Diniece Barran, Lesje Atkinson, Seleshi Demissie and Pushpom James*
Staten Island University Hospital, Northwell Health, SUNY Downstate College of Medicine, New York, USA
*Corresponding Author: Pushpom James, Staten Island University Hospital, Northwell Health, SUNY Downstate College of Medicine, New York, USA.
Received: March 13, 2019; Published: May 06, 2019
Citation: Pushpom James., et al. “Promoting the use of Inhalers with Spacers on Discharge from the Pediatric Emergency Department”. Acta Scientific Paediatrics 2.6 (2019):09-12.
Background: Spacer use with a metered dose inhaler (MDI) is the preferred method of asthma medication delivery to children, but many patients seen for asthma exacerbations do not receive a prescription of a MDI with spacer.
Objective: To improve the prescription of MDI with spacers, to children presenting to the pediatric emergency department with asthma exacerbations.
Methods: Over a six month period, educational in-services to providers and brochures for parents and patients were distributed to review the benefits of prescribing MDIs with spacers. MDI with spacer prescriptions were compared in the six months before and six months after this educational initiative.
Results: There was no significant increase in the prescription of MDI with spacers by providers, and the majority of patients were sent home without documentation of an inhaled asthma medication. However, there was an increase in the documentation of spacer prescription in the patient’s records, when MDIs were prescribed.
Conclusions: Metered dose inhaler prescriptions need to be provided to patients on discharge from the Emergency Department. Spacer prescription and documentation of education need to be improved when a MDI is prescribed. Sustained educational efforts are necessary to accomplish this.
MDI/spacer use in pediatric asthma is associated with better clinical scores and decreased rates of hospitalization.
This quality improvement project involved developing a brochure to distribute to families/patients to encourage MDI/spacer use and education to encourage ED health care providers to prescribe MDI/spacers in lieu of nebulized medication.
This quality improvement project aims to disseminate the advantages of prescribing MDI/spacers to children with asthma, as a way to improve asthma control.
Keywords: Inhaler; Spacer; Pediatric
ED: Emergency Department; EMR: Electronic Medical Record; MDI: Metered Dose Inhaler; SIUH: Staten Island University Hospital.
Inhalational therapy, which delivers medications directly to the lungs, is the preferred method of delivery for the treatment of asthma. The most commonly used devices are nebulizers and metered-dose inhalers with spacers (MDI/spacer). Either can be used for maintenance medication as well as emergency treatment of an acute exacerbation. Children can be started on either nebulized medication or a MDI/spacer. Younger children require a facemask with the spacer, while older children need to use a spacer with a mouthpiece, for effective medication delivery. Inhalation therapy through the use of a MDI/spacer, improves lung deposition, while minimizing systemic side effects [1].
Prescription of inhalational therapy must be accompanied by thorough education on the proper use of an inhaler and the importance of routine use of inhaled corticosteroids, when these are prescribed. Studies have found that many children fail to use a spacer or their technique is suboptimal, resulting in poor medication delivery and therefore inadequate asthma control [2,3]. Providers should monitor patients’ inhaler technique at each visit, correcting any errors in administration and educating patients and parents on the importance of proper inhaler with spacer use [4].
Research has shown that MDI//spacers are as effective as or better than nebulizers in aerosol delivery to children [5-7]. One study found that MDI/spacers were associated with better clinical scores and decreased rates of hospitalization [8]. MDI/spacers are easier for children to use and require less parental time and effort. They are portable, require no energy source or dose preparation, and require lower amounts of medication than nebulizers. Studies have suggested that shorter or simpler medication regimens are more likely to be associated with good compliance [9]. MDI// spacers require less time and are easier to use than nebulizers. Nebulizers require thorough cleaning and maintenance [10]. MDI/ spacers are cheaper, a significant factor in considering a patient’s ability to continue routine inhaled corticosteroid therapy, when this is prescribed. For maintenance therapy, compliance with a MDI/spacer is likely to be better than with a nebulizer, because it is less time consuming and easier to use. MDI/spacers are the recommended devices for asthma medication delivery [8]. However locally, the transition to prescribing MDI/spacers instead of routine nebulizer therapy has been slow [11].
This was a single-center, descriptive study with a pre-/posttest design, based on retrospective reviews of electronic medical records. The study was conducted in the ED of our 714 bed, atertiary-care teaching hospital located in New York City. The pediatric ED has a census of 20,300 patient visits per year. The study included two six-month periods, a year apart. The preimplementation period used for comparison was November 1, 2015 – April 30, 2016, and the post-implementation period was November 1, 2016 – April 30, 2017. All pediatric patients between one year and eighteen years of age, who were discharged from the pediatric ED who had a diagnosis of asthma, asthma exacerbation, or wheezing were randomly selected for this study.
Records were reviewed for six months before project initiation and six months after initiation. The number of patients receiving nebulized albuterol, MDI/spacers, both, or neither was recorded and percentages before and after project initiation were compared. Documentation in the patient’s record regarding spacers, including educating patients regarding use, was also recorded.
Our interventions included education designed to increase awareness of MDI/spacer therapy to attendings, residents, patients and their families. In-services were held to educate ED residents and pediatric residents on the benefits of spacer use for the treatment of asthma. Emails were sent to ED residents and attendings and one-on- one training was provided in real time to residents who rotated through the ED, during this time period. A brochure (See Supplementary attachment) was created and distributed to patients and parents in the pediatric ED. This brochure outlined the correct spacer to use in different age groups, why MDI/spacers are preferred over nebulizers, why spacers are important when using MDIs, and steps to follow for proper use. The brochure was included in the emails sent to faculty and residents. These interventions were implemented between May 1 2016 and October 31 2016.
A total of 194 patient records were evaluated before project initiation, and 194 after. For the pre-initiation cohort, the average age was 10.1 with a standard deviation of 5.47. Post-initiation cohort, the average age was 10.6 with a standard deviation of 5.61 (Table 1).
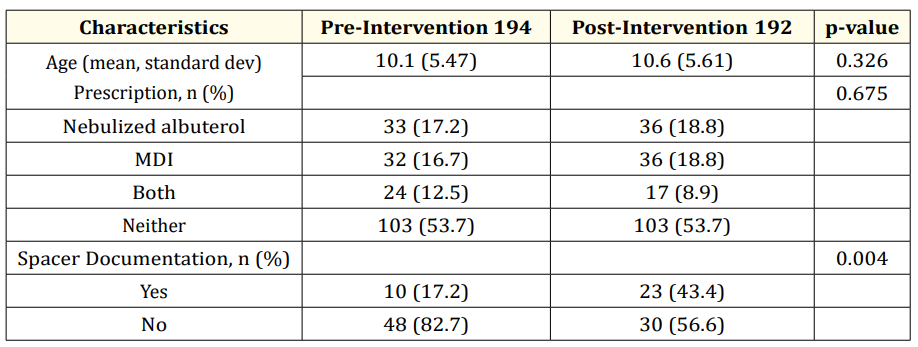
Table 1
Results of our analysis are recorded in figures 1-3. Of the pre-project cohort, 33 patients (17.2%) received nebulized albuterol, 32 patients (16.7%) received a MDI/spacer, 24 patients (12.5%) received both and 103 patients (53.77%) did not have documentation of receiving either.
Post-project initiation, 36 patients (18.8%) received nebulized albuterol, 36 patients (18.88%) received MDI/spacer, 17 patients (8.99%) received both, and 103 patients (53.77%) did not have documentation of receiving either.
Spacer documentation in patient charts was present in 10 of 58 (17.22%) before project initiation, and 23 of 53 (43.44%) after completion of project, resulting in a 56% percent improvement in documentation from baseline.
Despite our educational initiative, there was no significant increase in the prescription of MDI/spacers over nebulizers to patients who presented to the SIUH pediatric ED for an asthma exacerbation. This may have been in part because of the large number of providers in the emergency department, with frequent turnover. It is likely that to achieve significant results, we would need to contact every ED provider in a more sustained way. Multiple in-services to residents may have been helpful. Another issue was that the EMR system was being changed, so there was reluctance to add an alert in the old EMR which was being used during this study. Having an alert in the EMR would likely have increased prescription of MDI/spacers and encouraged documentation of education regarding spacer use.
During this project it became obvious that documentation needs to improve regarding whether a spacer script was provided, if spacer education was provided, and what method of medication delivery the patient was using at home.
While 27.6% of our study patients received MDI/spacer scripts or both MDI/spacer and nebulized medication in the post-intervention period, 43.4% of records had documentation of spacer prescription and education about spacer use. A study found that as few as 34% of children used a MDI/spacer correctly before standardized education was provided, concluding that proper education on device use may lead to significant improvement in asthma control [4]. Simply prescribing a MDI/spacer is not sufficient. Spacer documentation and education needs to be improved at our institution when a MDI/spacer is prescribed.
Encouragingly, spacer documentation was one aspect where we saw significant improvement during the course of our initiative. Hopefully, with more sustained education, MDI/spacer prescription and documentation of education will improve
There was no statistically significant increase in the prescription of MDI/spacers alone over group of patients who only received nebulized medications during our study period. The very slight increase of 2.11% was not statistically significant (p=0.675675). However, the increase in documentation of spacers in patient’s charts was statistically significant (p==0.0044). A majority of patients received neither a prescription for MDI/spacer nor nebulized medication. This maybe because it was unclear from the documentation whether these patients were receiving home medications, using a MDI/spacer or a nebulizer.
Pushpom James, MBBS, conceptualized and designed the study. She reviewed and revised the initial and final manuscript for important intellectual content. Diniece Barran, M.D. wrote the initial and final manuscript, collected data and reviewed data. Seleshi Demissie, PhD conceptualized the study, reviewed the manuscript and provided statistical analysis. Lesje Atkinson conceptualized the study, reviewed data and revised the manuscript.
Copyright: © 2019 Pushpom James., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.