Amal Alfakhri1, Esaida Elzaraough2, Raja Alfakhri3* and Hajer Elkailani2
1Commuinty and Family Medicine Department, University of Benghazi, Libya
2Benghazi Children’s Hospital, Libya
3Physiology Department, University of Benghazi, Libya
*Corresponding Author: Raja Alfakhri, Physiology Department, University of Benghazi, Libya.
Received: September 27, 2019; Published: November 07, 2019
Citation: Raja Alfakhri., et al. “The Effectiveness of Intensive Phototherapy in Reducing Exchange Transfusion in Neonatal Jaundice Cases in Year 2016 Compared to 2013/ Benghazi”. Acta Scientific Paediatrics 2.12 (2019):23-27.
Neonatal jaundice is the most common morbidity in the first week of life, The Aims is to assess the effectiveness of intensive phototherapy in reducing the need for double volume exchange transfusion (DVET) as a management strategy. A retrospective matched cross-sectional study was done by extracting the data from hospital archived files of neonates admitted due to neonatal jaundice during two past un-consecutive years specifically 2013 and 2016.There was a significant difference between two groups regarding mode of delivery, since operative labour was more common in 2016 than in 2013 (P = 0.023). Rh incompatibility between the mothers and their infants of the two study years was not as important cause of haemolysis as ABO blood group mismatching (2013 Chi = 23, P < 0.00, 2016 Chi = 27, P < 0.00).The need for DVET was considerably lower in 2016 (Chi = 15.13, P < 0.00) as well as serum bilirubin level (p = 0.004) (18.7 ± 4.2 mg/dl and 20.4 ± 4.4 mg/dl in 2016 and 2013) consecutively. The introduction of intensive phototherapy in management of neonatal jaundice led to dramatic reduction in the need for DVET in 2016 compared to 2013.
Keywords: Hyperbilirubinemia; Double Volume Exchange Transfusion; Intensive Phototherapy
Neonatal jaundice is a common and mostly benign peadiatric health problem, it is considered to be an important clinical condition because it is associated with high morbidity and mortality. It has been reported that the condition is the commonest cause of neonatal admission to the children’s hospitals especially in the emergency room [1].
Under normal circumstances, the level of bilirubin rises at birth and signs of jaundice becomes visible, usually peaking between the 2nd and 4th day. However, the levels start to decrease between the 6th and 8th days of life [2]. This type of jaundice is referred to as physiological and may result from defective transport of bilirubin into hepatocyte [3] low activity of bilirubin conjugating enzyme, excessive load of bilirubin to liver than it can conjugate due to its immaturity at birth [4]. Physiological jaundice occure in over half of term and 80% of preterm neonates [5]. The clinical signs include yellow discoloration of the skin and sclerar.
In contrast, hyperbilirubinemia might be pathological and it is the main reason for hospital readmission during the neonatal period [6]. Pathological jaundice is considered when total serum bilirubin (TSB) levels exceeding the range of physiological jaundice, which is defined arbitrarily and loosely as more than 5 mg/dL on first day, 10 mg/dL on second day, and 12-13 mg/dL thereafter in term neonates. Any TSB value of 17 mg/dL or more should be regarded as pathological and should be evaluated for the cause, and possible intervention, such as phototherapy [7]. If Jaundice persists after the third day of life, this may suggest a severe form of hyperbilirubinemia, requiring clinical intervention and management. The goal of therapy is to lower the concentration of circulating bilirubin or prevent it from increasing [8].
The most serious complication is Kernicterus which is a neurological condition characterized by deep yellow staining of the basal nuclei. Though it is a preventable when appropriate diagnosis, treatment and follow-up of infants are guaranteed. Usually, the symptoms of kernicterus are manifested within 2-5 days after birth in term infants and 7 days after birth in preterm newborns [8].
The accompanying clinical syndrome results from the destructive changes of these neuronal tissues are lethargy, hypotonia, poor feeding, bulging fontanelle, abnormal movements of the face and extremities and shrill cry, and loss of Moro reflexes, decreased deep tendon reflexes and seizures. Later, the infants may develop athetoid cerebral palsy, mental retardation and deafness. When neurological signs evident in the infant, permanent damage has already occurred, leading to death or long term disability [8].
The management strategies are aimed at preventing kernicterus. Until recently, these strategies suggested maintaining serum unconjugated bilirubin concentrations below 340 _mol/L (20 mg/ dL) in healthy term infants through the use of phototherapy or exchange transfusion [9]. Therefore; treatment modalities are either exchange transfusion, phototherapy or combination. Thus, it is the aim of this study to determine the effectiveness of intensive phototherapy in reducing the need DVET compared to the conventional phototherapy between the years 2013 and 2016, which is promising treatment in reducing the need for that invasive management and its complication. The second aim is to recognize how the intensive phototherapy might reduce the duration of infant hospitalization rand consequently reduce the economic burden of the hospital and the country.
A retrospective hospital based cross sectional study was conducted by reviewing information of a convenient quota sample of archived files of the infants admitted due to neonatal jaundice during two un-consecutive years which are 2013 and 2016, a total sample of 240 files were recollected, 120 file from each year. Matching was considered so that the two groups were similar in age structure of the two sample groups, male to female ratio, gestational maturity (term to preterm) and in the mean birth weight (table 1).
Data was collected using a pre designed sheet was prepared to be filled up from the file of each infant (The appendix).
The following characteristics were considered to include the infant in the survey:
Prior to the survey checklist filling up, a permission from the administrative personal was assured to get an access to the archived files, in addition the collected data was used to address a scientific issue, as a trial to increase the orientation about the uses of intensive phototherapy in neonatal jaundice, and no other unpleasant aim is intended, furthermore the researcher and his supervisors are entirely responsible about all the consequences of the study.
Statistical package of social sciences (SPSS) version 21.0 was used for data entry processing and analysis.
Descriptive and inferential analysis of the data were used accordingly to describe the study population and find the associations and correlations between the studied variables. Demonstrating graphs, diagrams and tables were displayed when applicable, a significance level of less than 5% and 95% confidence interval were considered.
A sample of 240 infant 120 infant were born in the year 2013 (group 1) and 120 in 2016 (group 2). The analysis was done depending on the year as the management strategy was different and the difference in the outcome is the area of interest for this research project, therefore the groups will be described as group 1 and group 2 according to the year.
The two sample groups showed statistical significant difference according to mode of delivery (Figure 1) as the operative labor was higher in group 2 (Pearson chi square = 4.51, P= 0.023, Table 1).
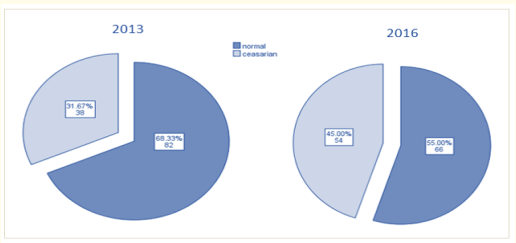
Figure 1: Mode of delivery of the two study groups.
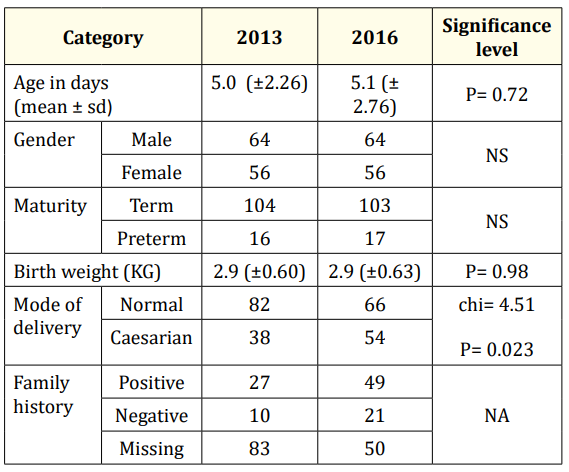
Table 1: Demographic and infant characteristics.
Blood groups of the mothers and infants were compared according to “ABO” and “Rh” system. Chi square test was conducted within each group to test the significance of difference between mothers and infants, the test revealed a very matching results in the two study groups as there was no significant difference in RH status between the mothers and infants, in group 1(2013), Pearson Chi square= 1.99, P=0.114, and in group 2 (2016) Pearson Chi square=0.95, P=0.21 (Table 2).
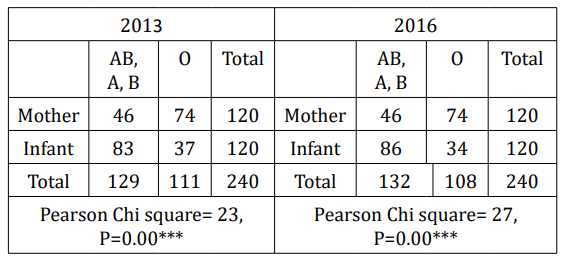
Table 2: ABO incompatibility between mothers and their infants of the two study years.
ABO blood grouping in group 1, there was a significant difference between mothers and infants in AB, A,B against O (Pearson Chi square= 23, P=0.00***), and similarly for group 2 (2016), there was a statistical significant difference in ABO blood grouping between mothers and infants (Pearson Chi square= 27, P=0.00***).
The serological investigations of the study groups were collected, the mean hemoglobin level is very close for the two groups, around 16.2 (P= 0.23), and so the mean hematocrite and mean platelet level. Post treatment mean total s. bilirubin is significantly higher in 2013 which is around 14.9 (±4.2) compared to 13.9 (±4.6) for 2016 P= 0.002, similarly for direct bilirubin.
Clinical characteristics of the sample (Table 3), for example the mean duration of hospital admission of the two study groups were very close (mean =2.3 days) and no significant difference in the mean duration of admission.
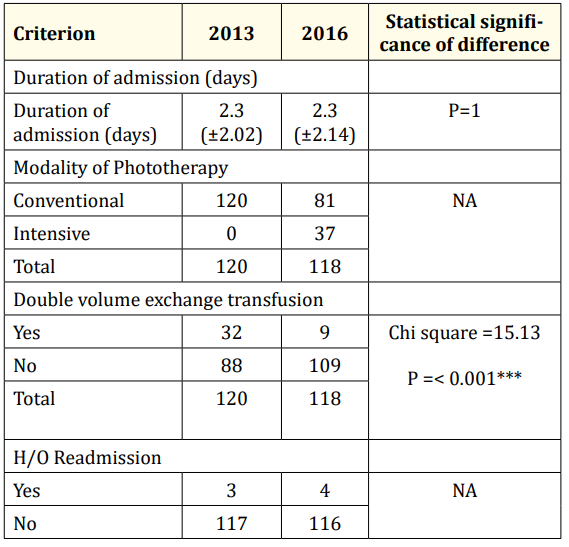
Table 3: Clinical characteristics of the study sample.
Regarding treatment modality, group 1 was entirely subjected to conventional phototherapy, while group 2 only 81 child exposed to conventional phototherapy and 37 child treated with intensive phototherapy.
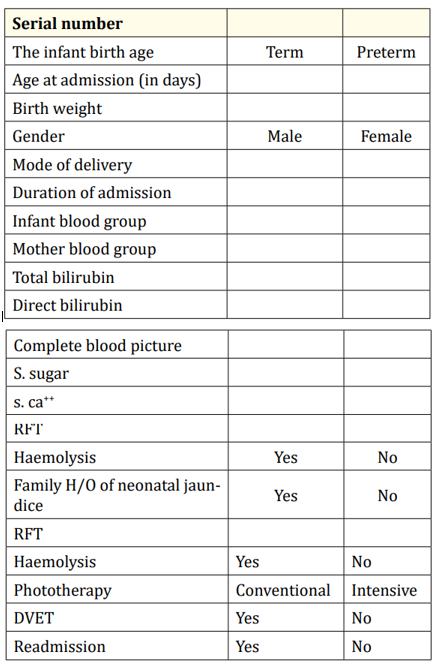
The need for DVET is different in the two study groups, as in group 1, 32 infants needed DVET compared to only 9 infants in group 2, and that difference is highly statistically significant (Chi =15.13, P= < 0.00) (Figure 2).
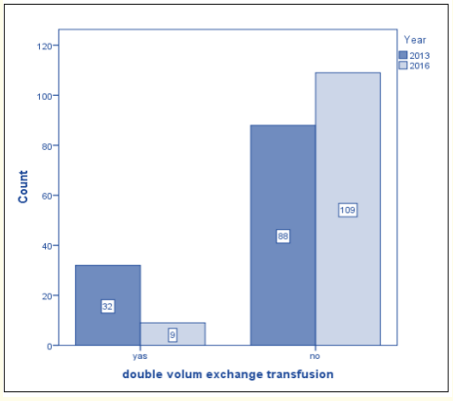
Figure 2: The need for DVET for the two study groups.
This study was conducted to compare the treatment strategy and its outcome for neonatal jaundice of a sample of two years which are 2013 and 2016, the two sample groups were very close and comparable for age, gender, birth weight and gestational age. However, the operative mode of delivery is significantly higher for the year 2016 compared to 2013 in which the normal vaginal delivery was more predominant.
There is a conflicting results regarding the effect of mode of delivery on occurrence and severity of jaundice, some suggest that unnecessary interventions during delivery such as excessive use of oxytocin during labor and caesarean section are considered as the risk factors for neonatal jaundice [10], agreeing with that, a study done by Tamook., et al. [11], found that the prevalence of jaundice was higher among neonates born by caesarean section, compared to those who were naturally delivered. On the contrary, Boskabadi and Navaei [12] found no significant relationship between mode of delivery and the incidence of jaundice.
Blood grouping of the mothers and their infants were studied as it is the main leading cause to neonatal jaundice in case of incompatibility, in this study it was found that mothers and their infants are very close in their ABO grouping and Rh status for the two sample groups. Regarding incompatibility, ABO mismatching between mothers and their infants was of great contribution for haemolysis and subsequently neonatal jaundice than RH incompatibility among the two study groups, this result might be explained by the use of anti D in case of Rh isoimmunization, while in case of ABO mismatching there is no available immune-prophylactic therapy, a recent study investigating neonatal jaundice [8] found that the most common causes if haemolysis was as the following ABO incompatibility, Rh incompatibility, G6PD deficiency, sepsis and infants of diabetic mothers.
Some clinical characteristics and blood investigations were compared, the mean duration of hospital admission was very close in the two years, in addition the mean levels of haemoglobin, hematocrite and platelets were almost similar with no any significant difference, contrary the mean serum total bilirubin level and direct bilirubin was significantly different as it is lower in 2016 than that of 2013, which could be referred to the use of intensive phototherapy in 2016.
The treatment modality of the two groups is the main focus of this study, all the infants of the year 2013 were treated with conventional phototherapy, out of them 32 infants needed DVET, while in the year 2016 conventional phototherapy was considered for 81 infants and 37 were subjected to intensive phototherapy, and only 9 infants needed DVET. There is a greater need for DVET in 2013 than in 2016 cases, and this difference has high statistical significance. This results is consistent with many studies proving that phototherapy decreases the need for exchange transfusion in newborns with severe hyperbilirubinemia, more over the dramatic reduction in the number of exchange transfusions being performed is considered as a measure of the efficacy of phototherapy [13].
A study done on Egyptian neonates to assess the effectiveness of using the intensive phototherapy in decreasing the Bilirubin level in shorter time and how it affected the rate of exchange transfusion in the management of neonatal hyperbilirubinemia. Newborns where divided to two groups, group 1 with high TSB near or over 20 mg/dl was put under highly intensive phototherapy for 4 hours, and group 2 those with less severe readings put under the usual phototherapy. Post phototherapy they found that the mean initial TSB for group 1 (No. 37) was 14.5 ± 2.6 mg/dl while in group 2 (No. 36) was 20.6 ± 3.74 with significant difference (p<0.001), therefore they proved that exchange transfusion rate was much decreased when highly intensive phototherapy was started in the management of neonatal jaundice [14].
Another prospective study done in Asuit with a very close aim, to assess the effectiveness of intensive phototherapy in comparison with conventional phototherapy in reducing the need for exchange transfusion and the duration of phototherapy for management of neonatal hyperbilirubinemia, concluded that the use of intensive phototherapy in the treatment of indirect pathological hyperbilirubinaemia has a similar effective as exchange transfusion in lowering TSB when its level is within 2-3 mg/dl (34-51 μmol/l) of the exchange level, whereas it is effective in reducing needs for exchange transfusion and duration of phototherapy [15,16].
Neonatal jaundice is a very common condition leading to infant hospitalization during early life all over the world, this study included a comparable study groups to find out about the effectiveness of intensive phototherapy in reducing the need for DVET compared to conventional phototherapy. The two groups were comparable in term of age structure, gender distribution, gestational age and birth weight. Whereas operative mode of delivery was significantly more frequent in group 2 (2016) than in group 2 (2013).
The introduction of intensive phototherapy in management of neonatal jaundice led to dramatic reduction in the need for DVET in 2016 compared to 2013 in which the conventional phototherapy was the only available mode of phototherapy.
Furthermore, TSB was significantly lower at the end of management when using intensive phototherapy (2016) than in case of conventional one (2013).
ABO incompatibility was the major underlying cause of haemolysis and neonatal jaundice among the two study groups.
Neonatal jaundice when properly managed is completely benign condition. Nevertheless, it could lead to serious irreversible consequences if appropriate care is delayed or neglected. Therefore, awareness of neonatal care providers should be raised to achieve the goal of “simple effort can save lives and money”.
Future study of similar issue is recommended using a more efficient design with prospective progress to avoid the limitations of this study which was, presence of missing data, and uncertainty of TSB level.
The appendix: Data collection sheet.
Copyright: © 2019 Raja Alfakhri., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.