Parveen Kumar1*, Vivek Vishwanathan2, and Rishabh Jain2
1 Assistant Professor, Department of Pediatric Surgery, Chacha Nehru Bal Chikitsalya, New Delhi, India
2
DNB Resident, Department of Pediatric Surgery, Chacha Nehru Bal Chikitsalya, New Delhi, India
*Corresponding Author: Parveen Kumar, Assistant Professor, Department of Pediatric Surgery, Chacha Nehru Bal Chikitsalya, New Delhi, India.
Received: July 22, 2019; Published: August 13, 2019
Citation: Parveen Kumar., et al. “Neonatal Abdomen: Pandora’s Box”. Acta Scientific Paediatrics 2.9 (2019):16-19.
Neonatal abdomen is truly called Pandora’s Box as it defies varies radiological investigations and reveals itself at the time of surgery. We present here three cases of neonatal surgical abdomen, which revealed true picture only at laparotomy.
Introduction: Abdomen is usually called as Pandora’s Box because of presence of various organs and complexed mechanism of their function. This get more so emphasized that these organs are still evolving in their structure and function in a neonate, who has been just separated from maternal world. We would like to take you through journey of three cases of surgical neonatal abdomen.
Keywords: Duplication Cyst; Meconium Cyst; Neonate
A 3-day-old male baby born at 35 weeks of gestation, with birth weight 2.7 kg normal vaginal delivery at a private local hospital. Antenatally one ultrasound scan was done at 32 weeks of gestation, which showed hydrops fetalis and polyhydramnios. Amniotic fluid index was 26.3 cm with fetal pleural effusions. At birth, baby had abdomen distension but cried immediately after birth. Baby passed urine in 24 hours of life. In view of antenatal scan findings and abdomen distension, baby was referred to other private center, where ascitic fluid tapping was done in view of increasing distension and respiratory distress. Baby was referred to us for further management. At presentation to us, baby was tachypneic (RR 37/ min), tachycardia (HR 163/min), capillary refill time was delayed (4 seconds). Baby was maintaining saturation of 96 % on room air. The abdomen was tense distended with clear air fields. After initial resuscitation, an infantogram was done, which showed air under diaphragm and centralized bowel loops (Figure 1). Ascitic fluid analysis (done outside) report was sought and showed 800 cells/cmm with 80 % polymorphs and proteins 3.1 g/dl. Other routine investigations included Hb 12g%, total leucocytes 17900/cmm with 46 %polymorphs and 50 % lymphocytes, platelets 1.1 lakhs/ cmm and C-reactive proteins of 59. Serum creatinine was 0.8 mg/dl with normal urea and electrolytes. Baby was taken for exploratory laparotomy and revealed meconium cyst like picture. Whole bowel with part of liver was encased in a sac like structure, which after removal of sac showed patent proximal bowel ending into cystic mass in distal ileum. Large bowel was healthy. The mass was resected and divided ileostomy was made. The histopathological examination revealed it to be duplication cyst. Distal stoma wash outs were started after 2 weeks and stoma reversed at 8 weeks. Patient is doing well in follow up and gaining weight.

Figure 1
A full term normally delivered male neonate was brought to our tertiary care center on day 6 of life, with complaints of generalized abdominal distension, bilious vomiting and refusal to feeds. Baby had increased respiratory rates since one day and history of nonpassage of meconium since birth. The baby was being managed at a private clinic with the diagnosis of sepsis with intestinal obstruction and then referred to us for further management. Blood counts revealed neutrophilic leukocytosis and a raised serum c-reactive protein. X ray abdomen showed a picture of intestinal obstruction and a large air fluid level with signs of antenatal calcification in left iliac fossa (Figure 2). The baby was taken for exploratory laparotomy after due stabilization. Intraoperatively there was a volvulus of the caecum and ascending colon, which was gangrenous and was blind ending in the shape of a pouch (Figure 3). This segment also had a perforation in it. The transverse colon was atretic and the large bowel starting again from the splenic flexure was collapsed. An end ileostomy and a transverse colon mucus fistula were made after resection of the gangrenous intestinal segment. Baby is doing well in follow up with regular washouts and is planned for stoma closure.
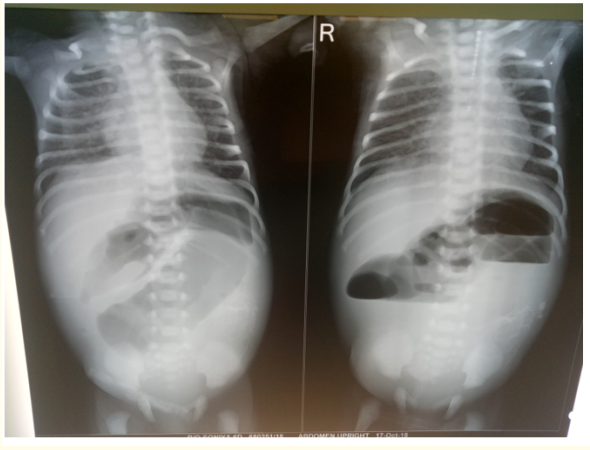
Figure 2

Figure 3
A 4-days-old female baby, full term brought to us with complaints of abdominal distension, bilious vomiting since birth. Baby had passed scant amount of meconium on day 1 of life. There were no antenatal scans and visits done. At presentation, baby had tachycardia (HR 156/min), tachypnea (RR 34/min) and delayed CFT. The abdomen was distended with sluggish bowel sounds and naso-gastric aspirates had bilious content. X-Ray abdomen revealed centrally placed bowel loops with tell-tale signs of antenatal event suggested by multiple calcifications in whole abdomen (Figure 4). After initial resuscitation, baby was taken for exploratory laparotomy and revealed distal ileal and cecal volvulus, densely adhered to left lower abdominal wall. The findings were representative of antenatal volvulus (Figure 5). The volvulus part was excised and distal ileostomy and transverse colostomy was made. Baby is gaining weight and is on regular distal wash outs in follow up.
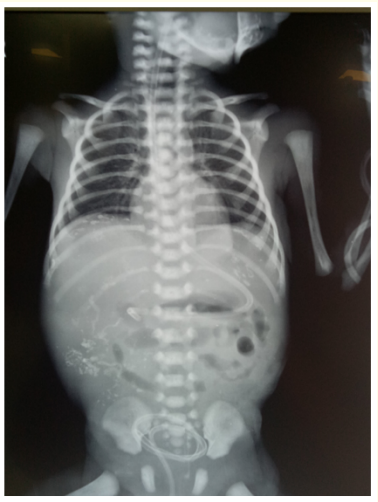
Figure 4

Figure 5
The abdominal cocoon is extremely rare condition reported in neonates [1]. It is usually acquired or may be idiopathic. The fibrocollagenous sac like structure is usually secondary to chronic inflammatory reaction. Congenital etiology states that it may be derived from yolk sac or omentum antenatally [2]. Wei., et al. proposed three types of abdominal cocoon depending on structures covered by sac [3]. In type I, part of small intestine while in type II small and large bowel is covered by sac. In type III, sac covers viscera along with whole bowel. It was type III cocoon in our case 1.
The duplication cysts are rare malformations of alimentary tract (from mouth to anus) more commonly involving ileum. They may or may not communicate with main bowel lumen and may have varied presentation including infection, bleeding, inflammation, torsion or perforation. The evidence of gas under diaphragm in our case 1 may be secondary to ascitic fluid tapping (done outside) or any antenatal event. To hypothesize post-natal perforation is very unlikely as duplication cyst had small bowel mucosa and not ectopic mucosa. The surgical excision is curative.
With the advance of medical sciences and antenatal imaging techniques, it is now possible to diagnose many conditions in prenatal period itself. The meconium peritonitis is rare but one of the conditions, which may be very well diagnosed on expert antenatal scanning. The incidence is 1 in 30,000 live births [4]. It may be secondary to bowel atresias, volvulus, intussusception, bands or imperforate anus. The presence of calcifications on X-rays of case 2 and 3 were indirect evidence of antenatal meconium contamination secondary to volvulus and perforation. The perforation site may have been plugged by omentum later.
The antenatal imaging findings on ultrasonography may include ascites, echogenic or dilated bowel, polyhydramnios and calcifications [4]. The findings of ascites and polyhydramnios were present in case 1 but other two did not have any antenatal scans done. The major risk factors of mortality in meconium peritonitis are sepsis and low birth weight [4,5]. We were able to salvage all the three cases with early and timely surgical intervention. However, learning points may be numbered as: 1. Antenatal scanning is must in all pregnancies. It could have brought case 2 and 3 more early to us and plan timely intervention. 2. Early detection of meconium peritonitis carries good outcome with timely surgery and current health care.
Neonatal abdomen is true Pandora’s box. We need to be vigilant about rare surgical emergencies as they may carry good outcome with present day health care.
Copyright: © 2019 Parveen Kumar., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.