Manochihr Timorian*, Razmi Rahman and Abdul Saboor saboor
Department of Cardiothoracic and Vascular Surgery, Pediatric Cardiology and Critical Care, Amiri Medical Complex Kabul, Afghanistan
*Corresponding Author: Manochihr Timorian, Department of Cardiothoracic and Vascular Surgery, Pediatric Cardiology and Critical Care, Amiri Medical Complex Kabul, Afghanistan.
Received: May 17, 2019; Published: June 17, 2019
Citation: Manochihr Timorian., et al. “Early Outcome After Total Correction for Tetralogy of Fallot in Department of Cardiothoracic and Vascular Surgery Amiri Medical Complex Kabul Afghanistan ”. Acta Scientific Paediatrics 2.7 (2019):08-11.
The purpose of this study was to evaluate the early out come after total correction of tetralogy of fallot in 180 consecutive patients with a mean age of 5-30 years underwent repair of surgery in a single center Amiri medical complex Kabul Afghanistan between august 2015 and October 2018.
Method: 8 patients had initial palliative operations (modified BT shunt) in outside centers and referred to us for total correction, trans annular pericardial patch was inserted in 133(73,8%) patients, 32(17,7%) patients repaired trans atrial total correction (ventricular septal defect, right ventricular out flow tract muscle band resection and pulmonary valvotomy through right atrium) for 5(2.7%) patients with absent pulmonary valve, monocuspid and bicuspid pulmonary valve reconstructed with pericardial patch. Result: Mean follow up was 1-3 months post operatively, mortality was (8,8%) (16patients) most of the patients whom repaired with trans annular patch had free pulmonary valve regurgitation post operatively by trans thoracic echocardiography, 26 patients had excellent function of their native valve, monocusp and bicuspid reconstructed pulmonary valve by pericardial patch, the peak gradient of right ventricular out flow tract was 10 to 35 mmHg post operatively. 22 patients had small(tiny) residual ventricular septal defect and none of the patients had complete heart block (0%).
Conclusion: Total correction of tetralogy of fallot can have low operative mortality and provide excellent short and long term survival, this experience suggests that key factor in total correction of tetralogy of fallot is to correct the pathology completely.
Keywords: Pulmonary Valve; Tetralogy; Fallot
Tetralogy of fallot is the most common cyanotic congenital heart disease with approximately 3000 new cases diagnosed in the united states each year.
The first complete repair of tetralogy of fallot was successfully performed by C. Walton Lillehi and his team in 1954, despite some advocates of rootin primary repair in infancy, unacceptable early mortality resulted in wide acceptance of a two stage repair with excellent results.
During the early 1990 s reports documented improved early results with primary repair was associated with improved outcome compared to a two stage approach, the purpose of this study was to analyze early postoperative and late result in total correction of tetralogy of fallot.
Between august 2015 to September 2018, 180 consecutive patients with tetralogy of fallot(TOF) (pink TOF Spo2>80% in room air and blue TOF Spo2 < 80% in room air) underwent total correction for tetralogy of fallot at department of cardiothoracic and vascular surgery amiri medical complex Kabul Afghanistan for the first time, there were 101(56.1%) male patient and 79(43.8%) were female patient Age ranged from 5 to 30 years old and weight was (9-55 kg).
These includes patient with classic tetralogy of fallot and associated pathologic processes such as atrial septal defect, patent ductus arteriosus and absent pulmonary valve (table 1), there were just 8 (4.4%) patients with primary palliative procedures (modified BT shunt) were referred to us for total correction.
The diagnosis of tetralogy of fallot for all patients were made by transthoracic echocardiography, CT angiography and cardiac catheterizations (table 2).
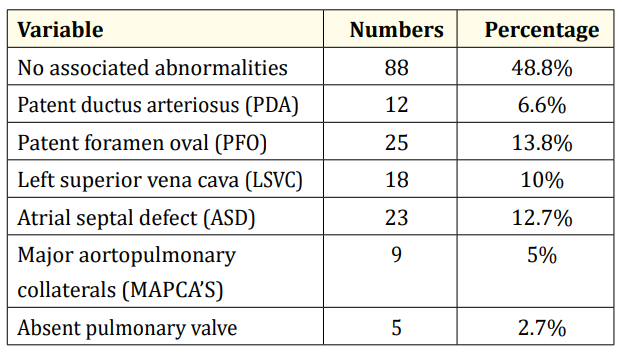
Table 1: Associated cardiopulmonary abnormalities.
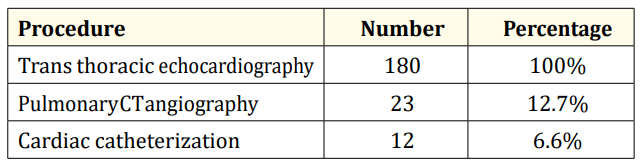
Table 2: Major diagnostic tools for diagnosis of tetralogy of fallot.
Figure 1
Figure 2
From review of the medical record data were collected relevant to the date of total correction, the follow up was achieved in 156(86.6%) patients in cardiology clinic, mean follow up was 3050 days post-operative.
The heart exposed through a median sternotomy a patch of pericardium was removed for ventricular septal defect repair and right ventricular out flow tract reconstruction, pulmonary artery trunk with branches dissected.
The operation was performed under cardiopulmonary bypass with hypothermia (nasopharyngeal temperature of 30-32c) intermittent doses of cold cardioplegia (del Nido cardioplegia) were used for myocardial protection, right atriotomy was used to expose the ventricular septal defect and right ventricular out flow tract muscle band resection.
In trans right atrium total correction ventricular septal defect, right ventricular outflow tract muscle band resection and pulmonary valve commissurotomy were done through right atrium. Ventricular septal defect patch was sewn by continues suture, the right ventricular outflow tract and pulmonary artery were enlarged with autologous pericardium in 133(73.8%) patients, monocuspid and bicuspid pulmonary valve reconstructed with autologous pericardium in 15(8.3%) patients.
In case of right or left pulmonary artery stenosis the patch was carried beyond the point of stenosis, all patent foramen ovals were closed by direct sutures and atrial septal defects were closed by pericardial patches.
Over all mortality was 16 patients (8.8%), 4 patients died due to sever bleeding pulmonary haemorrhage, 2 patients because of right Ventricular failure, 3 patients died due to multi organ failure, 4 patients because of sepsis, in 3 patients ventricular septal defect patch dehiscence were occurred and they died because of heart failure (patients attendant were not agree with re operation) there was not on table death.
Aortic cross clamp time was (30-45min) and cardiopulmonary bypass time was (55-75min), factors affecting operative survival were analyzed, aortic cross clamp time and cardiopulmonary bypass time not affected operative survival.
Previous palliative procedure did not adversely affect operative mortality.
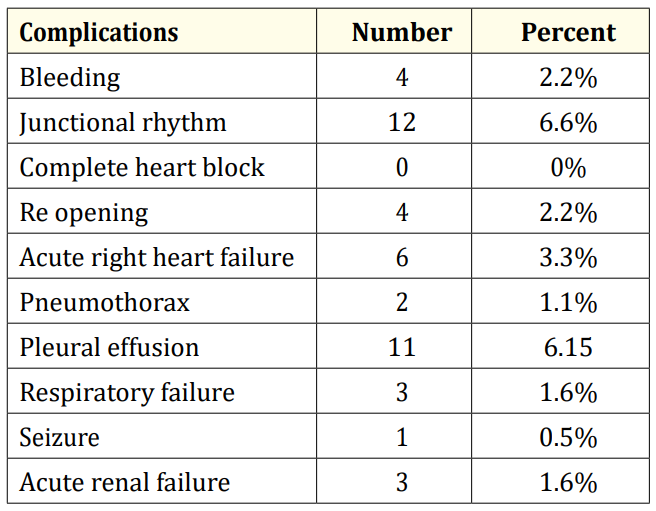
Table 3: Post-operative complications.
Among operative measurement construction of the right ventricular outflow tract with a patch was not related to early mortality, perioperative measurement of hematocrits level was significantly related to early mortality and perioperative thrombocytopenia was the great risk factor for postoperative mortality.
Postoperative ventilation more than 48 hours than tracheostomy was necessary in 3 (1,6%) patients, transient right heart failure required inotropic support for 72 hours occurred in 18(10%) patients, use of temporary pace maker was required in 13 (7.2%) patients, no patient required permanent pace maker implantation in the perioperative period postoperative complication shown in table (3).
Figure 3
The median length of stay in intensive care unit was 2- 8 days, the median hospital stay was 4-16 days.
Residual anatomical defect were first diagnosed by clinical and echocardiographic or both, 22 patients had a tiny residual ventricular septal defect (VSD) and most of the patients with trans annular patch had free pulmonary regurgitation, 5(2.7%) patients with pulmonary valve reconstruction (bi cusp and mono cusp) with pericardial patch had good function of reconstructed valve with mild pulmonary valve regurgitation, 32(17.7%) patients whom repaired trans right atrium total correction had excellent function of pulmonary valve and right ventricle function.
Despite total correction of tetralogy of follot being a common cardiac surgical procedure for more than 50 years, some controversy still exist regarding the optimal treatment method.
Some groups advocated routine two staged procedure for tetralogy of fallot with a shunt for symptomatic patients during infancy and total correction within 1.5 years of palliation, other investigators propose selective staged management with initial shunting particularly in patients with less than ideal anatomy, however patients with undergoing staged treatment of tetralogy of fallot using a palliative shunt and subsequent total correction accrue the risk of two operative procedure and the potential complications of right to left intra cardiac shunting, compromised ventricular function and fibrosis with ongoing hypoxemia and myocardial ischemia, the selective operative treatment of tetralogy of fallot has developed from previous surgical failure and surgical successes with the operative management of various subset of patients with the tetralogy fallot.
We originally thought that significantly higher operative mortality might be found in those patients with the most sever intra cardiac malformation and high haematocrit [1-20].
There is general agreement that the best treatment of patients with tetralogy of fallot is complete repair in infancy which may reduce the incidence of late electrophysiological and hemodynamic problem and improve survival, the trans atrial approach is a feasible technique for total correction of TOF in adequate pulmonary annulus size with satisfactory echocardiography performance of late postoperative right ventricle and pulmonary valve functions.
Copyright: © 2019 Manochihr Timorian., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.