a circular manner to check for abnormalities, 25% of responses were: observation and palpation of the breast for lump, nodule, and any abnormalities, 1.9% of responses were: when bathing, touch/press the breast with fingers. This shows that the majority know how to practice BSE.
Concerning the difficulties faced by the respondents in the prevention of Breast Cancer, 13.3% of the respondents said no problem, 12.2% said time constraint, 17.8% not being able to identify normal fatty tissue of the breast with a nodule/lump/mass, 22.2% said difficulties to do BSE properly, 16.7% said forgetfulness, 3.3% said no access to a large mirror, 4.4% lack of primary in an overcrowded house, 8.9% said lack of interest and negligence, 1.1% fear to discover abnormal nodules. This show that the respondents need to be updated on preventives practices which can help to reduce the incidence of Breast Cancer in the future.
As regards additional information to be provided by the state holders/ministry of public health to enhance proper prevention of Breast Cancer, 37% said they need: proper education on BC, how to practice BSE properly at home, how often BSE should be done and the best time to do it, 8.7% said no additional information, 22.8% said real cause of Breast Cancer and preventive measures other than BSE, 10.9% said more education on risk factors of Breast Cancer, 1.1% if Breast Cancer can be treated [1-43].
After close analyses of the data collected, it can be deduced from the results that, 97.4% was aware of Breast Cancer and among those who were aware, 60.6% got it from knowledge acquired from school; 90.8% of them practiced BSE at home but 9.2% did not know how to do it. Almost the majority of respondents have an idea on Breast Cancer definition, predisposing factors, signs and symptoms, preventive measures but just few were not knowledge on Breast Cancer. Even though they have deficit knowledge, they thought that awareness can reduce Breast Cancer incident rate. In addition, 73.1% knew how to examine their breast through BSE and how to prevent Breast Cancer against 1.9% who did not know how to practice BSE at home.
Copyright: © 2020 Suning Teto Francine Laure and Bodzewan Emmanuel Fonyuy. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.