Samah Alasrawi*
Pediatric Cardiologist, AlJalila Children Heart Center, Dubai, UAE
*Corresponding Author: Samah Alasrawi, Pediatric Cardiologist, AlJalila Children Heart Center, Dubai, UAE.
Received: September 27, 2019; Published: October 15, 2019
Citation: Samah Alasrawi. “Cardiology Approach to Kawasaki Disease ”. Acta Scientific Paediatrics 2.11 (2019):40-43.
Objectives: Kawasaki disease is an acute multi system vasculitis affects large and medium sized vessels of childhood, So, it can affect the coronary arteries, in this article we will focus on the cardiology approach to Kawasaki disease.
We will go through Investigations: Echo cardiography, stress test and catheterization, then the treatment and follow up for Kawasaki disease patients.
Conclusion: Kawasaki disease is a common childhood systemic vasculitis characterized by specific clinical features. Transthoracic echocardiography is recommended in suspected cases of Kawasaki disease, however a normal study does not exclude the diagnosis. Treatment with high dose intravenous immunoglobulin should be initiated based on the clinical presentation and should not be delayed by the timing of echocardiography.
Keywords: Kawasaki Disease; Cardiology; Approach
Kawasaki disease is an acute self-system vasculitis affects large and medium sized vessels of childhood.
Characterized by: Fever, Bilateral non exudative conjunctivitis Erythema of the lips and oral mucosa, Changes in the extremities, Rash, Cervical lymphadenopathy
Sudden death
But giant aneurysms (>8 mm) don’t resolve most of the time, and some may develop stenosis.
Echocardiography is used for the diagnosis of coronary artery lesions, it is sensitive and specific tool, and should be done in confirmed or suspected cases of Kawasaki disease at the time of diagnosis.
Treatment is recommended when there is a clinical presentation for Kawasaki disease, and should not be delayed until we do the echocardiography.
But if full clinical criteria are not met and there are coronary artery lesions on echocardiography, then the child has incomplete features of Kawasaki disease and we have to treat.
The main aim of echocardiography in Kawasaki disease is to identify coronary artery lesions, and the other inflammation process in the heart like pericarditis and/or myocarditis.
We can evaluate the coronary arteries from parasternal short axis which allows to see the left coronary artery origin, left anterior descending artery and left circumflex artery, as well as the right coronary artery (Figure 1, 2).
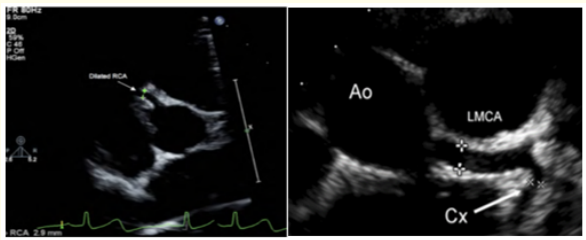
Figure 1: Short axis view showed in the left: dilated right coronary artery, in the right: dilated left coronary artery.
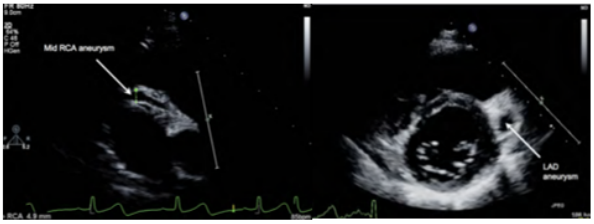
Figure 2: Short axis view showed in the left: right coronary artery aneurysm, in the Right: left coronary artery aneurysm.
The recommendations are to perform echocardiography at diagnosis, then after 2 weeks and repeating at 6-8 weeks after the onset of clinical features for uncomplicated cases.
The baseline study should be done at diagnosis for left ventricular function, coronary arterial lesions, valvar involvement, myocardial and/or pericardial involvement.
If there is any cardiac involvement closer follow up is required.
When the coronary aneurysms > 5mm this will elevate risk of developing stenotic coronaries so it will require close monitoring.
Transient cardiac involvement is likely to have resolved by 6 to 8 weeks, or if coronary artery dilation and/or aneurysms are present, the maximum diameter is usually reached by 6 to 8 weeks also, because that we do follow up Echo at this time.
Coronary artery lesions are perivascular brightness, dilatation, aneurysm formation, and lack of tapering of the distal coronary vessel (Figure 1, 2).
Aneurysms forms: (Figure 3)
Fusiform (spindle-shaped),
Saccular (spherical),
Ectatic (uniformly dilated long segment) or
Segmented (multiple dilatations joined by normal or stenotic areas)
*classification was first published in 1984. Aneurysms according to internal diameter are considered to be
Small if <5mm,
Medium if between 5-8mm,
Giant if >8mm.
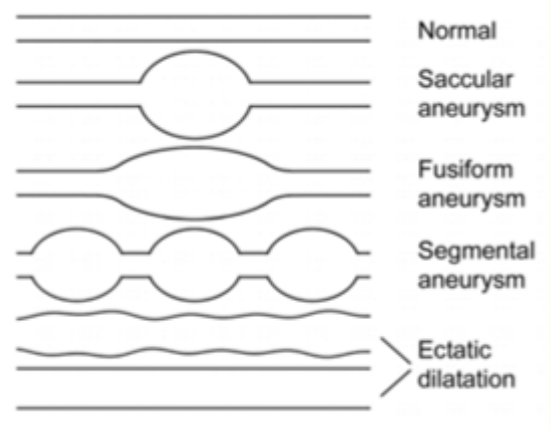
Figure 3: Coronary artery abnormalities.
Coronary artery imaging difficulties increases with age, so other imaging options may be used like resonance imaging and multi detector computed tomography. Especially that echocardiography has its limitations in diagnosis of stenosis and thrombosis.
Cardiac stress testing may be used to identify reversible ischemia and regional wall motion abnormalities during increased demand.
Coronary perfusion abnormalities can be further assessed with exercise echocardiography, pharmacologic (dobutamine, dipyridamole or adenosine) stress echocardiography and exercise myocardial perfusion scans.
Cardiac catheterization with selective coronary angiography is considered the gold standard for delineation of coronary artery anatomy, and if required interventional procedures such balloon angioplasty, stent placement or percutaneous transluminal coronary revascularization may be performed in the same setting.
Cardiac catheterization is usually recommended for patients with complex coronary artery lesions however it can provide useful detailed information and help with risk stratification but with mild coronary artery lesion it is not recommended.
Coronary angiography in this instance is recommended 6-12 months after the onset of Kawasaki disease, or sooner as clinically indicated [1-9].
Treatment
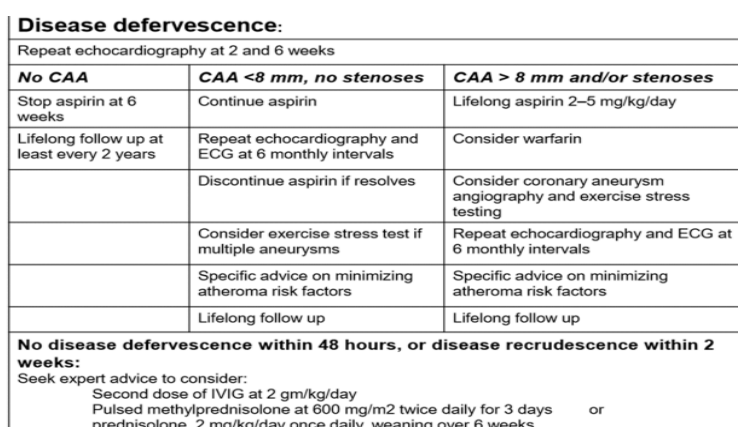
Table 1: Treatment and follow up according to the coronary arteries involvements.
Risk stratification (Table 2)
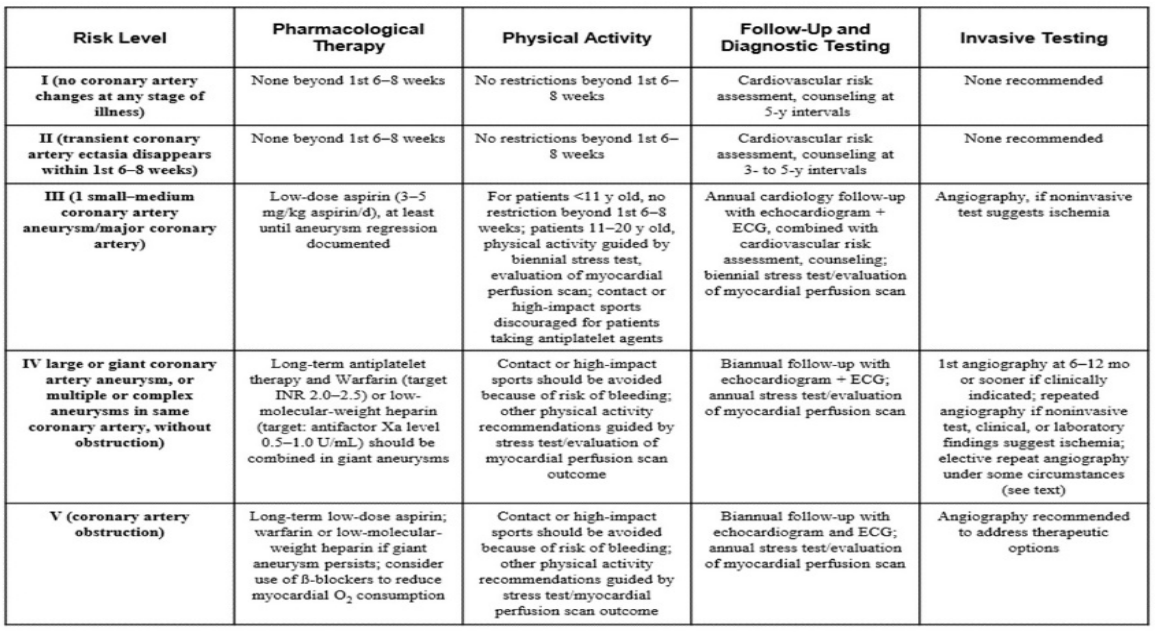
Table 2
Copyright: © 2019 Samah Alasrawi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.