Omar Atef Elekiabi1, Mohamed E Eraky1, Waleed A Abdelhady2, Ahmed M Sallam2 and Loay M Gertallah2*
1Department of Pediatric surgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt 2Department of General surgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt
*Corresponding Author: Loay M Gertallah, Department of General surgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt.
Received: March 28, 2019; Published: May 02, 2019
Citation: Loay M Gertallah., et al. “A Comparative Study between Laparoscopic Repair and Open Repair of Pediatric Inguinal Hernia; Outcomes and Benefits”. Acta Scientific Paediatrics 2.6 (2019):03-08.
Background: The improvement of pediatric laparoscopic instruments and increased experience with laparoscopy technique, laparoscopic inguinal hernia repair in children become an important skill which the laparoscopist must be aware of. Laparoscopic repair of inguinal hernias in children is less invasive, more feasible and less painful. Additionally, this procedure is that, it could allow contra lateral hernia detection and repair in same setting.
Aim: In our study we aimed to compare between the outcomes of the conventional opened repair and the laparoscopic repair of pediatric inguinal hernia.
Materials and Methods: The current prospective study which included 30 patients with inguinal hernia who were divided in to two groups the first group included 10 patients and was managed by laparoscopic repair, while the second group included 20 patients and was managed by the conventional open repair.
Results: The mean time of operation in laparoscopic repair is slightly shorter than that of opened repair but this was not statistically significant. Post-operative recovery was significantly faster in patients undergoing open repair than in laparoscopic repair (p = 0.003). Post-operative discharge was significantly faster in undergoing open repair than in laparoscopic repair (p = 0.025). Postoperative secondary hydrocele was common in laparoscopic repair that in open repair while scrotal edema was common in opened repair that laparoscopic repair (p = 0.049). Patient cosmetic Satisfaction was higher in group 1 with laparoscopic repair than in group 2 with opened repair (p = 0.012).
Patient financial satisfaction was lower in group 1 with laparoscopic repair than in group 2 with opened repair (p = 0.046).
Conclusion: Laparoscopic repair of inguinal hernias in children is less invasive, more feasible, less painful and it could allow contra lateral hernia detection and repair in same setting.
Keywords: Laparoscopic Repair; Open Repair; Inguinal Hernias fants.
The incidence of pediatric inguinal hernia ranged from 0.8 percent to 4.4 percent and it is higher in infant aged less than one year. Boys are affected about 6 times higher than girls.
The site of pediatric inguinal hernia is more common in the right side than the left side and it is bilateral in 10% of cases [1]. Inguinal hernia will not improve spontaneously and its surgical treatment is a must, due to the risk of incarceration, especially in young infants. It was reported that about ninety percent of complications are avoided when the repair is performed during the first month of diagnosis. Plethora of surgeons have recommended hernia repair immediately after diagnosis [2].
The first laparoscopic repair of inguinal hernia repair was reported round the 1990s, [3], since then many techniques have been described which can be divided in to two major groups [2]; intra-corporeal technique that included dissection, ligation and division of the sac that resemble the true classic inguinal herniotomy [4,5] and the extra-corporeal percutaneous technique which compromised ligate the patent processus vaginalis without its division [6-8]. Up till now no consensus existed that could favor any of both techniques. I was found that laparoscopic repair is minimally invasive, safe and effective method for management of inguinal hernia if adequate training and mentorship are assured [9]. Due to the advancement of pediatric laparoscopic instruments and improvement of the experience with the laparoscopy technique, many centers perform laparoscopic repair for inguinal hernia in children as a routine work [10]. Recently this procedure is less invasive, less painful and it has allowed the early diagnosis and adequate repair of the contra lateral hernia in the same procedure [11].
In our study we aimed to compare between the outcomes of the conventional opened repair and the laparoscopic repair of pediatric inguinal hernia.
This is a prospective study which was designed to compare between laparoscopic repair and open repair in management of pediatric inguinal hernia regarding; outcome, benefits and drawbacks.
Our study was performed in Pediatric Surgery Department, Faculty of Medicine, Zagazig University. The approval of local ethical committee of Faculty of Medicine Zagazig University was obtained. A total of 30 children who were complaining of inguinal hernia were included for a period from January, 2016 to March 2018.
All selected patients were divided in to two groups the first group included 10 patients and was managed by laparoscopic repair, while the second group included 20 patients and was managed by the conventional open repair.
Written informed consents were acquired from all patients’ guardians for all surgeries.
Patients were admitted to Pediatric Surgery Department in the evening before the operations after they were screened for any co-morbid conditions or undescended testis. Patients were made fasting for about four hours before surgery. No pre-operative medications were given to any of them.
We have operated one patient by laparoscopic repair and next two patients by open repair. We have recorded patient’s demographic data, duration of the operation, postoperative pain, complications, recurrence and cosmetic satisfactions.
Laparoscopic hernia repair was performed under general anesthesia with endotracheal intubation of the patients, while open repair was done by inhalational anesthesia.
In the group of patients who underwent laparoscopic repair, sterile draping was done after antiseptic preparation of the anterior abdominal skin. An umbilical port measured a five5 mm was done by the open procedure and pneumoperitoneum was done and inflation of Carbon-di-Oxide was done making the pressure fixed within about 8-10mm Hg. Then a three hundred telescope which has a camera was put into the abdominal cavity using that port and detection that processus vaginalis is patent through internal inguinal ring of diseased side was done. During direct telescope guided vision introduction of the two five mm working ports were done through right and left lower abdomen. Then introduction of Maryland forceps and needle holder were done from these ports. Then a 3-0 vicryl suture and a cutting needle were put directly into the abdominal cavity piercing the abdominal wall. After reduction of the contents of the sac with a forceps help, we have made purse-string sutures around the internal ring by coordinated manipulation of the working instruments. We made further reinforcing knots. Contra lateral side was checked for processus vaginalis patency and if it is diagnosed it was repaired in the same setting which described above. Then all ports were removed, the gas was squeezed out and port wounds were closed by subcuticular 3-0 or 4-0 vicryl. We have applied sterile dressings. In the group of patients who underwent opened repair, after antiseptic preparation of the lower abdominal wall, we made an incision in the crease in the lower abdominal skin on the diseased side; the incision begins slight lateral to the pubic tubercle. After we dissect Camper fascia, fascia of Scarpa and aponurosis of the external oblique muscle from the superficial to deep direction, we have swiped out the cremesteric muscle and fascia by blunt dissection with a forceps. We detected the hernial sac antero-medial to the spermatic cord, then we separated it from testicular vessels and from vas difference (in male patients) using the blunt dissection. We have dissected sac was dissected proximally up to internal inguinal ring which is marked by extra peritoneal fat appearance. We have ligated the sac neck at the level of the internal ring with 3-0 or 4-0 vicryl and was excised distal to the knot. We have excised redundant portion of sac was excised out if it was small enough or it was left in place if it was big.
We have closed the wound in layers and we closed the skin with 3-0 or 4-0 vicryl sutures. Finally we have applied sterile dressing.
We have used acetaminophen for analgesia (fifteen mg/kg/ dose, every six hours) in children who need relief of pain. We discharged patients once they were stable hemodynamically, with no residual anesthesia effects and are tolerating oral feeding well. We have asked parents of the patients to bring the patients back to the outpatient department for review. All patients were assessed for postoperative pain, postoperative secondary hydrocele, scrotal edema; cosmetic appearance of the scar; changes in testicular size, if any complications are present as compared with the preoperative state. We have followed our patients for an average of six months to evaluate these short-term outcomes by ultrasound.
All data were analyzed using Statistical Package for Social Science for windows version 18.0 (SPSS Inc., Chicago, IL, USA). All tests were two sided. p-value < 0.05 was considered statistically significant.
This study was carried out from January, 2016 to March 2018 in the Department of Pediatric Surgery, Zagazig University Hospitals. Total 30 patients of inguinal hernia were grouped under 2 groups: Group-A, who underwent laparoscopic repair, (n =10) and Group-B who underwent open repair (n = 20) Table 1.
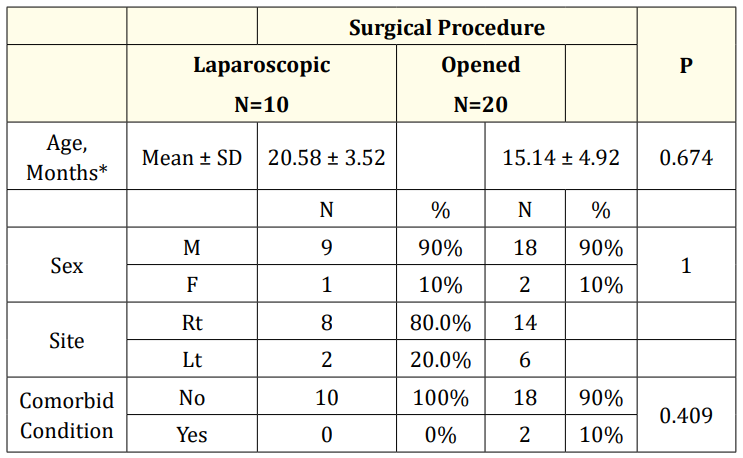
Table 1: Comparison of clinico-demographic prameters between both groups.
About ten children aged less than 12 Months old, the age of children undergoing laparoscopic repair was significantly older than those undergoing opened repair but this was not statistically significant.
The mean time of operation in minutes in laparoscopic repair is slightly shorter than that of opened repair but this was not statistically significant.
Post-operative recovery was significantly faster in patients undergoing open repair than in laparoscopic repair (p = 0.003). Post-operative discharge was significantly faster in undergoing open repair than in laparoscopic repair (p = 0.025). Post-operative secondary hydrocele was common in laparoscopic repair that in open repair while scrotal edema which resolved spontaneously in a few days was common in opened repair that laparoscopic repair and these results were statistically significant (p = 0.049).
Erythema over the suture line was observed in 1 cases performed with opened repair, which resolved with oral antibiotics. Patient cosmetic Satisfaction was higher in group 1 with laparoscopic repair than in group 2 with opened repair (p = 0.012). Patient financial Satisfaction was lower in group 1 with laparoscopic repair than in group 2 with opened repair (p = 0.046). In both the groups there was no recurrence table 2.
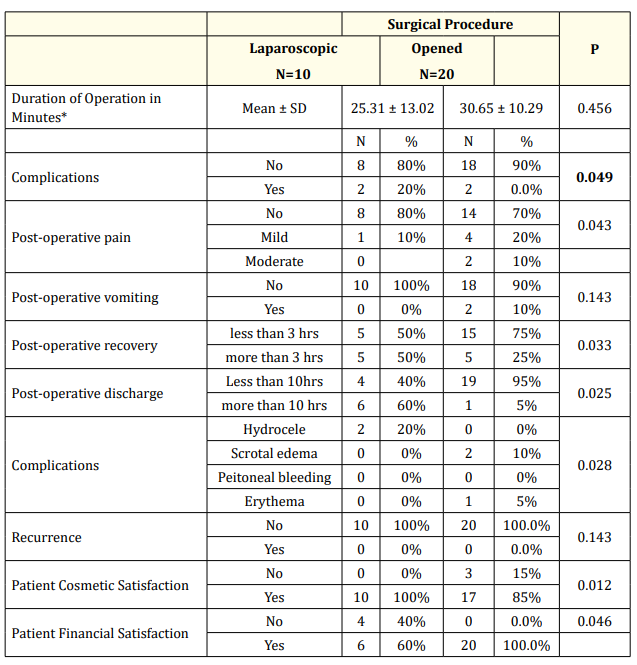
Table 2: Comparison between both groups regarding operative and post-operative parameters.
Inguinal hernia is considered a common surgical complain in children, and its surgical management by herniotomy is considered its standard management, as it could be performed easily, has a high success rate in addition to low rate of complications [12]. Despite that, the advancement in minimally invasive surgery made laparoscopy to gain popularity in pediatric hernia surgery also [13,14]. Laparoscopic pediatric hernia repair recently become comparable to conventional open herniotomy regarding its reported results with nearly similar recurrence rate and better cosmetic results. Additionally, the basic principle of laparoscopic pediatric inguinal hernia repair is a high ligation of the hernia sac from inside in continuity through using complete purse string suture or after peritoneal dissection around the internal inguinal ring to separate the distal hernia sac.
Our current prospective study is discussing two methods of pediatric inguinal hernia repair; laparoscopic with open methods. We have detected and proved the advantages and disadvantages of each method. We found that laparoscopic hernia repair is better than opened repair regarding the lower incidence of pain, better cosmosis, diagnosis and management of bilateral cases in the same setting, which was similar to Sharifuzzaman., et al. who proved similar results regarding better cosmosis but found no differences between both methods regarding post-operative pain and complication [1]. The recurrence rate of pediatric inguinal hernia repair is 1-2.5%, and such high rates of recurrence are more common in patients who were operated by young not well qualified surgeons or by surgeons who are not qualified in pediatric surgery [15]. For pediatric inguinal hernia, high hernia sac ligation is all that is needed for its correction [16]. Reported recurrences after the open repair might be due to plethora of factors; failure to ligate the sac high enough at level of the internal ring, inguinal canal floor injury due to operative trauma, failure of internal ring closure in girls, or wound infection and hematoma postoperatively [17]. In both groups no recurrence was found and we proved that laparoscopic inguinal hernia repair is a safe method that could prevent or avoid causes of hernia recurrence when performed carefully, which was similar to results of Sharifuzzaman., et al. and Cheung and Chan [1,18].
Laparoscopic repair of hernia ends the question of whether exploration of the contra lateral side is essential in children with inguinal hernia [19]. As in cases of open repair it was found on follow-up most patients have developed contralateral hernias. as these patients were managed by the open technique, rather than by laparoscopic tecnique, but the main benefit of the laparoscopic repair was the inspection of both sides and correction of bilateral hernia in the same setting [1]. We have found that the group A of patients who were managed by laparoscopic repair required lesser amount of analgesics than group B who was managed by the open technique. Wound complications were few in both groups. Moreover secondary hydrocele was not reported in open repair but was found in laparoscopic repair. Similarly, Bharathi have noticed transient occurrence of hydroceles in laparoscopic repair more commonly due to thicker peritoneum bites that lead to lymphatic embarrassment [20].
All these results were similar to Sharifuzzaman., et al. and Bharathi [1,20]. Recovery from the effects of anesthesia was delayed in patients undergoing laparoscopic repair. This may be attributed to deeper anesthesia and muscle relaxation which is needed during intubations [21]. Open repair can be performed with the patient under a face mask, in addition to simultaneous administration of caudal analgesia. Even when a patient is intubated, the anesthesia levels and the needed relaxation are less. Similarly, Bharathi found that the rates of complication of both procedures were similar and minor [20]. Five-millimeter incisions in laparoscopic repair were, cosmetically better than open repair if compared with 2-cm incisions in open repair [13]. But, this benefit is of lesser value as the scar in open repair is hidden by clothes.
Laparoscopic inguinal hernia repair is, novel, safe and elegant, but the costs are not affordable in the developing world. So they prefer conventional open herniotomy that yields nearly similar results, so, it is still considered the standard of care.
Laparoscopic repair of inguinal hernias in children is less invasive, more feasible, less painful and it could allow contra lateral hernia detection and repair in same setting.
Copyright: © 2019 Loay M Gertallah., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.