Taslima Akhter1, Nuhad Raisa Seoty2, Mainul Alam Chaklader3, Rabeya Yasmin4, Nawzia Yasmin5, Sk Akhtar Ahmad6 and MH Faruquee4*
1Former Medical Officer, Infectious Diseases Division, International Centre for Diarrhoeal Disease Research, Bangladesh
2Assistant Professor, Department of Public Health, State University of Bangladesh, Bangladesh
3Associate Professor, Department of Community Medicine, Bangladesh Medical College, Bangladesh
4Associate Professor, Department of Occupational and Environmental Health, Bangladesh University of Health Sciences, Bangladesh
5Professor, Department of Public Health, State University of Bangladesh, Bangladesh
6Professor, Department of Occupational and Environmental Health, Bangladesh University of Health Sciences, Bangladesh
*Corresponding Author: MH Faruquee, Associate Professor, Department of Occupational and Environmental Health, Bangladesh University of Health Sciences, Bangladesh.
Received: February 18, 2019; Published: March 04, 2019
Citation: MH Faruquee., et al. “Risk Factors of Respiratory Problems Among Under 5 Children in Bangladesh”. Acta Scientific Paediatrics 2.4 (2019): 03-09.
A large number of under 5 mortality due to acute respiratory infection is preventable and treatable. This cross sectional study was conducted among purposively selected 138 caregivers of under 5 children with respiratory problems prior to attend the study specialized tertiary level hospital in Dhaka. Clinical status of the subjects was assessed using modified scoring method (Wejse C. 2008). The average modified clinical score of the study children was 4.78 ± 1.39. Multivariate adjusted regression analysis revealed that if the family size, sibling sequence and number of person living in same room increased the risk of developing severe respiratory illness; β-coefficient = 13%; 95% CI(4.0%, 23%) (p = 0.005); β = 44%; 95% CI (22.0%, 65.0%) (p < 0.001) and β = 55%; 95% CI (31.0%, 79) (p < 0.001) respectively. Risk of developing severity of illness in the garments workers child was 4.11 times higher compared to day labor father. Multinomial logistics regression revealed that the child had 2.0 and 1.89 times higher risk of getting severe clinical score with the indoor tobacco smoking fume and both tobacco smoking and mosquito coil fume respectively compared to only exposure with mosquito coil fume. The child who visit pharmacy had 4.17 times higher chance to develop higher clinical score (95% CI = 1.28, 7.07; p = 0.005) compared to mild clinical score. Similarly the child who were visited to traditional village doctors and religious spiritual persons had 4.2 (95% CI 1.28, 6.03; p = 0.005) and 2.9 (95% CI = 0.13, 5.61; p = 0.040) times higher risk to develop severe clinical score compared to mild clinical score.
Keywords: Risk Factors; Under 5 Children; Respiratory Problems; Bangladesh
Respiratory tract infections are the most important reason of childhood illness and death in under 5. Annually 12 million children expire before their fifth birthday, several throughout the first year of life in developing countries. Seven out of ten of these diseases are as a result of ‘acute respiratory infections (mostly pneumonia), diarrhea, measles, malaria or malnutrition or a combination of these condition’ [1]. Significant proportions of under-five deaths were from preventable and curable diseases like acute respiratory infections, diarrheal diseases and malaria. By consuming reasonable treatment like antibiotics for acute respiratory infections, oral rehydration therapy for diarrheal diseases and the use of suitable drugs for malaria, many of these lives could save. Though, large numbers of the children expire lacking proper management and before arriving health facility or due to make late for care seeking in developing countries [2]. Among these, respiratory infections divided into upper and lower respiratory infections. Upper respiratory infections include common cold, cough, sore throat, sneezing etc. and lower respiratory infections include pneumonia, bronchitis, Tuberculosis etc. A study from Malawi observed that out of a 1000 admission in the pediatric ward, 298 cases were due to respiratory diseases in children [3]. Respiratory disease remains a major cause of childhood mortality in under five children and 30% of these diseases being acute respiratory infections (ARIs) particularly pneumonia. On an average in Bangladesh, there are seven to nine episodes of ARI experience by a under 5 child every year with duration of 7 to14 days and such cases contribute to 25% of the above deaths [4].
Among these, Pneumonia is one of the most common causes of death in children globally. Pneumonia killed 9, 20136 children of under 5 in the year 2015 and 16% of all deaths of children under five years old, 5% of which are neonatal. Pneumonia is most prevalent in South Asia and sub-Saharan Africa. Immune compromised children are at higher risk of developing pneumonia. A child's immune system may be weakened by malnutrition, particularly in infants who are not exclusively breastfed [5]. In Bangladesh, about 28% deaths occurred because of pneumonia in children of under-five. Nearby 50,000 children die of pneumonia every year worldwide. On an average 80,000 children of under five are admitted to hospital due to virus-associated acute respiratory illness each year.
‘Health seeking behavior is preceded by a decision making process that is further governed by individuals and/or household behavior, community norms, and expectations as well as provider related characteristics and behavior’ [6]. It is recognized that more than 80% of childhood deaths in the developing countries occur at home. To solve such complications, the Integrated Management of Childhood Illnesses (IMCI) strategy was announced by WHO ‘to provide easy, practical and efficient methods of diagnosing and treating childhood illnesses as a way of improving childhood survival’. It has three main components: ‘improved case management by health workers, improved child care at the community level and improvement of the existing health resources’. Attempts are continuing in many parts of the developing world to adjust the guidelines of the IMCI strategy to local applies [7]. There are poor awareness of danger signs or the severity of childhood illnesses in the developing world [8-10]. Health care is sought late for childhood illnesses in most parts of the developing world. Health seeking for childhood illnesses was often delayed more than 24 h after the onset of illness. Most studies on care-seeking for childhood illnesses are community-based [7,11-13].
This cross sectional study was conducted among 138 caregivers of under 5 children with respiratory problems prior attending the study specialized tertiary level hospital in Dhaka during December 2017 to February 2018. Purposive sampling technique was adopted to select the respondents-the caregivers of under 5 children for interview. Data was collected by pre tested interviewer administered semi structured questionnaire and clinical status of the subjects was assessed using modified scoring method (Wejse C. 2008). After collection of data, all responses were checked for their completeness, correctness and internal consistency in order to exclude missing or inconsistent data. Corrected data was entered into computer. The data was analyzed by using the statistical software namely SPSS. Approval from ethical review committee of the State University of Bangladesh (SUB) was taken. Verbal Informed consent was obtained from each respondent before the interview and hearing tests. Respondent’s rights of refuse and withdraw him/herself from the study at any time was ensured. Privacy and confidentiality of the respondents were maintained strictly.
A total of 138 children aged <5 years with respiratory illness attending in tertiary level hospital in Dhaka city were enrolled according to inclusion criteria. The patients were enrolled from Dhaka Shishu Hospital between the periods of 17th December 2017 to 10th February 2018.
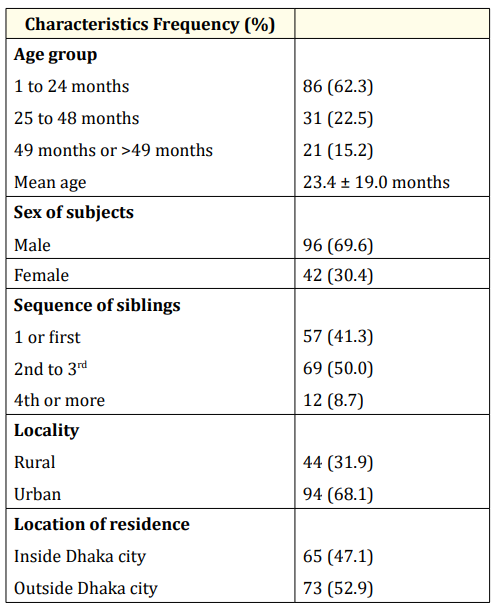
Table 1: Socio-demographic distribution of subjects (n = 138).
In this study, the number of boys was higher than the girls who were 96 (70.0%) boys and 42 (30.0%) girls. The mean age of the study subjects were 23.4 ± 19.0 months and caregiver were 28.25 ± 8.7 years. Majority of the children were within 24 months (62.3%) followed by 25 to 48 months (23%) and 15.2 % were ≥ 49 months. In this study, the number of boys (70.0%) was higher than the girls (30.0%) were girls. It has been reported that 53% study population lived outside of Dhaka city while rest in Dhaka city, but 68% resided in urban area and only 32% in rural areas.
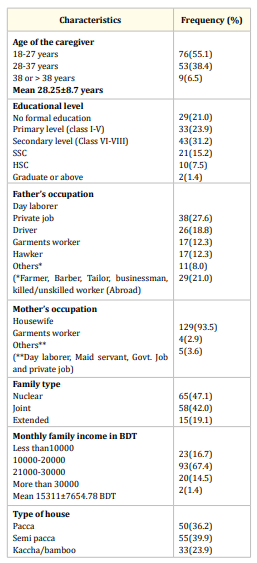
Table 2: Socio-demographic distribution of the respondents (n = 138).
Majority of the reported children’s mothers occupation were housewife 129 (93.0%) followed by garments worker 5 (7.0%). The occupation of the children’s fathers were day laborer 38 (27.6%), private job 26 (18.8%), driver and business man 17 (12.3%), hawker 11 (8.0%) and others 29 (21.0%). Majority of the reported children’s family were nuclear 65 (47.1%) followed by joint 58 (42.0%) and extended 15 (10.9%). The mean household monthly income of the reported families was 15311 ± 7654.78 BDT (min 5000; max 50000). Among the accounted history of education of the children’s caregivers were Secondary levels (Class VI-VIII) 43 (31.2%). Majority of dwelling house was semi pacca 55 (39.9%).
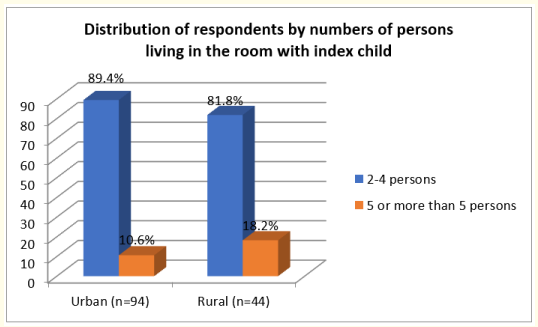
Figure 1: Distribution of respondents by numbers of persons living in the room with index child.
In urban (n = 94), 89.4% of the respondents had 2-4 persons followed by 5 or more than 5 persons were 10.6% and in rural (n = 44), 81.8% of the respondents had 2-4 persons followed by 5 or more than 5 persons were 18.2% living in the room with index child. Mean numbers of persons living in the room with index child was 3.6 ± 0.88 persons.
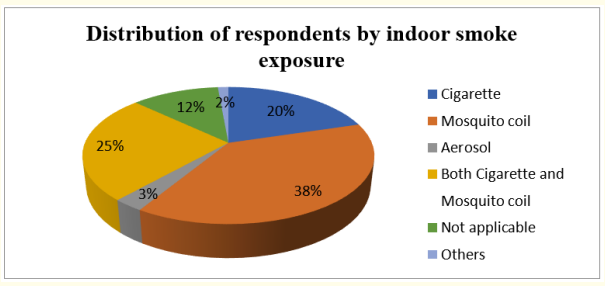
Figure 2: Distribution of respondents by indoor smoke exposure.
In case of indoor smoke exposure, mosquito coil 53(38.4%), followed by both cigarette and mosquito coil exposure 35(25.4%), cigarette 28(20.3%), aerosol 4(2.9%).
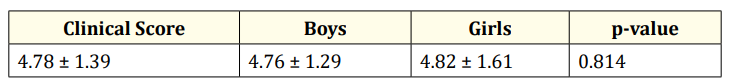
Table 3: Average modified clinical score according to sex.
The average modified clinical score of the study children was 4.78 ± 1.39. No significant difference was found between the boys and girls while clinical score was stratified by sex (p > 0.05).
Multivariate adjusted regression analysis revealed that if the family size, sibling sequence and person lives in a room is increased by 1 person it increased the risk of developing severe respiratory illness; β-coefficient = 13%; 95% CI(4.0%, 23%) (p = 0.005); β = 44%; 95% CI (22.0%, 65.0%) (p < 0.001) and β = 55%; 95% CI(31.0%, 79) (p < 0.001) respectively.
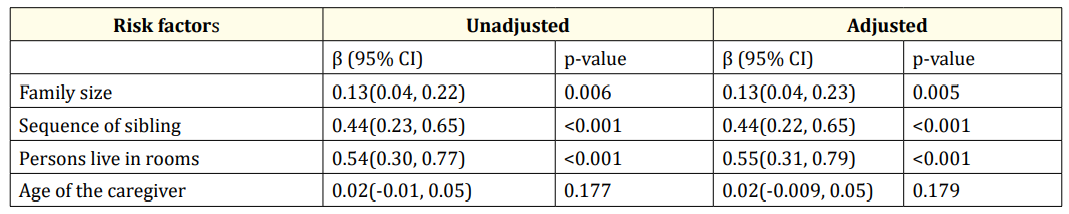
Table 4: Multivariate regression analysis of risk factors with modified clinical score of the study participants.
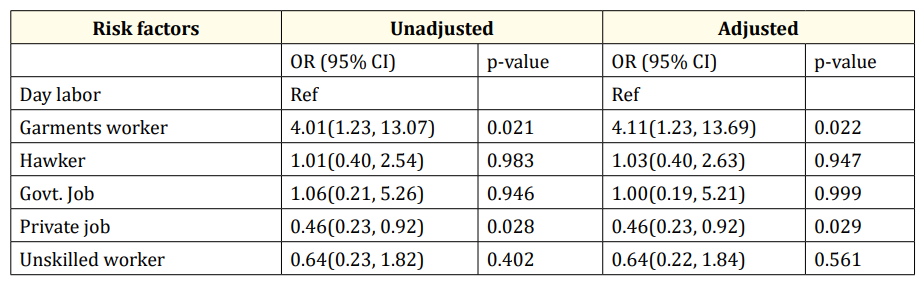
Table 5: Risk of getting higher clinical score in the participant’s father’s occupation compared to day laborer vs. others occupation. The model was adjusted by child age and sex.
The risk of severity of the child in relation to father occupation was estimated by multinomial adjusted logistic regression. Which showed that child of garments worker had higher odds [OR = 4.11; 95% CI (1.23, 13.69); p = 0.022] and private job had less risk [OR = 0.46; 95% CI (0.23, 0.92); p = 0.029] compared to day laborer.
Risk of developing severity of illness in the garments workers child is 4.11 times higher compared to day labor father.
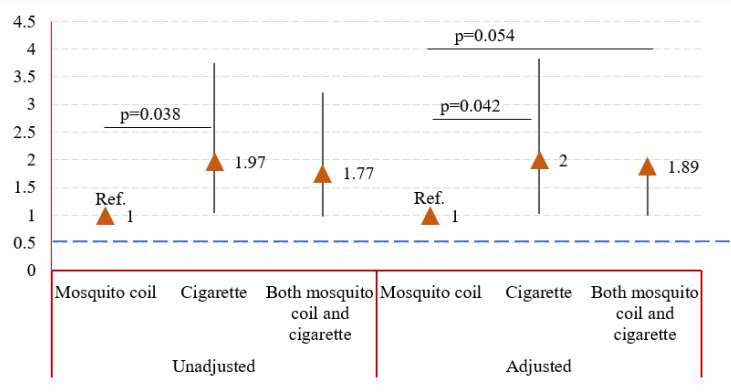
Figure 3: Associated risk factors of indoor smoke on child to getting higher clinical score.
Tobacco smoking exposure was found having higher risk to develop severity of diseases. Multinomial logistics regression revealed that the child had 2.0 and 1.89 times higher risk of getting severe clinical score with the indoor tobacco smoking fume and both tobacco smoking and mosquito coil fume respectively compared to only exposure with mosquito coil fume. The model also showed that the only smoke exposure of cigarette was alone created the risk of higher clinical score.
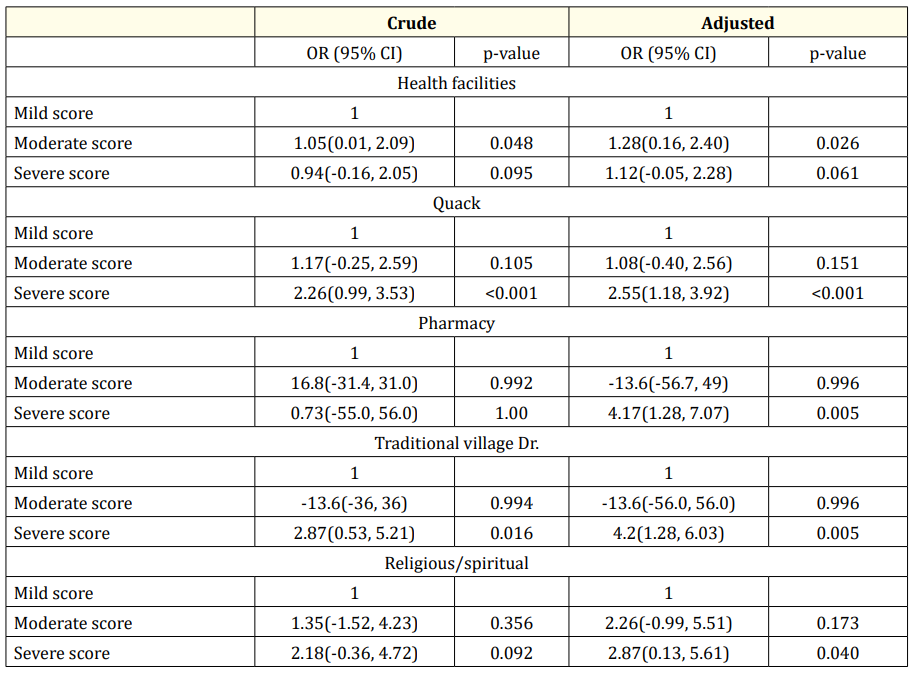
Table 6: Multinomial adjusted regression analysis of factors associated with a child to getting severe clinical score. OR; Odds ratio; CI, Confidence interval
The child who visit Quack, Pharmacy, traditional village doctors and religious or spiritual person were in higher risk to become severe in disease. The children who visit quack were in higher risk of getting severe clinical score [Odds = 2.55; 95% confidence interval = 1.18, 3.92; p-value < 0.001] compared to mild clinical score. The child who visit pharmacy had 4.17 times higher chance to develop higher clinical score (95% CI = 1.28, 7.07; p = 0.005) compared to mild clinical score. Similarly the child who were visited to traditional village doctors and religious spiritual persons had 4.2 (95% CI 1.28, 6.03; p = 0.005) and 2.9 (95% CI = 0.13, 5.61; p = 0.040) times higher risk to develop severe clinical score compared to mild clinical score.
Significant portion of the child deaths in the under-five age group globally were preventable and highest sicknesses such as acute respiratory infection remain to cause childhood mortality even when effective interventions were available to contain them. Timing of health seeking and seek health care to appropriate health providers by caregivers can be a useful tool in dealing with ARI thereby avoiding related complications and mortalities [14].
Our study was conducted in Dhaka city, the capital and largest city in Bangladesh due to financial and time constraints. Dhaka is the 4th most densely populated city in the world with a population of 18.89 million [15]. Dhaka Shishu Hospital (DSH) is the largest children hospital in Bangladesh located at Sher-e-Bangla Nagar, Shyamoli, Dhaka. The number of boys (70%) was higher than girls (30%) in our study which was similar to some studies in Bangladesh [16-18]. The mean age of the subjects was 23.4 ± 19.0 months and that of caregivers was 28.25 ± 8.7 years. Age distribution of the children and caregivers correspondent with a study conducted in rural area and urban slums at Lucknow, India [19]. Main occupation of mother was housewife (93%) and father was day laborer (27.6%) which were relatively comparable to a study in rural Bangladesh where occupation of mother was found housewife in 95.3% cases but occupation of father was agricultural worker/day laborer (31.2%) as that study was community based [20]. Household average monthly income was 15311/tk, common educational status of the caregivers was secondary level (31.2%) which was very nearly similar to a study conducted at Nepal [13]. Contrast result was also found in another study in Nairobi where no education of caregivers were found higher (73.2%) than secondary education (26.8%) [21]. In our study average 5.5 persons lived in each family and average 3.6 persons were living in the room where index child live. Majority of the family was nuclear (47.1%); dwelling house was semi pacca (39.1%). As Dhaka is the largest dwelling place of mosquito, the exposure to mosquito coil was found higher (38.4%) than others.
Multivariate adjusted regression analysis revealed that if the family size, sibling sequence and person live in a room is increased by 1 person; it increased the risk of developing severe respiratory illness. The risk of severity of the child in relation to father occupation was estimated by multinomial adjusted logistic regression which showed that child of garments worker had higher odds ratio and private job had less risk compared to day laborer. Risk of developing severity of respiratory illness in the garments workers child is 4.11 times higher compared to day laborer father.
The child with the exposure of cigarette had higher risk to develop severity of diseases. Multinomial logistics regression revealed that the child had 2.0 and 1.89 times higher risk of getting severe clinical score with the indoor smoke of cigarette and both cigarette and mosquito coil respectively compared to only exposure with mosquito coil. A Vietnamese study of almost 25,000 children less than 5 years of age found that household ETS(Environmental tobacco smoke) exposure to be independently associated with hospitalization for pneumonia [22].
The children who visited Quack, Pharmacy, traditional village doctors and religious or spiritual healers were in greater risk to develop severity in illness compare to health facilities. The children who visit quack were in higher risk to getting severe clinical score compared to mild clinical score. The child who visit pharmacy had 4.17 times higher chance to develop higher clinical score compared to mild clinical score. Similarly the children who were visited to traditional village doctors and religious spiritual persons had 4.2 and 2.9 times higher risk of developing severe clinical score compared to mild clinical score [23,24].
Exposure to indoor tobacco smoking, bigger family size, sibling sequence and increase number of persons living in same room were found higher risk to develop severity of respiratory diseases among the study children. Awareness on risk factors of respiratory diseases along with anti-tobacco campaign especially at home and family planning may improve the situation.
Copyright: © 2019 MH Faruquee., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.