Mohammed J Aboud*
Consultant Pediatric Surgery, Pediatric Surgery Unit, The Maternity and Child Teaching Hospital, Al Diwaniya, Iraq
*Corresponding Author: Mohammed J Aboud, Consultant Pediatric Surgery, Pediatric Surgery Unit, The Maternity and Child Teaching Hospital, Al Diwaniya, Iraq.
Received: August 09, 2019; Published: August 30, 2019
Citation: Mohammed J Aboud. “Vaginal Parts of Sarcoma Botryoides in Children: A Case Report”. Acta Scientific Paediatrics 2.9 (2019):100-104.
Introduction: Genital and Gynecologic tumors in children are rare and represent less than 5% of all pediatric neoplasms. Vaginal parts of these tumors can have a spectrum and variable clinical presentation. Rhabdomyosarcoma (RMS) is considered the most common soft-tissue sarcoma found in children. We present a case of Sarcoma botryoides to illustrate the difficulties encountered by pediatric surgeons in the management of this malignant and aggressive tumor.
Case Report: A 3 years old girl presented to our pediatric surgery clinic with 2-months history of a protruding mass from her vaginal orifice. The patient was arranged for surgery, where an en-bloc dissection of the total mass was done. A classic histologic findings in sarcoma botryoides were confirmed.
Conclusion: All parents and concerned health workers should take care on finding a protruding mass in the genitourinary tract of their child and they should bring the child to medical attention, this can enhance the early diagnosis and better prognosis.
Keywords: Case Report; Vagina; Sarcoma; Children
Genital and Gynecologic tumors in children are rare and represent less than 5% of all pediatric neoplasms [1]. Vaginal parts of these tumors can have a spectrum and variable clinical presentation, including abdominal pain, abdominal mass, chronic genital ulcer, bloody discharge or tissue protruding from the vaginal orifice [2]. Rhabdomyosarcoma (RMS) is considered the most common soft-tissue sarcoma found in children, with approximately 20% of all RMSs found in the genitourinary tract. It is the most common soft tissue sarcoma in childhood and young adulthood, and account for 4-6% of all malignancies in this age group [1]. The tumors also occurs rarely in the cervix or uterine fundus and often is described in other term as "cluster of grapes”[3]. The survival rate of vaginal and cervical lesions has been reported to be 60-96%, respectively [4]. Vaginal bleeding is the most common presenting feature even though non-specific [5].
It may also present as a polypoid or fleshy mass in the vagina, or more classically projecting from the introitus. Urinary symptoms are the other forms of presentations especially when the tumor is anteriorly situated or tenesmus where there is posterior extension [6]. The management of pediatric vaginal tumors has evolved from radical surgery to the neo adjuvant chemotherapy followed by local control with surgery or radiotherapy in the last decades [7]. Radical surgery is the cornerstone of the treatment, as the disease is uniformly fatal with a five-year survival rate of between 10-35% [8]. Sarcoma botryoides has been reported with marked tendency for recurrence locally after excision and to invade adjacent organs [9].
We present a case of Sarcoma botryoides to illustrate the difficulties encountered by pediatric surgeons in the management of this malignant and aggressive tumor.
Written informed consent was obtained from the patients' parent who participated and managed in this report for publication of both cases and any accompanying images. The scientific and health committee in our Health directorate office approved this publication.
A 3 years old girl presented to our pediatric surgery clinic with 2-months history of a protruding mass from her vagina orifice. The mass began as a small noticeable round nodule in her vagina that rapidly increased in size. The mother stated that her daughter has had white, foul-smelling vaginal discharge with occasional streaks of blood on her diaper. The mother also described redness of the skin immediately surrounding the mass. The patient has normal urine output and urinary frequency without any evidence of discomfort during urination, and there is no hematuria. There have been no fevers or weight loss, although she has had a decreased appetite for 15 days.
Physical examination revealed an alert; well-appearing child in no acute distress and the patient was pale. Vital signs are normal for age, and her weight, height, and head circumference are at the 25th percentile. Abdominal examination revealed a soft, non-tender abdomen, no hepatosplenomegaly or palpable masses. Multiple bilateral inguinal lymph nodes are detected, most prominently in the left inguinal region, where the largest node is fixed and approximately 1 cm in diameter. No cervical or axillary lymphadenopathy is noted. Genital examination revealed a large, grapelike mass filling the vaginal vault (Figure 1, A-C). Streaks and tinges of blood with some white discharge are noted on the diaper. The urethra cannot be seen or distinguished from the mass. Overlying erythema of the labia and surrounding skin is noted with some excoriations on the surrounding skin. A mass was palpable anteriorly on rectal examination. Radiological studies, ultrasound showed a heterogeneous mass measuring 5x7 cm occupying the vagina. Pelvic computerized tomographic scan (CT) with contrast revealed a solid, cystic mass 5x6.5x6 cm, located anterior to the rectum, and at the posterior-superior aspect of the bladder (Figure 2, A-C). There was no calcification or retroperitoneal lymphadenopathy. The study did not reveal any extension of the tumor beyond the vagina.
Initial laboratory findings revealed a white blood cell count of 19.600/mm3, hemoglobin of 9.8 g/dL, erythrocyte sedimentation rate was 45 mm/hr. Serum electrolyte and blood urea nitrogen values are normal. Liver function tests were normal. Serum alphafetoprotein (AFP) was highly elevated (6400 KIU/L), B-human chorionic gonadotropin (B-HCG) was normal.
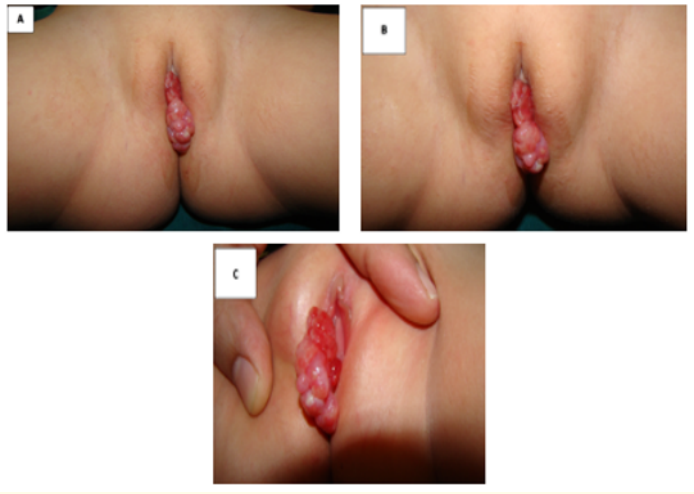
Figure 1A-C: A large, grapelike mass filling the vaginal vault. The urethra cannot be seen or distinguished from the mass.
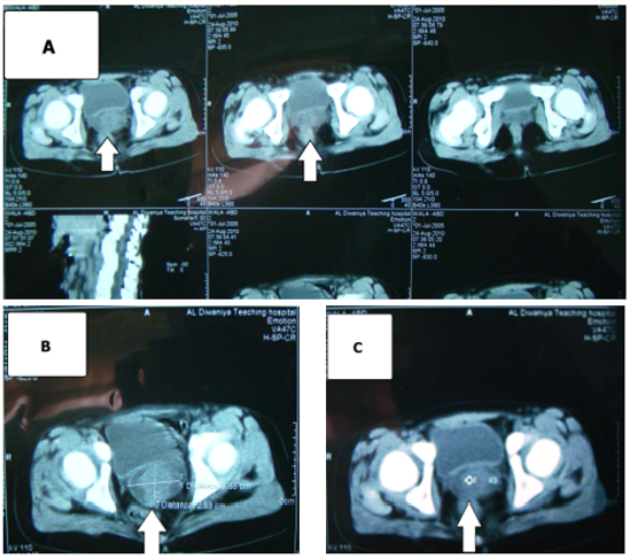
Figure 2A-C: Pelvic computerized tomographic scan (CT) with contrast revealed a solid, cystic mass 5x6.5x6 cm, located anterior to the rectum, and at the posterior-superior aspect of the bladder (arrowed).
The patient was arranged for surgery, where an en-bloc dissection of the total mass was done. The tumor was arising from the superior part of the vagina (Figure 3, A, B). Uterus and cervix were free of tumor, and there was no infiltration into the bladder and rectum. Gross appearance of the tumor was that of a pale tan-yellow slimy tumor with foci of necrosis. Microscopically, the biopsy findings demonstrating a rhabdoid cell with irregular nuclear contour, increased eosinophilic cytoplasm and submucosal zone with increased tumor cellularity. A classic histologic findings in sarcoma botryoides were confirmed. According the Clinical Groups staging, stage 2 was submitted (figure 4). The patient had a smooth postoperative recovery and she was referred to the oncologist for further management including combination chemotherapy. She received 8 cycles of neoadjuvant chemotherapy (Vincristine, Dactinomycin and Cyclophosphamide). Follow-up visits were arranged with AFP level estimation and CT scan, a repeat CT for post-treatment evaluation showed no evidence of recurrence at the surgical site or distant metastasis.

Figure 3A-B: Perioperative images where an en-bloc dissection of the total mass was done through a vaginal approach. The tumor was arising from the superior part of the vagina.
One of the most common problems presenting to a pediatric gynecologist are those involving the vulvo vagina. About 7 weeks before the development of an embryo, cells called rhabdomyoblasts which will eventually form skeletal muscles, begin to form. These cells can develop into RMS. Because this is a cancer of embryonal cells, it is much more common in children, although it does sometimes occur in adults [10]. The vast majority of cases occur sporadically with no recognized predisposing risk factors, although in a small proportion of the cases there may be a genetic link between cervical RMS and other primary tumors; most notably Sertoli–Leydig tumor [11]. There are 2 main types of RMS, along with some less common types; first, embryonal rhabdomyosarcoma (ERMS) usually affects children in their first 5 years of life, but it is the most common type of RMS at all ages. The cells of ERMS look like the developing muscle cells of a 6- to the 8-week-old embryo. This tumor tends to occur in the head and neck area, bladder, vagina, or in or around the prostate and testicles. Two subtypes of ERMS, botryoid, and spindle cell rhabdomyosarcomas tend to have a better prognosis (outlook) than the more common conventional form of ERMS. Second, Alveolar rhabdomyosarcoma (ARMS) typically affects all age groups equally. It makes up a larger portion of RMS in older children and teens than in younger children (because ERMS is less common at older ages) [12,13]. ARMS most often occurs in large muscles of the trunk, arms, and legs. In one report, large scale study for patients with rhabdomyosarcoma stated that the site of origin was paratesticular in 35%, bladder in 25%, prostate in 24%, vagina in 7%, and other sites, including cervix, vagina, and vulva, in 8% [14]. The cells of ARMS look like the normal muscle cells seen in a 10-week-old fetus. ARMS tends to grow faster than ERMS and usually requires more intense treatment. Anaplastic rhabdomyosarcoma (formerly called pleomorphic rhabdomyosarcoma) is an uncommon type that occurs in adults but is very rare in children [12]. Many authors recommended that any polypoidal mass found in a child be regarded as botryoid RMS unless proven otherwise [3]. Common presenting features of sarcoma botryoides include a vaginal or urethral mass, non-menstrual vaginal bleeding, urinary retention, and a foul-smelling discharge from the genital region. Initial misdiagnosis of sexual abuse can occur, especially when vaginal bleeding is present and a protruding mass is not yet obvious. Common sites for metastatic rhabdomyosarcomas include the lungs, bones, and regional lymph nodes. The diagnosis of sarcoma botryoides is based primarily on biopsy of the protruding mass. Staging for sarcoma botryoides includes computed tomography (CT) scan or (MRI) of the chest and abdomen, a bone scan, and bilateral bone marrow biopsies. Any suspicious lymph nodes found on physical examination also should be biopsied for proper disease staging because the presence of diseased lymph nodes alters the treatment protocol [15].
The role of histopathology in the diagnosis of RMS cannot be underestimated and it is the gold standard test in the diagnosis. Although three varieties of RMS have been described (Embryonal, Alveolar and Undifferentiated), the embryonal type is the most common and has a favorable prognosis, whereas the alveolar type is rare with a poor prognosis. Embryonal RMS of the cervix must be distinguished pathologically from adenosarcomas, malignant mixed Müllerian tumors and low-grade stromal sarcomas as the optimal management strategies and clinical outcomes differ for each [11]. The clinical group is based on the extent of the disease and how completely it is removed during initial surgery [10]. Former opinions suggesting extensive surgery and radiation improve the dismal outcome in these young children are outdated. Due to balanced therapies: total excision of the mass, chemotherapy, and radiation adjusted to the tumor stage, cure of these sarcomas may be expected dependent on tumor stage, localization and response to chemotherapy [16]. Although ultra-radical surgery i.e. pelvic exenteration was considered the treatment of choice in the late 1960s, outcomes were often unsatisfactory. In the past years, limited surgery with adjuvant chemotherapy and/or irradiation showed improved survival [17]. In Sweden, pediatric RMS showed a higher rate of metastatic disease, this might explain the decreased trend in overall survival in the last decade. However, the reason for the higher frequency of metastasis remains unclear and it would be of great interest to find out more about underlying causes [18]. We must consider other differential diagnosis of sarcoma botryoides includes other malignant tumors, such as germ cell tumors of the vagina and clear cell sarcoma. Nonmalignant entities included in the differential diagnosis include a prolapsed urethra, paraurethral cyst, ureterocele, hydrocolpos, genital warts, and condylomata acuminata [19].
It is important to know that the exact pathology of such an uncommon lesion in that site and its clinical implications are important to avoid inaccurate and subsequently mismanagement. All parents should take care on finding a protruding mass in the genitourinary tract of their child and they should bring the child to medical attention, this can enhance the early diagnosis and better prognosis. Accordingly, many authors concluded that this tumor has good prognosis due to early presentation, slow progression and the prognosis of patients treated with multimodal therapy is very good.
The author expresses sincere gratitude to all the pediatric surgery unit staff and all the colleagues in the radiology unit at the Maternity and Child Teaching Hospital, Al¬ Qadisiya, Iraq, for their assistance.
The authors declare that they have no competing interests.
Copyright: © 2019 Mohammed J Aboud. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.