Hazar Khankan* and Sawssan Ali
Pulmonology Division, Department of Pediatrics, Children’s Damascus University Hospital, Syria
*Corresponding Author: Hazar Khankan, Pulmonology Division, Department of Pediatrics, Children’s Damascus University Hospital, Syria.
Received: May 29, 2019; Published: July 10, 2019
Citation: Hazar Khankan. “Pulmonary Agenesis Type 3 (Hypoplasia) - A Report of Two Cases in Children”. Acta Scientific Paediatrics 2.8 (2019):24-27.
Pulmonary agenesis is a very rare congenital anomaly characterized by the absence of pulmonary parenchyma, bronchial tree and vasculature. It may be associated with other congenital anomalies. Patients may present early, especially with repeated pulmonary infections, or be asymptomatic for many years. The certain diagnosis is mainly based on imaging studies with preference for chest CT scan. According to amounts of pulmonary parenchyma, bronchial tree and vascular supply, this condition is classified into three types: agenesis, aplasia and hypoplasia.
In our report we present two cases with different presentations and same diagnosis, which is pulmonary agenesis type 3 (hypoplasia). First case is a left pulmonary hypoplasia in a 6-month-old male infant. Second case is a right pulmonary hypoplasia in a 3-yearold female child.
Keywords: Pulmonary; Lung; Agenesis; Hypoplasia; Chest Computed Tomography (CT)
CXR: Chest X-Ray; CT: Computed Tomography; CRP: C-Reactive Protein
Pulmonary agenesis (Lung agenesis) is a very rare developmental anomaly characterized by the absence of pulmonary parenchyma, bronchial tree and vasculature. The estimated incidence is 1 in 10,000- 15,000 births [1]. Although it is a rare condition, more cases have been reported over the past years due to availability of non-invasive diagnostic imaging methods. Herein, we report two cases of lung agenesis type 3. The first case showed respiratory symptoms early after birth, which is common among patients who have this congenital anomaly, while the second case did not show any symptoms until the age of 3 years, which is not a common presentation of this condition.
A 6-month-old male infant presented with a history of chronic cough, recurrent pulmonary infections and failure to thrive. He was born by normal vaginal delivery to a non-consanguineous parent.
Physical examination revealed subcostal and intercostal retractions, wheezing on both sides of chest and diminished breath sounds on the left side.
On investigation, chest CT topogram (equivalent to chest X-ray) showed decreased lung volume on the left side, increased lung volume on the right side with mediastinal shift to the left (Figure 1). Chest computed tomography (CT) scan showed decreased size of the left lung with presence of the left main bronchus, compensatory increase in the right lung volume, herniation of the right lung towards the left side and cardiac shift into the left hemithorax (Figure 2 and 3). Echocardiography revealed secondary pulmonary hypertension and no anatomical cardiac defects.
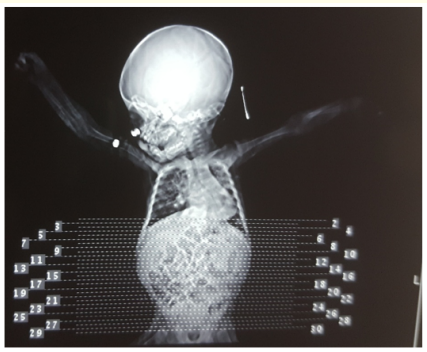
Figure 1: Chest CT topogram shows decreased lung volume on the left side, increased lung volume on the right side and mediastinal shift to the left.
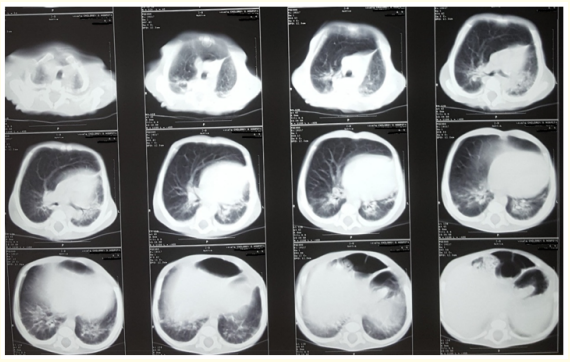
Figure 2: Chest CT scan shows decreased size of the left lung, increase in the right lung volume, herniation of the right lung towards the left side and cardiac shift into the left hemithorax.
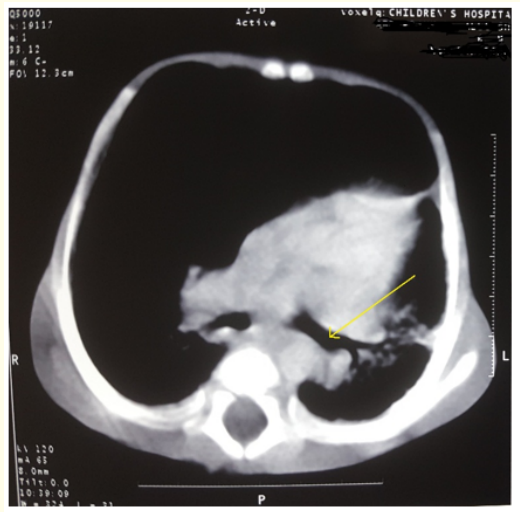
Figure 3: Chest CT scan shows the left main bronchus (yellow arrow).
Finally, the patient was diagnosed as having left pulmonary agenesis type 3 (hypoplasia).
A 3-year-old female child presented with the complaint of cough, shortness of breath and fever for the last 20 days. There was no history of recurrent pulmonary infections or respiratory symptoms before this complaint. She was born to a non-consanguineous parent. She was hospitalized in another center and treated as pneumonia (with Vancomycin plus Ceftriaxone) based on opaque right hemithorax on CXR. After 5 days the patient was referred to Children's Damascus University Hospital to complete study and management.
At admission, physical examination revealed decreased breath sounds on the right hemithorax with crackles, heart rate of 110 per min, no cyanosis or respiratory distress on room air and no fever.
Investigations revealed hemoglobin of 11.8 mg/dl, total leucocyte count of 3,400/mm3 (Polymorphs 53%, lymphocytes 27%) and CRP of 0.5 (upper normal limit is 0.5).
Intravenous antibiotic therapy was continued with Vancomycin plus Ceftriaxone for another 8 days. On chest clinical examination, crackles disappeared but breath sounds on the right hemithorax were still decreased.
Further imaging study was performed. Repeated CXR showed deviation of heart, trachea and mediastinum to the right with increased opacity on the right hemithorax and compensatory hyperinflation of contralateral side (Figure 4). Chest CT scan showed reduced volume of the right lung parenchyma with presence of the right main bronchus and right pulmonary artery, compensatory increase in the left lung volume and cardiac shift into the right hemithorax (Figure 5 and 6). Echocardiography revealed no pulmonary hypertension and no anatomical cardiac defects.
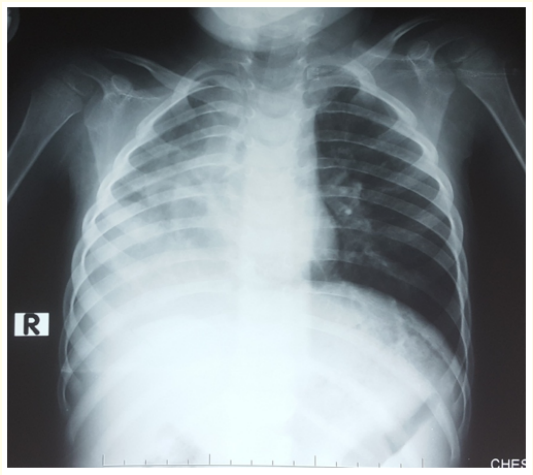
Figure 4: CXR shows deviation of mediastinum to the right with increased opacity on the right hemithorax and compensatory hyperinflation of the left hemithorax.
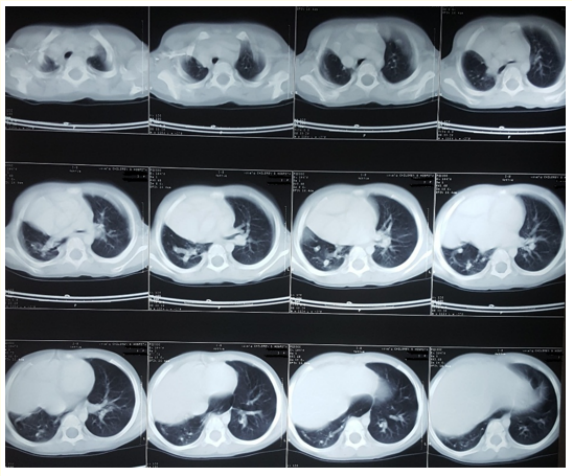
Figure 5: Chest CT scan shows reduced volume of the right lung parenchyma with increase in the left lung volume and cardiac shift into the right hemithorax.
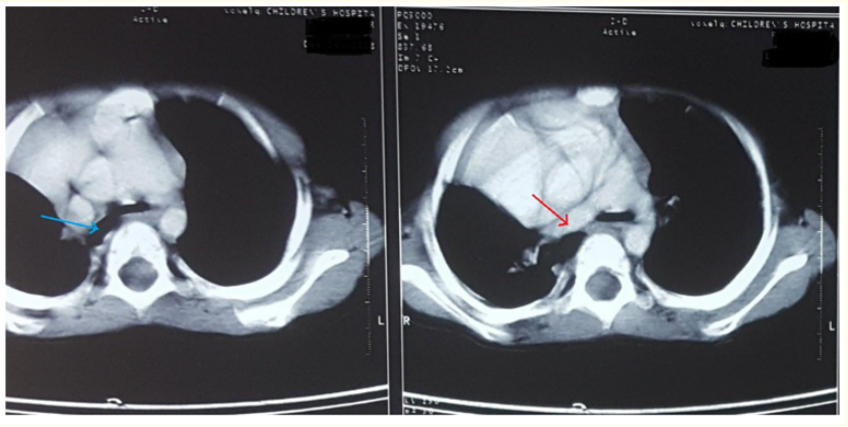
Figure 6: Chest CT scan shows the right main bronchus (blue arrow) and the right pulmonary artery (red arrow).
The patient was diagnosed as having right lung agenesis type 3 (hypoplasia).
Lung agenesis is a rare congenital anomaly. Although its etiology remains unknown, this condition is thought to be an autosomal recessive trait [1]. This anomaly can be unilateral or bilateral. Almost 50% of cases are associated with other congenital anomalies of the cardiovascular, gastrointestinal, skeletal and genitourinary systems [2-4]. In our cases, no accompanying congenital defects were detected.
Lung agenesis is classified into three types as following [5-7]:
As presented early, our two patients were diagnosed with type 3 (Hypoplasia).
Clinical presentation varies. Patient may be asymptomatic or critically ill. It depends on the side of agenesis and accompanying congenital defects. Symptomatic children usually present with recurrent pulmonary infections and respiratory distress, like in the first case.
Time of diagnosis depends on the appearance of clinical manifestations but it may be recognized by a routine examination in an asymptomatic patient [8]. Some reports have mentioned first time diagnosis in adulthood [9,10] while others have reported prenatal diagnosis [11,12]. Unilateral lung agenesis was first recognized prenatally in 1997 by Kalache., et al [13].
Diagnosis is made by imaging studies with preference for chest CT scan [14-16]. It provides details about lung parenchyma, vascular supply and bronchial tree. Chest X-ray usually shows increased opacity of the affected side with mediastinal shift to the ipsilateral side and compensatory hyperinflation of contralateral side. Bronchoscopy can help in detecting rudimentary bronchus. Echocardiography is important to rule out accompanying cardiac defects and to demonstrate pulmonary hypertension which is a common complication of lung agenesis. In our report, the patient who had early symptoms after birth was the one who had pulmonary hypertension.
Bilateral lung agenesis is incompatible with life after birth. Patients with agenesis of the right lung have poor prognosis comparing with patients with left lung agenesis [1,17].
The mainstay in management is to prevent and treat pulmonary infections.
Lung agenesis is a very rare condition and establishing the diagnosis is still difficult, so it is imperative that physicians have a high clinical judgment. When a patient has a decreased breathing sounds on one side of the chest with increasing opacity on CXR on the same side, then lung agenesis should be kept in mind as a differential diagnosis. Not only in cases with a history of recurrent respiratory infections, but even in cases that were previously asymptomatic. If lung agenesis is suspected, then CT scan should be done to clarify the diagnosis.
None.
The authors declare that they have no competing interests.
Copyright: © 2019 Hazar Khankan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.