K Fathi and F Harangi*
Department of Pediatrics, Balassa Janos County Hospital, Szekszard, Hungary
*Corresponding Author: K Fathi, Consultant Pediatric Surgeon, Department of Pediatrics, Balassa Janos County Hospital, Szekszard, Hungary.
Received: August 08, 2019; Published: September 13, 2019
Citation: K Fathi and F Harangi. “Bilateral Simultaneous Testicular Torsion in a 17-Year-Old Boy: Case Report and Review of Literature”. Acta Scientific Paediatrics 2.10 (2019):44-46.
Bilateral testicular torsion in adolescent is a rare condition, it is more frequent in neonate. Herein we describe a case of 17-yearold boy presented with sudden onset of left testicular pain of 1-hour duration. Left testicular torsion was diagnosed by physical examination and confirmed by testicular Doppler ultrasound. Right testis was asymptomatic with normal Doppler ultrasound findings. Surgical exploration of both testes showed salvageable left testicular torsion and torsion of right testis. Bilateral untwisting and orchidopexy performed. Although the occurrence of bilateral testicular torsion in adolescence is rare, as this case demonstrates, it can happen simultaneously without initial symptoms. Therefore, bilateral scrotal exploration and orchidopexy is mandatory in unilateral testicular torsion.
Keywords: Bilateral Testicular Torsion; Synchronous; Spermatic Cord; Adolescent
Testicular torsion is an acute vascular event in which the testis is twisted around its spermatic cord causing ischemia to the testis. It is most common genitourinary tract emergency in children requiring urgent surgery. Bilateral testicular torsion is more common in neonates, however, in adolescent it occurs rarely, only five cases have been reported in the literature [1].
A 17-year-old boy presented with 1-hour history of severe left hemi-scrotal pain, radiating to left groin and nausea. The pain started during sleep and he did not have any sport injury or trauma. Physical examination revealed pale patient, left testicle was positioned higher than the right side, lying obliquely, extremely tender and mildly enlarged. The right testicle was of normal size and non-tender. There was negative cremasteric reflex on the left side (Figure 1). Emergency Doppler ultrasound scan showed no intratesticular colour flow (circulation) in the left testicle. The left epididymis was grossly thickened with moderate left scrotal hydrocele. Colour flow was seen in right testicle and epididymis. Emergency left hemi-scrotum exploration showed dusky left testicle with 720⁰ clockwise torsion of the spermatic cord. Following untwisting of testis, its circulation improved and recovered (Figure 2). Then the right hemi-scrotal exploration was performed, which revealed 180⁰ clockwise torsion with normal coloured testicle (Figure 3). The testis was untwisted and bilateral orchidopexy performed. Ten months following bilateral orchidopexy, Doppler ultrasound examination showed that both testicles are of normal, equal volume and normal circulation and echogenicity (Figure 4).

Figure 1: Left testis is located higher due to torsion.

Figure 2: a. Left testis with 720⁰ torsion. b. after untwisting, left testis circulation and coloration recovered.

Figure 3: In asymptomatic right testis 180⁰ twist was noted.
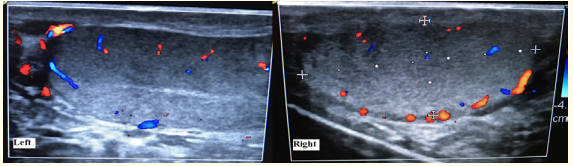
Figure 4: Doppler ultrasound of left and right testicle 10 months post-torsion, normal circulation noted.
Bilateral simultaneous testicular torsion in adolescent is very rare, only five cases have been reported in the literature [2-6]. It is more common in neonates, synchronous bilateral neonatal testicular torsion counts for 11-21% of all reported neonatal testicular torsions [7-12]. There are two types of testicular torsion, namely extravaginal torsion occurs in neonates, and intravaginal torsion particularly seen in adolescent with the peak incidence of 14 years of age [13]. The etiology of extravaginal torsion is due to flimsy or lack of attachment of tunica vaginalis to the scrotal wall, which allows free movement of testis around spermatic cord commonly seen in neonates. This also suggest the higher incidence of bilateral testicular torsion in neonatal age [2]. Intravaginal torsion on the other hand, occurs in adolescent due to loose attachment of tunica of appendix testes. Sixty nine percent of cases present within 12 hours of onset of torsion [14]. The testis lies higher, with oblique or transverse position and absence of cremasteric reflex [15]. Accompanying gastrointestinal and abdominal symptoms such as nausea, vomiting, lower quadrant abdominal pain have been noted. Occasionally patients with right lower quadrant abdominal pain referred with suspected appendicitis, turned out to have an acute right testicular torsion. Therefore testicular examination of all boys presenting with lower quadrant abdominal pain should be part of physical examination, in order to avoid missed testicular torsion. Doppler ultrasound scan is a good diagnostic tool, permits any vascular and echogenicity changes of the testis, with sensitivity of 63.6-100% and specificity of 97-100% [16]. However early on the testicular torsion might not show any ultrasonographical changes. As in our case, the right testis was asymptomatic and Doppler ultrasound showed normal vascularity of the testis. This case demonstrates that initial scrotal examination and Doppler ultrasound scan are unreliable tolls and can be misleading in the diagnosis of bilateral synchronous testicular torsion. The time elapsed from the onset of symptoms until the exploration and the degree of cord twisting are the most crucial factor in the degree of damage to the testicle. Some authors reported severely damaged, non-salvageable testicles after 24 hours of duration and more than 360⁰ of twist [17-19]. Therefore, when testicular torsion is suspected, there should be least delay in diagnostic work-up as the time is tickling and further delay increases ischemic and irreversible damage to the testicle. Manual detorsion of the testis by outwards rotation of the testis under Doppler ultrasound guidance should be done to relief pain and improve testicular circulation followed by urgent bilateral orchidopexy [20].
Bilateral testicular torsion is extremely rare, mostly seen in neonates, but may also occur in adolescents or adults. Emergency bilateral hemi-scrotal exploration is mandatory in patients presenting with acute unilateral scrotal pain, to avoid missing contralateral asymptomatic testicular torsion.
Copyright: © 2019 K Fathi and F Harangi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.