Koleva Kr, M Georgieva*, N Rasheva, B Balev, P Drenakova and P Petrov
University Hospital “St. Marine”, Varna, Bulgaria
*Corresponding Author: M Georgieva, University Hospital “St. Marine”, Varna, Bulgaria.
Received: January 28, 2019; Published: April 15, 2019
Citation: Koleva Kr, M Georgieva., et al. “Case Report - Ulcerative Colitis in Early Paediatric Age Group”. Acta Scientific Paediatrics 2.5 (2019):55-57.
Ulcerative colitis, a subcategory of inflammatory bowel disease (IBD), is an idiopathic condition of gastrointestinal tract, causing inflammation and ulcers in the colon. Inflammatory bowel diseases are associated with an increased risk of vascular complications. The most important are arterial and venous thrombosis that have rarely been reported in children. The thromboembolic complications are thought to be a consequence of hypercoagulable status in IBD, resulting from the presence of a thrombogenic gastrointestinal mucosa and altered clotting factors. We report a case of deep venous thrombosis in femoral and iliac veins in a child with acute ulcerative colitis.
Keywords: Ulcerative Colitis; Nursery Age; Thrombosis
The ulcerative colitis and the Crohn's disease are part of the group of chronic inflammatory bowel diseases. They have many extraintestinal manifestations, manifested both as initial syndrome and as a complication.
Thromboembolic complications are considered to be the consequence of hypercoagulability in the IBD arising from the presence of thrombogenic gastrointestinal mucosa and damage to the clotting factors. These complications occur more frequently in adult patients. In childhood there are extremely few described cases in the special literature.
A 3 year old child diagnosed (clinically, endoscopically, histologically) with UA at 2 years of age is presented, in which the authors observe as a complication the development of deep vein thrombosis of femoral and iliac veins during treatment of relapse of the disease.
Boy MA, at 3 years, was hospitalized in emergency in the sector of children's gastroenterology at "St. Marina" University of Varna. The infant was found at 2 years of age and an epistemological treatment was performed with 5 ASA (Salofalk) 2 x 250 mg/24h with good effect until exacerbation. Exacerbation of UC began 2 weeks before hospitalization - diarrhea, 7 - 8 times a day, with mucus and blood impurities, 37.2 subfebrility, refusal of food, abdominal pain.
Child was in moderately impaired general condition, subfebrillary to 37.2, weight 19 kg, height 97 cm, BMI - 17.8m (85th percentile). Respiratory and cardiovascular systems - CT. Abdomen - mild, above chest, liver and spleen unstretched, peristalsis enhanced, soreness in the colon. Limbs - Movable, no swelling. Defecation - 6-7 stools with mucus and blood, watery-pulp.
CBC - norm, biochemical studies - glucose, creatinine, peak. picture, common protein, albumin, cholesterol, triglycerides, LDL cholesterol, LDH, GGT, alkaline phosphatase, cholinesterase, alpha-amylase - norm. Urea - 1 mmol/l, HDL - cholesterol - 0.55 mmol, ACAT - 123 U/l, ALAT - 102 U/l, lipase - 146 U/l, GGT - 59.0 U/82mg/l. Electrolytes and trace elements: sodium - 126.0 mmol/l, potassium - 3.90 mmol/l, chlorides - 89.0 mmol/l, iron - 2 mmol/l, calprotectin - 364 E (norm < 50). Coagulation status in the norm. Coprogram CT, Urine CT, Enterococcus faecalis, UC-40 index (moderate to severe) (according to Pediatric Index of Activity).
A 3 cm long liver on the right medioclavicular line, with a hyperechogenic structure. Gall Bladder - CT. There is no evidence of free flowing fluid. Kidneys - no specifics. Wall of colon descendens - thickened 8 mm. Large amount of gases.
During the hospital stay (on the 4th day after dosing), complaints of pain and edema of left lower limb appear. Laboratory and imaging studies indicated that it was the femoral vein thrombosis. Laboratory tests: showed platelets - 780.10 12/l (norm to 440), fibrinogen - 1.9 g/l (norm of 2.38 - 4.98 g/l), D-dimers - 1.620 mg/5 mg/L, APTT - 22 seconds (25.4 - 36.9 seconds), prothrombin time - 11.9 seconds (11.5 - 14.8 seconds). The patient underwent an ultrasound examination and a doppler of lower limbs, establishing normal vein passage to the right and venous thrombosis data of femoral vein. There was no evidence of a vena poplitea defect, but under pressure it showed resistance and was not compressed. A consultation with a vascular surgeon who gave Heparin therapy at optimal doses of 50 E/kg/24h, Endotelon 2 x 50 mg/24h, reclose, APРT monitoring every 12 hours, and control of Heparin infusion to maintain the parameter within a range of about 50 - 70 seconds was done.
For treatment with 5ASA and corticosteroids 2 mg/kg/24h, which started with the antibiotic treatment was added in combination: Metronidazole - 15 mg/kg/24h three times, Ceftriaxone - 80 mg/kg/24h twice. Amikacin - 20 mg/kg/24h twice, Ranitidine - 10 mg/kg/24h. A computer tomography (CAT) test on the abdomen and a small pelvis due to the risk of pulmonary thromboembolism was done. CAT confirmed the ultrasound finding and complemented it with the discovery of defects with the appearance of thrombus, placement in the b femoral vein, the external venae and internal iliaca, the iliaca communis sin and distal segment of vena cava (Figure 1). Tested and clotting factors, some of which show deviations - protein C -> 140% (rounded), factor VIII - 154 (norm 150), anti-thrombin 3 - 130% (norm 125). On the fifth day of treatment with Heparin, lower limb edema and palpation pain disappeared. The patient displayed improvement and treatment with low molecular weight heparins s. c 0,4ml once daily, 5 ASA (Salofalk 2x 250 mg/24h), hepatoprotective (Ursoflak 2h125mg, 1 month - due to transaminase elevations), Omega 3 × 1 capsules, Esomeprazole 2x 10 mg/24h, decreasing dose of corticosteroid. Switching from a standard treatment regimen to Infliximab treatment is recommended.
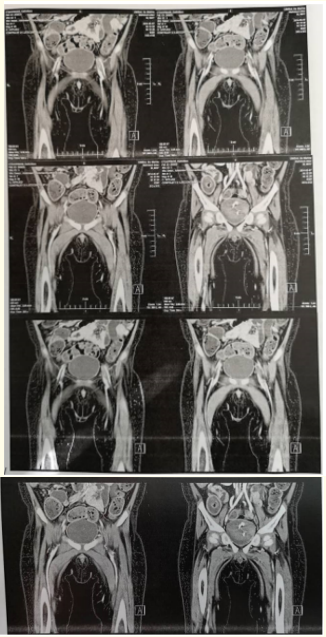
Figure 1: CAT examination of patient vessels.
Thrombosis and thromboembolism are known complications in UC patients but are extremely rare in pediatric patients [3,5]. Thrombosis, which occurs as a complication in patients with IBD, is believed to result from a disorder in blood clotting factors. A study of Lam., et al. [1] found an elevated factor VIII and V level and significantly reduced antithrombin 3. Another factor that plays a role in thrombogenesis in UC is thrombocytosis [4]. According to the literature, the thromboembolic complications of IBD are the combination of thrombocytosis, elevated levels of certain specific coagulation factors and decreased levels of endogenous anticoagulants. The damaged mucosa is considered a trigger of the coagulation system [2]. Based on these findings, it is increasingly accepted that treatment with corticosteroids used to control the disease may exacerbate the thrombosis process [2]. Laboratory thrombocytosis, decreased fibrinogen, increased factor VIII, antithrombin 3 and protein C and shortened post-thrombus time were established in the described case. The thrombotic event occurs during treatment of active UC, which suggests that disease control is essential to prevent complications such as thromboembolism. Despite all the facts and conclusions set forth, it is impossible to produce standard therapeutic behavior in these cases at least because thromboembolism as a complication of UC in infancy is very rare, making it difficult and costly to conduct a prospective study aimed at clarifying reasons and optimize the diagnostic and therapeutic approach in these cases [6].
Thrombosis and thromboembolism are rare in children with UC, but in severe UC patients this should also be expected to initiate treatment with low molecular weight anti-aggregates at the onset of clinical picture.
Copyright: © 2019 Sangita D Kamath., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.