AS Ibama1*, INS Dozie1, OC Abanobi1, AN Amadi1, G Iwuoha1, CR Nwufo1, SN Ibe1, OG Udujih1, T Jaja2 and P Dennis3
1Federal University of Technology, Owerri, Nigeria
2University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria
3Rivers State Primary Health Care Management Board, Port Harcourt, Nigeria
*Corresponding Author: AS Ibama, Federal University of Technology, Owerri, Nigeria.
Received: June 24, 2019; Published: July 30, 2019
Citation: Sangita D Kamath., et al. “A Case Report on Choroidal Metastases from Adenocarcinoma of Lung – Tip of the Iceberg!”. Acta Scientific Paediatrics 2.8 (2019):00-00.
Studies indicated that, Effective host defense of the respiratory tract against pathogens is based on interaction of different antibodies, complement, neutrophils or other phagocytic cells. Studies had also associated higher incidences of respiratory infection among children to none immunization. The aim was to ascertain if there exists any pattern of relationship between risk of acute respiratory infection (ARI) among infants and immunization status per age. The study design was community-based Nested casecontrol study undertaken on randomly selected 1,100 infants in 12 communities from 6 Local Government Areas of the 3 senatorial districts of Rivers State. The subjects were selected via multistage random sampling technique up to the community level. The characteristics of the subjects were represented using descriptive method while logistic regression at 5% level of significance, applied in testing the disparities in ARI between none immunization and complete immunization status among infants. Measures of size effect of ARI on immunization status disparities was interpreted using odds ratio (OR). More cases of ARI were found among infants with none immunization status (15.4%) in rural communities than in urban communities (11.2%). In all, infants with none immunization status, had higher frequency of 32.3% in occurrence of ARI, against 19.4% for complete immunization status. For the infants with none immunization status, the odds for ARI (unadjusted) were about 2times higher in significance when compared with those infants with complete immunization status (OR = 1.97, p< 0.0001, 95%CI=1.495-2.604), while the odds for ARI (adjusted), found to be a significant risk, lower on the immunized children by 50% (OR = 0.5, p < 0.0001, 95%CI = 0.368 – 0.689) against the unimmunized ones. This evidence of pattern of relationship between risk of ARI among infants and immunization status per age is quite outstanding to herness the benefits of timely vaccinations to achieving the prevention and control of ARI. Routine immunization activities should be strengthened through aggressive and consistent outreach/home-based services as a deliberate effort in reducing risk of ARI among infants.
Keywords: Immunization Status Per Age; Acute Respiratory Infection; Pattern; Rural; Urban; Community; Vaccines; Case-Control
Immunization as a concept is a method and practice concerning the activation and or maintenance of the body immune system over time. Immunity is the key entity in disease prevention which immunization as a health care delivery strategy and practice is designed to achieve.
The researchers, having perceived the poor attitude of mothers/ caregivers towards vaccination/immunization of their children, thereby making a lot more children not fully immunized to derive benefits of adequate immune responses gotten from active immunization activities, seek to know to what extent none or partial uptake of vaccines per age among infants is implicated in the pattern and risk of acute respiratory infection. It is without doubt, from epidemiological point of view that sustained timely activation of the immune system via type specific vaccination for adequate response to antigens (specific pathogens) is fundamental in breaking the chain of transmission of implicated diseases in the community through herd immunity. It is quite obvious and understandable in public health practice that; improvements in hygiene and sanitation only control certain infections, population change can affect sanitary measures, some infections are only controlled by changing individual behaviour, emerging infections will not be controlled by sanitary changes alone, some modern lifestyle changes increase infection risk, pathogens may undergo mutation to resist our control/ management programmes, our defence systems cannot always prevent or eliminate pathogenic microbes [1]. Unless we can achieve total elimination of vaccine-preventable diseases, we have to continue immunizing until such diseases are eliminated or eradicated.
In the study of [2], clinical manifestation of ARI among children is with any one or combination of symptoms and signs like cough and cold, running or blocked nose, stops feeding and or drinking, sore throat, fast breathing, noisily breathing, chest-wall retraction etc.
Pattern, epidemiologically denotes the occurrence of healthrelated event by time, place and person… place pattern may be geographic variation, urban/rural differences… The health-related event in this context being, occurrence of ARI. The risk in our present discuss refers to the chances of an infant contracting ARI by virtue of immunization/vaccination status per age.
Research work had shown that, innate immune response affords the first line of defense against infection. In this regard, it had been estimated that the innate immune system provides protection against 98% of encountered pathogens [3].
According, to [4,5], effectual host defense of the respiratory tract against pathogens is a function of the interaction of specific type of antibodies, complement, neutrophils even other phagocytic cells. When pathogens overpower these defenses and eventually enters the blood stream, systemic protection is mediated by anticapsular antibodies [6] and the essence of vaccination/immunization is to ensure activation of the immune system for the production of specific type of antibodies against specific disease-causing pathogens. Insufficient mucosal immune response may create the way for persistent and recurrent colonization and subsequent infection, while an efficient local immune response to the pathogen promotes elimination of colonization and prevention of re-colonization [7]. In a general analysis, [7] stated as thus, “the mucosal immune system develops faster than the systemic immune system, and functions from the age of 6 months”. Some diseases such as diphtheria, pertussis (whooping cough), and measles are vaccinepreventable diseases that may have a respiratory tract component but also affect other systems [8].
The work from West Tripura stated that the incidence of respiratory infection was higher among none immunized children [9]. Similarly, in Delhi study, inappropriate immunization for age was significantly related to ARI in under-five children [10]. A hospitalbased prospective study conducted in Kolkata found that none immunization was a significant risk factor for ARI [11].
The study by [12], revealed that immunization appears to be strongly associated with severity of ARI cases. This result was consistent with results found by [13], in Iraq and [10], in India. In the study conducted on ARI in Mysore, revealed that significant sociodemographic risk factors were overcrowding and partial immunization [14].
In a cross-sectional community-based study conducted in 21 registered urban slums of Guwahati in Assam, India to ascertain the prevalence and risk factors associated with ARI among 370 under-five children in 184 households and 370 families, within the period of 15th September to 30th December 2004, as revealed in the study of [2], showed that none immunized children had more chances of developing ARI (RR = 2.01). ARI cases, having complete immunization status were only 10%, while among the none immunized group were 57.5%. In this study, children classified as having complete primary immunization status were combined with those partially immunized and compared with none immunized children in ascertaining the risk of ARI in relation to immunization status.
In a cross-sectional study covering 500 under five children in urban (five zone) and rural (five PHC of Sanand Taluka) area of Ahmedabad district within the period covering September 2008 to March 2009, reported in the works of [15] showed direct correlation between immunization status of children and occurrence of ARI. It was least in children who were fully immunized (9.1%) as compared to unimmunized children (33.7%). This difference was statistically significant (x2= 33.87, p<0.001).
The study by [16], comprising 436 under-five children ARI cases in three hospitals in Enugu, Nigeria, poor immunization status was found to significantly contribute to the prevalence of ARI, with 50% of poorly immunized subjects having severe forms of ARI. This is consistent with previous reports [15,17].
It is therefore of concern to the researchers to ascertain the relationship of immunization status per age in the pattern and risk of acute respiratory infection among infants in Rivers State which may ensure specific emphasis in the design of programmes and policies aimed at strengthening routine immunization activities to enable children complete their uptake of vaccines per age before they attain their first birth day as a mark of commitment in the resolution of the problem posed by acute respiratory infection within the scope of the Sustainable Development Goals (SDG) 3, which duel on healthy lives and promotion of wellbeing for all at all ages.
The study aimed to ascertain if there exists any pattern of relationship between risk of acute respiratory infection (ARI) among infants and immunization status per age.
Null Hypothesis H0 – There is no relationship between pattern and risk of ARI and immunization status per age among infants in Rivers State, Nigeria.
Alternative Hypothesis H1- There is relationship between pattern and risk of ARI and immunization status per age among infants in Rivers State, Nigeria.
The study design was community-based prospective-retrospective (Nested) case – control method, aimed at ascertaining the pattern and risk of ARI among infants in relation to immunization status per age in the study areas.
The inclusion criteria for cases were children less than 12months of age in the study areas with at least any two of the signs and symptoms of cough, running nose or fever less than 3 days duration among others within 2weeks of enrollment/interview. While the inclusion criteria for controls were children less than 12months of age in the study areas without such signs and symptoms within 2weeks of enrollment/interview.
The exclusion criteria were removal of any case or control with difficulty in extracting complete information required for the study. See figure 1 for the schematic illustration of the design concept.

Figure 1 .
The study was conducted in 12 communities having either rural or urban settings, in 6 Local Government Areas (LGAs), out of 23 LGAs in the 3 senatorial districts in Rivers State, Nigeria. Rivers State, one of the 36 states in Nigeria has coordinates, latitudes 4051129.076111 and 4051.48461N, longitude 60 55115.288611 and 6055.25481E, [18], with Port Harcourt as the State capital. It occupies an area of about 37,000 square kilometers and bounded in the north by Imo and Abia States; in the south by the Atlantic Ocean; to the east by Akwa Ibom State and to the west by Bayelsa and Delta States. Table 1 showed the communities used as sampling points in the study.
The study population was children less than 12months in the study areas. The population of Nigeria was estimated to be at about 167 million (2006 census report) and children below 1year of age constitute 4% (6.6 million) of the total population [19].

Table 1: Communities used as Sampling Points for the Study in the LGAs.
In Nigeria and other developing countries 10-15 percent of all ARI may progress to disease of moderate to severe intensity [20], giving an estimate figure of such intensity to 29,040 to 43,560 cases annually with geographical zones and urban/rural settings variation.
The sample size for this study was based on [21] formula.
r + 1 (p*) (1-p*) (Zβ + Zα/2)2
Sample size = ………….. Eq 1
r (P1- P2)2
Where;
r = Ratio of Control to Case, 1 for equal number of Case and Control p* = Average proportion exposed = Proportion of Exposed Cases + Proportion of Control Exposed/2
Zβ = Standard normal variant for power = for 80% power it is 0.84 and for 90% power value is 1.26
Zα/2 = Standard normal variant for level of significance = 1.96
P1- P2 = Effect size or different proportion expected based on previous studies. P1 is proportion in cases and P2 is proportion in control.
Consequently, from Equation 1 and considering power of study of 80% (0.84), expected proportion in case group and control group to be 0.35 and 0.20 respectively and substituting values we have;
1+ 1 (0.275) (1-0.275) (0.84+ 1.96)2
Sample size =
1 (0.35-0.20)2
= 138.9
≈ 139 Cases and Control each gives a total of 278 at least.
For a matching power of 1:3, the minimum sample size required for this study is;
139 X 3 = 417 + 139 = 556 Cases and Controls.
Nevertheless, for a representative sample population for the study, the number was increased proportionally from the selected communities, giving 1,100 infants which are greater than 3% of the prevalence value considering the lower ARI prevalence rate of 10 percent, [20] that may progress to moderate to severe cases.
Figure 2 shows the schematic multi-stage procedures for simple random sampling and stratified sampling method in choosing the caregivers/infants of cases and the control group that participated in the study, it implies, every infant/caregiver of the population was given a chance of being selected.

Figure 2: Multi-stage simple random sampling procedures and Stratified sampling method.
A total of 1,100 infants comprising 275 cases and 825 controls (1:3) were picked proportionally, among the communities based on proportional allocation factor of 6:4 (660:440) for urban and rural communities for both cases and control, reflecting the size of study population of the communities, and a proportional allocation factor of 1:4.5:4.5 (100:500:500) for the age group of <2 months, 2months – 6months and 7months up to 12months. Figure 3 gives the summary of the study population in each sampling points/LGA.

Figure 3: Summary of Study Populationin in each Sampling Points/LGA.
The tool used for data collection was set of structured questionnaires. The items were based on demographic characteristics, knowledge and attitude of the target/study population concerning immunization status in the pattern and risk of ARI among infants. The questionnaire was reviewed for content validity. Pilot-testing for understanding of items by target/study population was undertaken, using 10 caregivers/infants who were not part of the sample used for the study.
The questionnaires were administered personally on the mothers/caregivers of the randomly selected infants for relevant information by the researcher with the help of recruited Community Health Practitioners after one-day training on the pattern of administration of the questionnaires and retrieved on the same day.
During the collection of data on ARI, mothers/caregivers were asked if their child under one (1) year of age had been ill with at least any 2 of the 3 signs and symptoms; cough, running nose or fever less than 3days duration within the 2weeks of enrollment/ interview. Those infants with such outcome attributes of ARI at any time during the 2weeks of interview were identified or defined as having ARI as cases.
Data from control group of the study was generated from matched study population to the cases of ARI from the same referent population using an uncontrollable variable (age), grouped as less than 2months, 2months – 6months, 7months up to 12months. Immunization status of study population was assessed as elicited by mothers/caregivers and verified by immunization card/record and categorized as fully immunized: a child who had received all vaccines according to national schedule as per his/her age at the time of interview, partially immunized: a child who had received some vaccines according to national schedule as per his/her age at the time of interview, and un-immunized: a child who had not received any vaccines according to national schedule as per his/ her age at the time of interview (See Table 2; Vaccine uptake schedule as per age according to National Immunization Programme). All of these go to ensure that the 5% chance of erroneously rejecting the null hypothesis was not increased when making comparism of study variable between cases and control groups of the study.
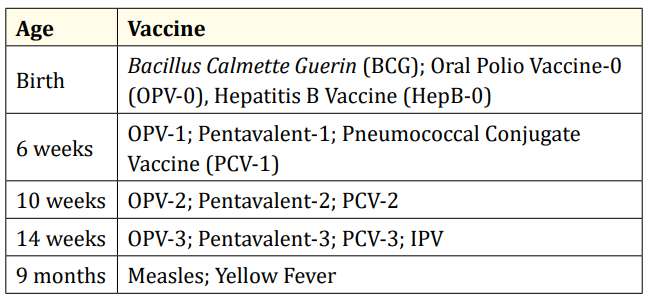
Table 2: Vaccine Uptake Schedule as per Age according to National Immunization Programme.
Note: OPV-0 and HepB-0 must be given before the age of 2weeks.
IPV - Inactivated Polio Vaccine
Data from responses were collated and presented in a tabular form with nominal scale, showing values for cases and non-cases (control) for the variable of study (immunization status). The entries were double checked for error of recording. Statistical analysis was performed using SPSS, version 21.0, to test the hypothesis for result at 5% significant level and also to show distribution of disparity in none immunization (none and some vaccines uptake per age) and immunized (all vaccines uptake per age) infants. Descriptive method was used to represent the characteristics of the subjects and the disparities in ARI between none immunized and immunized infants were tested in a bivariate and stepwise logistic regression at 5% level of significance. Odds ratio (OR) was used to interpret the measures of size effect of ARI from none immunized and immunized disparities.
The University of Port Harcourt Teaching Hospital Ethical Committee and the Research Ethics Group of the Centre for Medical Research and Training, College of Health Sciences, University of Port Harcourt gave the approval. Prior the interview, clear explanation on the nature and purpose of the study and level of participation of the mothers/caregivers and their infants were made and their informed consent sought. Participation was voluntary even after providing consent.
Figure 4 on distribution of demographic characteristics, showed that a total of one thousand, one hundred infants were studied, in which the age distributions revealed that majority 506 (46.0%) were within 2-6 months’ age bracket, against 491 (44.6%) within 7-11 months’ age group and 101 (9.2%) within less than 2months, whereas the age of 2(0.2%) were unknown so, excluded.
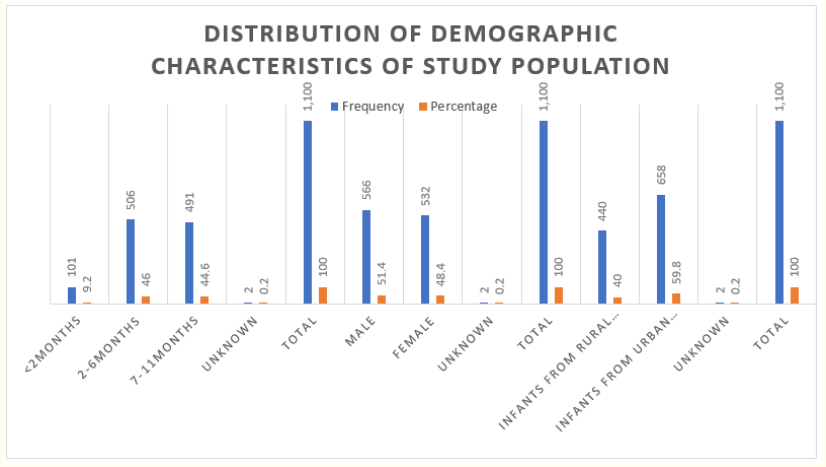
Figure 4: Distribution of Demographic Characteristics of Study Population.
The gender distribution showed that 566 (51.4%) were male infants, against 532 (48.4%) female infants.
The study area distribution indicated that 658 (59.8%) of the study population were from urban communities, against 440 (40.0%) study population who were from rural communities, while 2 (0.2%) of them were excluded, due to want of information.
The table 3, showed pattern of ARI and immunization status of the study population in rural communities (N=440), reflecting that, for the none immunization category (none and some vaccines uptake per age) N=191; n=64(33.5%) of the cases came under this category, against n=127(66.5%) of the controls who were also classified in the same category as at the two weeks of the interview/ enrollment for the study and so seen to having none immunization status.

Table 3: Pattern of Acute Respiratory Infection (ARI) and Immunization Status of Infants in Rural Communities.
For the category of immunized (all vaccines uptake per age) N=248; n=45(18.1%) of the cases came under this category, against, n=203(81.9%) of the control who were also classified under this category therefore, seen as having complete immunization status.
However, a case but no control infants from the rural communities fell under the category of unknown/indeterminate category.
Table 4, showed the pattern of ARI and immunization status among the infants from urban communities (N=660), in which for the none immunization category N=289; n=91(31.5%) of the cases were under this category, against n=198(68.5%) of the controls who were equally classified in the category within the period of the study and so classified as having none immunization status.

Table 4: Pattern of Acute Respiratory Infection (ARI) and Immunization Status of Infants in Urban Communities.
In the category of immunized N=365; n=74(20.3%) of the cases were immunized, against n=291(79.7%) of the controls who were also immunized and classified as having complete immunization status.
While, for the category of unknown/indeterminate N=6; n=6(100%) of the infants’ control status of immunization were unable to be determined, against none for the cases.
The evidences provided in tables 3 and 4 gave clear picture of existence of pattern relationship between ARI and immunization status among infants in rural (15.4% higher among none immunization status as categorized) and urban communities (11.2% higher among none immunization status as categorized) with a statistical difference of 4.2% higher in occurrence of ARI in Rural communities.
The table 5, reflecting pattern of acute respiratory infection in relation to immunization status of the study population (N=1,100), showed that, for the category of none immunization (none uptake of vaccine and some uptake of vaccines per age according to National Immunization Schedule) combined N=480; n=155(32.3%) were cases and so fell under that category and were classified as having none immunization status, against n=325(67.7%) of the controls who also came under that category and were equally classified as having none immunization status as at the two weeks of the interview/enrollment for the study.
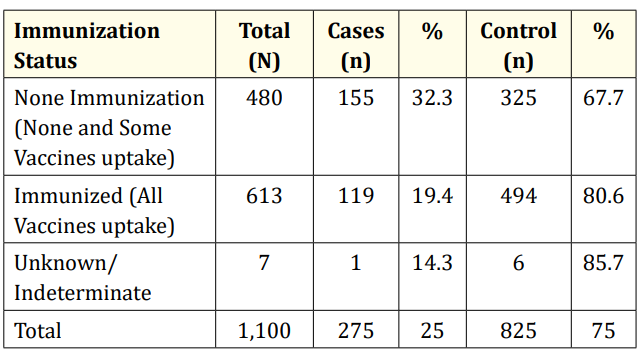
Table 5: Pattern of Acute Respiratory Infection (ARI) and Immunization Status of Study Population.
For the category of immunized (uptake of all vaccines per age according to National Immunization Schedule) N=613; n=494(80.6%) of the controls came under that category and were classified as having complete immunization status, against, n=119(19.4%) of the cases who also came under that category and were equally classified as having complete immunization status.
However, out of N=7; n=6(85.7%) of the infants’ control record of vaccine uptake, against n=1(14.3%) of the cases were difficult to ascertain for want of information.
Going by the evidence provided by the data in table 5, in which the cases presented a pattern relationship between immunization status (uptake of vaccines) and ARI, wherein infants with none immunization status, had higher frequency of 32.3% in occurrence of acute respiratory infection, against 19.4% for complete immunization status; thus one can adduce that a relationship between acute respiratory infection and immunization status among infants was observed to exist as determined in this study with a statistical difference in frequency of 12.9% in occurrence.
Data in table 6, reflects the relationship between acute respiratory infection and immunization status among the study population of this research work; in which out of N=480 infants with none and partial uptake of vaccines for their age according to national schedule for immunization, n=155 infants presented with signs and symptoms of acute respiratory infection as cases, against n=325 infants without signs and symptoms of acute respiratory infection as controls, within the 2weeks of interview/enrollment for the study.

Table 6: Relationship between Immunization Status and Acute Respiratory Infection (ARI) among Infants
Also, from total; N=613 infants who had completed their uptake of vaccines for the respective age according to national schedule for immunization, n=119 infants equally presented with signs and symptoms of acute respiratory infection as cases within the 2weeks of the interview/enrollment for the study, whereas n=494 infants were without signs and symptoms of ARI within the 2weeks of interview/enrollment for the study.
However, on subjection of the data as presented in table 6 to bivariate logistic regression analysis for odds ratio (unadjusted) to determine if there is relationship between risk of ARI among infants and immunization status in terms of none and partial uptake of vaccine per age combined and complete uptake of vaccine per age according to national immunization schedule, showed significant association or relationship between immunization status and acute respiratory infection OR-Unadjusted= 1.97≈ 2, (p < 0.0001, 95%CI=1.495-2.604), which implied that infants with none and partial immunization status per age according to national immunization schedule were about 2times at risk (OR=1.97) of contracting acute respiratory infection than infants with complete immunization status per age according to national immunization schedule.
Table 7 indicated the output from the stepwise logistic regression showing the adjusted results for cofounding effects, and it was found that immunization status of infants is a significant risk factor of ARI (p < 0.0001, 95%CI = 0.368 – 0.689). On the ARI cases, the unimmunized children are at higher risk of having the disease. The odds of the disease were found to be lower on the immunized children compared to that of the unimmunized ones by 50% (OR = 0.5).

Table 7: Logistic Regression (via Stepwise Method) with adjusted Odds Ratio for Immunization Status with ARI.
The ARI cases were found to be a little higher among infants with none immunization status (15.4%) in rural communities than infants with the same status in urban communities (11.2%). In overall, infants with none immunization status (none and partial uptake of vaccines per age), had higher frequency of 32.3% in occurrence of acute respiratory infection, against 19.4% for complete immunization status. For the infants with none immunization status, the odds for ARI (unadjusted) were about 2times higher in significance, compared to infants with complete immunization status (OR = 1.97, p<0.0001, 95% CI=1.495-2.604), while the odds for ARI (adjusted), found to be a significant risk, lower on the immunized children against the unimmunized ones by 50% (OR = 0.5, p < 0.0001, 95%CI = 0.368 – 0.689).
This finding, will therefore, consolidate awareness creation and enhance intensification of tracking of defaulting infants in view of immunization programme and so capable of contributing to improved coverage of immunization and herd immunity to preventing the transmission of implied pathogens in the communities.
Noting that earlier studies looked at association between ARI and none immunization and partial/complete immunization among children combined which in our consideration had masking effect of the problem in epidemiological point of view, the data in this study were collected, collated, and presented by bringing none and partial uptake of vaccine per age in one group and classified as none immunization status (unimmunized), and so more likely to contract acute respiratory infection in infancy; and uptake of all vaccines per age in the other group and classified as complete immunization status (immunized) and less likely to contract acute respiratory infection.
Subjecting the data to descriptive statistics and test of hypothesis analysis by bivariate and stepwise logistic regression statistical method against the null hypothesis at a significant level of 5% probability (∞ = 0.05) to determine the existence of any association between immunization status and acute respiratory infection among infants. The analysis reflected a relationship between pattern and risk of acute respiratory infection and immunization status among infants. Therefore, it may be stated that the proposed alternative hypothesis probably obtains and the pattern and risk of ARI is higher among infants with none or partial immunization status per age.
This is quite interesting, in that this result is consistent with documented body of knowledge regarding immunization status and pattern and risk of acute respiratory infection as reported by [9] [10][12][15][2] and [16], though studies were on under 5years children, including infants. The import of classification of none and partial immunization status as unimmunized as undertaken in this study in view of active immunization programme may be explained in terms of the mechanism of antibody production via primary and secondary responses after immunization/vaccination.
It had been reported that when vaccination is given and antigens (microorganisms) are encountered for the first time there is a primary response in which a low level of antibodies can be detected in the blood after about two (2) weeks. Although the response may be sufficient to overcome the antigen, the antibody levels then fall unless there is another encounter with the same antigen (vaccination) within a short period of time (say 4 weeks) for multiple doses vaccines. The second encounter produces a secondary response in which there is swift response by memory B-cells creating a marked increase in antibody production. Further increase can be recorded by later encounters, such as supplemental immunizations/vaccinations or according to immunization schedules per age, but ultimately a maximum is reached. This is the principle behind active immunization programme against infectious diseases [22,23]. This implies that partial uptake of vaccines per age lacks systemic mechanisms capable of producing sustainable secondary responses in increasing antibody production within definable period in fighting specific pathogens, but rather even the primary response antibody level will keep depleting as pathogens are encountered, thereby making such partial uptake of vaccines to be as good as none uptake of vaccine in disease prevention and control principle.
The difference in occurrence of ARI in relation to immunization status among infants between rural and urban communities, being higher in rural communities may be explained in terms of socioeconomic and cultural drivers of poor health seeking behaviour and attendant consequences, skewed towards rural communities.
Therefore, the result of this study will ensure specific emphasis in the design of programmes and policies aimed at strengthening routine immunization activities to ensure that, children complete their uptake of vaccines per age before they attain their first birth day as a mark of commitment in the resolution of the problem posed by acute respiratory infection within the scope of the Sustainable Development Goals (SDG) 3, which emphasizes healthy lives and promotion of wellbeing for all at all ages.
The existence of relationship between immunization status per age and pattern and risk of acute respiratory infection among infants is quite outstanding to herness benefits that goes with timely vaccinations to achieving prevention and control of ARI. This portrays the need for innovative plan of action for sustainable active immunization activities reaching out to the unreachable that are most times the most vulnerable.
Copyright: © 2019 AS Ibama., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.