Aman B Pulungan1, Jose RL Batubara1, Bambang Tridjaja1, Frida Soesanti1, Ghaisani Fadiana1, Diadra Annisa2* and Sirma I Mada2
1
Endocrinology Division, Child Health Department, Faculty of Medicine University of Indonesia, Cipto Mangunkusumo Hospital, Jakarta,
Indonesia
2
Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
*Corresponding Author: Aman Pulungan, Endocrinology Division, Child Health Department, Faculty of Medicine University of Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia.
Received: November 05, 2018; Published: January 25, 2019
Citation: Aman Pulungan., et al. “Profile of Diabetic Ketoacidosis in Children with Diabetes Mellitus in a Tertiary Care Hospital in Jakarta: A Retrospective Study”. Acta Scientific Paediatrics 2.2 (2019):24-29.
Introduction: Diabetic ketoacidosis (DKA) is a leading complication of Diabetes Mellitus (DM), especially type-1 Diabetes Mellitus which mostly affects children. DKA recurrence was frequent and mortality was associated with number of hospital admission of DKA. In Indonesia, there is a lack of clinical and biochemical characteristics in these patients. Our aim is to describe the clinical and laboratory data of DKA in DM children.
Methods: We reviewed 16 cases of 12 children aged 0-18 years diagnosed with DKA and DM retrospectively in Cipto Mangunkusumo Hospital, from January 2017-October 2018. Medical history and laboratory data were obtained. DKA was classified into mild, moderate, and severe based on pH and HCO3 levels. Data was analyzed with SPSS.
Results: Sixteen cases from 12 children with DKA were obtained. The median age was 14 (0-16) years. Only four patients had a family history of DM. Four patients (4/16) had first onset of DKA, and twelve cases had histories of previous DKA. More than half of the cases had classical symptoms of DM (11/16), dyspnea (11/16), and nausea or vomiting (9/16). The average length of stay was 3.5 (1-17) days; one patient was an infant with comorbidities thus needing longer care. Most subjects had severe DKA (8/16). Mean blood glucose and HbA1c levels at arrival were 692.49 (303-1113.6) g/dL and 12.04 (6.8-16.7)%, respectively. Hypernatremia and hypokalemia were the most common electrolyte abnormalities. Leukocytosis was found in most patients. The average starting and maximum insulin dose was 0.05 (0.05-0.1) IU/kg/hour and 0.1 (0.05-3) IU/kg/hour, respectively. DKA resolution was 28.8 ± 14.5 hours, while length of stay was 3.5 (0-17) days. All patients recovered from DKA, there were no deaths.
Conclusion: The number of DKA recurrence in previously diagnosed DM patients remains high. Poor compliance due to lack of knowledge in the patient and caregivers contributes to DKA recurrence. Proper application of treatment protocol with low dose insulin is effective to lower mortality. More effort is needed to prevent DKA by ensuring that patients and caregivers are well educated on long term care of DM.
Keywords: Diabetic; Children; Cipto Mangunkusumo; Jakarta
The incidence of Diabetes Mellitus (DM) in children and adolescents is rising. Up to 2018, the registry of the Indonesian Pediatric Society (IPS) recorded 1194 cases of Type-1 DM (T1DM) in pediatric patients. The incidence rate of pediatric T1DM in Indonesia increased sevenfold over the course of 10 years; 3.88 per 100 million to 28.19 per 100 million population in 2000 and 2010, respectively [1]. Other types of DM, such as T2DM or monogenic diabetes are still poorly registered in Indonesia. Hence, the existing data on DM in children is only the tip of an iceberg; the real incidence is predicted to be much higher.
Diabetic ketoacidosis (DKA) is the most common complication of DM, especially T1DM. Based on the IPS registry, DKA occurs in 60.56% T1DM children and adolescents in 2012 [1]. Severe deficiency of insulin causes metabolic abnormalities: hyperglycemia, metabolic acidosis, ketonemia, dehydration, and electrolyte imbalance. These abnormalities manifest through clinical manifestations of dehydration, tachycardia, tachypnea, kussmaul breathing, breath smells of acetone, nausea, vomiting, abdominal pain, blurry vision, and loss of consciousness ranging from confusion to coma [2].
Risk factors for DKA are different between newly diagnosed and previously known diabetic patients. In newly diagnosed patients, risk factors include younger age, delayed diagnosis, lower socioeconomic status, and domicile in countries with low prevalence of T1DM. Meanwhile, in previously known DM patients, DKA risk increases in children with insulin cessation, poor metabolic control, previous history of DKA, gastroenteritis, psychiatric disorders, family problems, limited access to medical services, alcohol consumption, and in peripubertal and adolescents [2].
DKA recurrence is often a challenge in treating DM children; mortality is associated with the number of hospital admission for DKA [3]. Previous studies have shown that the frequency of DKA recurrence was significantly higher in patients with poor glycemic control, reflected by higher HbA1C level and insulin treatment omission [4,5]. Diabetes knowledge is one of the keys to achieve glycemic control. A study by Martin., et al. [6] about diabetes knowledge in adolescents with T1DM determined that diabetes knowledge and skills score was significantly higher in patients with HbA1C below 8% compared to patients with higher HbA1c levels.
Due to the large variation of clinical characteristics and outcomes of DKA worldwide, this study aims to analyze the profile of DKA in the Indonesian population, specifically in Cipto Mangunkusumo Hospital (CMH), Jakarta. Identification of risk factors is needed for evaluation of therapy and preventive measures to reduce DKA rates.
This descriptive retrospective study was conducted by reviewing medical records of children aged 0-18 years hospitalized for DKA in Cipto Mangunkusumo Hospital (CMH), Jakarta, from January 2017 until October 2018. Characteristics of patients, medical history, laboratory data, and insulin use were recorded.
Medical history included age of DKA onset, DKA recurrence, symptoms, time of DKA resolution, length of stay in the hospital, occurrence of cerebral edema, and outcome. DKA resolution was based on the time until the patient received subcutaneous insulin, while outcome was based on death or discharge. Cerebral edema was defined as receiving mannitol.
DKA was defined based on the 2018 ISPAD criteria: hyperglycemia (blood glucose >200 mg/dL), venous pH <7.3 or serum bicarbonate <15 mmol/L, and ketonemia or ketonuria [2]. The severity of DKA was classified according to the ISPAD 2018 guideline; (1) mild (pH <7.3 or bicarbonate <15 mmol/L), (2) moderate (pH <7.2 or bicarbonate <10 mmol/L), and severe (pH <7.1 or bicarbonate <5 mmol/L) [1]. Electrolyte levels were also assessed [2]. Based on the reference range used in CMH, hypokalemia was defined as serum potassium <3.3 mEq/L, hyperkalemia: serum potassium >5.4 mEq/L, hyponatremia: serum sodium <132 mEq/L, and hypernatremia: serum sodium >147 mEq/L. Definition of leukocytosis was white blood cell count >10,000/L [7].
Data were analyzed using SPSS (Version 20 for Mac) for statistical analysis. The mean (± standard deviation) or median (minimum – maximum) was calculated based on data normality which used the Shapiro-Wilk Test.
Sixteen cases out of 12 patients were reviewed. The median age was 14 (0-16) years, the majority of subjects were adolescents (10/12). Subjects were mostly diagnosed with DM at a young age (0-4 years; 4/12) or at adolescence (10-14 years; 5/12). Most patients (9/12) were diagnosed with T1DM, while other less common types included neonatal DM and drug-induced DM; two patients who were on leunase developed DKA. All patients were insulin-dependent. The ratio of girls: boys was 1.4:1. Family history of DM in the family was uncommon, two patients had history of T1DM and two of Type-2 Diabetes Mellitus. Almost all patients (9/12) resided in Jakarta and surrounding areas (Depok, Bogor, Tangerang, Bekasi). All patients were funded by the Indonesian National Health Insurance. The characteristics of subjects in the study can be seen in table 1.
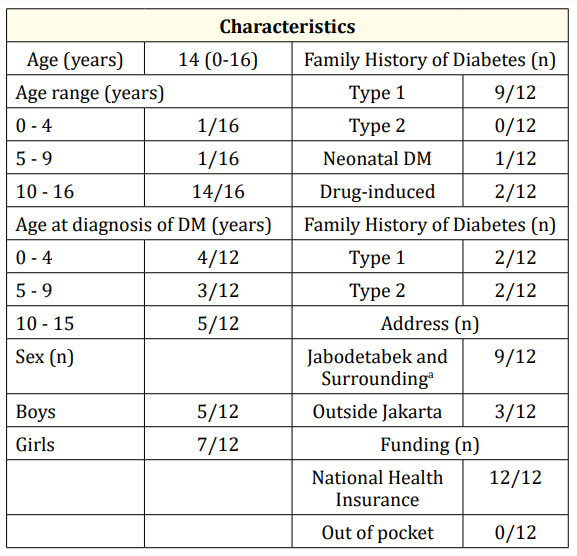
Table 1: Characteristics of Subjects.
Table 2 describes the medical history of the patients. Twelve out of 16 patients had history of DKA. Four patients had the first occurrence of DKA, three among them had DKA at presentation of DM. The highest number of DKA recurrence was 11 times, which was a teenage girl with poor treatment adherence and lack of knowledge in the patient and caregivers. The highest DKA precipitating factors were poor compliance (10/16), followed by infection (2/16), and fasting (1/16). The most common symptoms were classical symptoms (polyuria, polydipsia, polyphagia), dyspnea, and nausea or vomiting with a proportion of 11/16, 11/16, and 9/16, respectively.
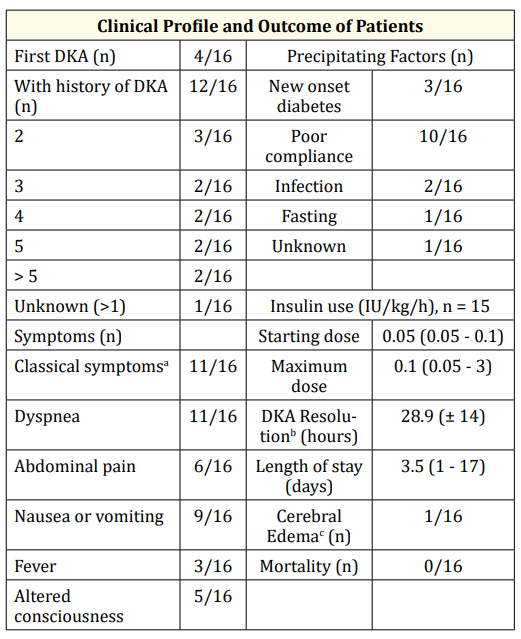
Table 2: Clinical Profile and Outcome.
aClassical symptoms: polyuria, polydipsia, polyphagia, bDKA resolution: time until pasien received SC insulin, c cerebral edema: administered mannitol.
Table 3 shows the laboratory trends in DKA patients. The median of blood glucose at arrival was 692.49 (303-1113.6) g/dL, while HbA1c was 12.04 (6.8-16.7)%. Based on pH levels, five (5/16) patients were classified as mild DKA, three (3/13) as moderate, and eight (8/16) as severe. Hyperkalemia (5/16) and hyponatremia (5/16) were the most common electrolyte abnormalities. Almost all subjects (14/16) had leukocytosis (21,948.13/L ± 14,068.63); two patients without leukocytosis were diagnosed with leukemia and were on chemotherapy at the time of examination. The average blood ketones level in 14 cases was 3.36 (±1.11). Blood ketones level was not measured in two patients because of reagent unavailability.
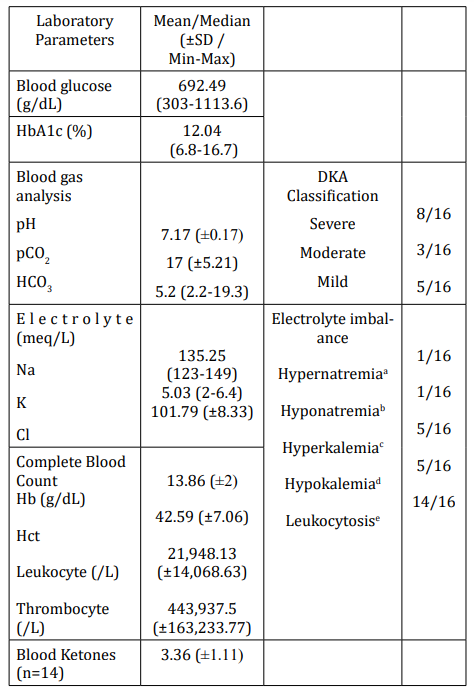
Table 3: Laboratory Trends on Admission. aHypernatremia: Serum Na >147 mEq/L, bHyponatremia: Serum
Na <132 mEq/L, chyperkalemia: Serum K >5.4 mEq/L, dHypokalemia: Serum K <3.3 mEq/L, eleukocytosis: >10.000/L.
One patient was discharged against medical advice after three hours in the emergency room and was not included for insulin and DKA resolution analysis. Table 2 shows the insulin use and DKA resolution. The median starting dose was 0.05 (0.05-0.1) IU/kg/ hour, while the maximum dose was 0.1 (0.05-3) IU/kg/hour. DKA resolution was 28.9 (±14) hours. Insulin use and DKA resolution can be seen in Table 2.
Table 2 presents the length of stay, occurrence of cerebral edema, and mortality. The median length of stay was 3.5 (1-17 days). One patient was a neonate with comorbidities needing 17 days of care. Cerebral edema occurred in one patient from admission to the hospital. All patients were discharged and none died.
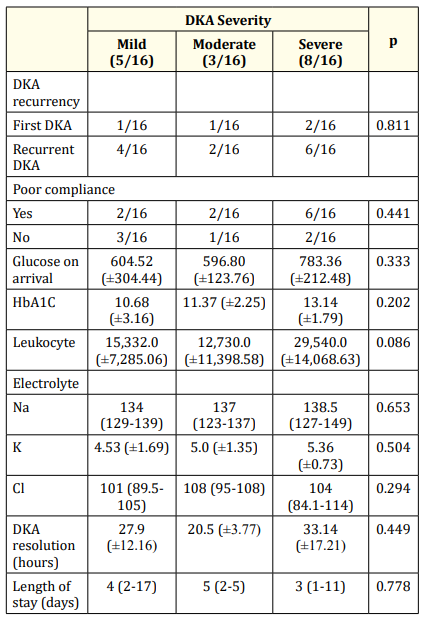
Table 4: Association of DKA severity with clinical and laboratory parameters.
DKA is a main cause of mortality in DM patients. In this study, T1DM is the most common type of DM in children aged 0-18 years. The median age of patients in this study was 14 (0-16) years; thus, teenagers were at most risk of developing DKA. A previous research conducted in Saudi Arabia found a lower median age, 11 years (813) [8]. Studies in India [9,10] reported a median and mean age of 7.52 (2-14) and 11.4 ± 4,4 years respectively, also lower than this study. The relatively higher median age of patients in this study is in accordance to the observed higher prevalence of T1DM among children aged 10-14 years according to the IPS registry [1]. Different population may affect the different age range of DKA and DM.
We found that frequency of DKA is slightly higher in girls compared to boys (1.4:1); in contrary to previous studies which found that DKA frequency was higher in boys [6]. A previous study by Pulungan., et al. [11] conducted in CMH reported similar but more dramatic results, with ratio of female:male reaching 17.5:1. Female predominance was also found among DKA patients in a study by Onyiriuka and Ifebi [12] with a female-to-male ratio of 1.5:1. This finding may be caused by hormonal changes in puberty, especially the raising of counter-regulatory hormones, such as growth hormone and estrogen. The decrease in circulating insulin accompanied by elevation of counter regulatory hormones may elicit DKA. The hormonal changes occur differently between boys and girls; serum level of estrogen in girls is greater than boys at puberty [12].
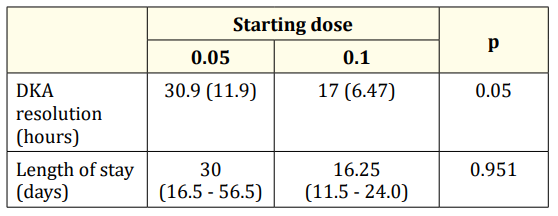
Table 5: Relationship of starting dose with DKA resolution and length of stay.
The most common precipitating factor of DKA was due to compliance problems. Similarly, Naeem., et al. [4] also found that non-compliance to insulin high (79%) in children with DKA in Saudi Arabia. Lack of parental knowledge on T1DM treatment plays a major role in non-compliance, causing insulin omission or failure to routinely visit the physician for insulin adjustment. Most patients who presented with DKA at CMH had previous history of DKA; and lack of knowledge was a main problem. Many studies mentioned that recurrence of DKA was associated with diabetes knowledge and level of socioeconomic status [12]. It was reported by Vanelli M., et al. [13] about DKA prevention program in Parma, Italy, that raising awareness and improving knowledge through dissemination of information about diabetes mellitus could significantly reduce prevalence of DKA at type 1 DM from 78% to 12.5%. This finding proves that knowledge is one of the main factor in preventing DKA.
In this study, we found that patients who had DKA reoccurrence due to poor compliance were all female adolescents (≥10 years old). Few reasons for insulin omission were psychological stress (e.g. breaking up with a boyfriend), social reasons (e.g. not taking insulin shots during a sleepover), and mostly due to lack of knowledge. Consistent with the present study, Malik., et al. [14] in the United States reported that older children and females had higher risk of frequent DKA admission. Rewers., et al. [15] implied that the increase of DKA frequency in teenage girls might be affected by body image (skipping insulin to loose weight), increased insulin resistance in puberty or obesity, and eating disorders. Adolescents with DM are at risk of poor insulin compliance, thus needing special attention. An integrated interdisciplinary diabetes care team, comprised of pediatric endocrinologists, psychologists, psychiatrists, and social workers are needed to ensure optimal treatment and preventing DKA [16].
Other precipitating factors found in this study were new onset diabetes, infection, fasting without insulin adjustment, and unknown causes. Indonesia is Muslim-majority country and many adolescents with DM choose to fast during Ramadan. Pre-Ramadan medical assessments, insulin regimen modification, close monitoring, and a detailed medical education are crucial strategies to prevent DKA and DM complications [17].
The leading DKA symptoms were classical DM symptoms, dyspnea, and nausea or vomiting. This result is in line with previous studies [4,5,11]. Symptoms of DKA often mimics other acute illnesses, causing delayed diagnosis especially in patients with new onset DM. This delay was found to significantly increase mortality [18]. Increasing physician and public awareness is important to prevent delay in diagnosis of DKA.
We observed that half of the patients in this study were classified as severe DKA (8/16). In accordance to this finding, Kanwal., et al. [19] in India found that severe DKA occurred in 61.8% in children with T1DM. Leukocytosis is a hallmark of DKA’ in the present study, marked leukocytosis occurred in almost all patients with an average of 21,948.13/L. A previous study by Xu., et al. [20] found that DKA severity is significantly associated with higher leukocyte count due to leukocyte production and release with increased H+.
The mean blood glucose at arrival reached 692.49 (303-1113.6) g/dL, this is consistent with the result that the majority of patients in this study had severe DKA. Mean HbA1c was high, reaching 12.04% (6.8-16.7%), showing poor glycemic control in this group of patients. Karges B., et al. [21] stated highest DKA rates were observed in subjects with HbA1C ≥9.0% and increasing HbA1C was associated with a higher ketoacidosis rate. Blood ketones level is an important laboratory parameter to diagnose DKA [22]. In this study, blood ketones level could not be measured in two patients because the reagent was temporarily out of stock. This reflects one of the many challenges of DKA treatment in Indonesia, where resources for laboratory examinations are often limited or even unavailable especially in rural areas; hence, the application of international standards can be difficult. Capillary beta-hydroxybutirate, although important for monitoring of DKA resolution [3,23], is not routinely measured in children with DKA in CMH. Its use is still not common nationwide.
The median starting dose was 0.05 IU/kg/hour. According to the ISPAD 2018 guideline, a low starting dose of 0.05 IU/kg/hour was safe and effective compared to higher doses [2]. DKA resolution was 28.8 ± 14.5 hours, concordant with findings by Lone., et al. [24] which reported the duration of IV insulin switched to subcutaneous in T1DM children was 27.5 ± 14.1 hours. Length of stay in the hospital was longer, with a median of 3.5 days. An extended length of stay is needed to educate caregivers on long-term care of children with DM, including the importance of medication adherence.
The occurrence of cerebral edema was low (1/16) and the mortality rate was zero; all patients were discharged. A study by Pulungan., et al. [11] which also assessed pediatric DKA in CMH from 2006-2011 found that one patient died in the first three hour of care due to cerebral edema. This finding implies that DKA care in CMH has improved and may be due to application of a proper DKA protocol. A national DKA guideline adjusted to fit local conditions is an important tool to optimize DKA care. In 2017, the Indonesian Pediatric Society renewed the DKA clinical practice guideline.
The occurrence of cerebral edema was low (1/16) and the mortality rate was zero; all patients were discharged. A study by Pulungan., et al. [11] which also assessed pediatric DKA in CMH from 2006-2011 found that one patient died in the first three hour of care due to cerebral edema. This finding implies that DKA care in CMH has improved and may be due to application of a proper DKA protocol. A national DKA guideline adjusted to fit local conditions is an important tool to optimize DKA care. In 2017, the Indonesian Pediatric Society renewed the DKA clinical practice guideline.
A few limitations of this study include low number of samples and the use of secondary data from medical records. The prevalence of DKA was also not assessed. A cohort study with greater number of subjects is needed to provide better information on DKA in the Indonesian pediatric population.
DKA is a serious and life-threatening event. Recurrence of DKA remains high, especially in adolescents. Prevention of DKA must be a main concern of healthcare workers. We found no significant association between DKA severity and DKA recurrence, but this study included only a small number of sample. An integrative and multidisciplinary team must ensure that patients and families are well educated on the long term care of T1DM.
Copyright: © 2019 Aman Pulungan., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.