Sachin KR1*, Nagamani Agarwal2 and Vinay KM3
1 Junior Resident, Department of Paediatrics, JJM Medical College, Davangere, Karnataka, India
2 SProfessor, Department of Paediatrics, JJM Medical College, Davangere, Karnataka, India
3 Junior Resident, Department of Paediatrics, JJM Medical College, Davangere, Karnataka, India
*Corresponding Author: Sachin KR, Junior Resident, Department of Paediatrics, JJM Medical College, Davangere, Karnataka, India.
Received: January 17, 2019; Published: January 24, 2019
Citation: Sachin KR., et al. “Herbst’s Triad - A Rare Case Report ”. Acta Scientific Paediatrics 2.2 (2019):21-23.
Gastroesophageal reflux with or without hiatus hernia associated with finger clubbing, hypoproteinemia and iron deficiency anemia is known as Herbst’s triad. Herbst’s triad, Sandifer syndrome (reflux esophagitis, iron deficiency anemia and head cocking) and Rumination syndrome are rare presentations of GERD. We report a case of Herbst’s traid in a 13 year old adolescent male suffering from GER with hiatus hernia, persistent severe iron deficiency anemia, finger clubbing and hypoproteinemia who remained undiagnosed because of complex clinical picture. Following surgical correction of hiatus hernia, GER and other associated symptoms promptly regressed.
Keywords: Herbst’s Triad; Gastroesophageal Reflux; Hypoproteinemia; Clubbing
The association of Gastroesophageal reflux with or without hiatus hernia with finger clubbing, hypoproteinemia and iron deficiency anemia is rare and is known as Herbst’s triad. Only sporadic cases of Herbst’s traid have been reported in the literature and there is a lack of awareness of this condition. We report a case of Herbst’s triad in a 13 year old adolescent male who presented with severe anemia, clubbing and bilateral pitting pedal edema.
A 13 year old adolescent male presented with complaints of generalized weakness, effort intolerance, puffiness of face and edema of feet and decreased appetite of one month duration. There was no history of icterus, decreased urine output or change in urine colour. There was history of recurrent respiratory tract infections from early childhood. He also complained of recurrent episodes of pain in the epigastric region associated with retrosternal burning sensation. He was transfused thrice with packed red blood cells in the last three years in view of severe anemia. On examination his height and weight were less than 3rd percentile on WHO growth charts. There was significant pallor with grade 3 clubbing in both upper limb and lower limb with puffiness of face and bilateral pitting pedal edema. His blood pressure was 120/60 mm of Hg. Systemic examination revealed hemic murmur and tenderness in epigastrium. There was no organomegaly.
Investigations revealed severe anemia (Hb -4.5gm/dl), decreased reticulocyte count and increased red cell distribution width. Peripheral blood smear revealed microcytic hypochromic anemia. Iron studies were suggestive of Iron deficiency anemia. Serum total protein and albumin were 4.1gm/dl and 1.6 gm/dl respectively. Stool was positive for occult blood. Chest X ray revealed no radiological abnormality. Barium meal study showed normal study. Upper GI endoscopy showed grade 2 hiatus hernia with grade A reflux esophagitis. Duodenal biopsy showed normal histopathology. ATTG (anti tissue transglutaminase) antibody was within normal limits. Rapid urease test for Helicobacter pylori was negative. Bone marrow biopsy (done during previous admissions) showed micronormoblastic bone marrow with grade 1 iron stores on Perl’s stain.
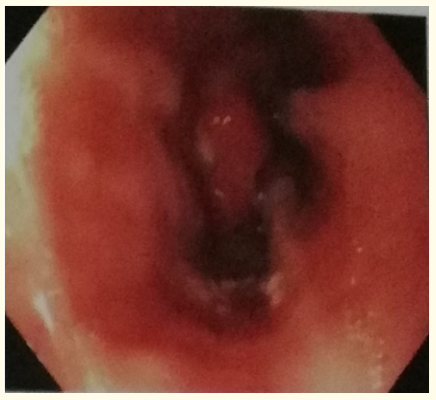
Figure 1: Upper GI endoscopy showing OG junction with hiatus hernia.
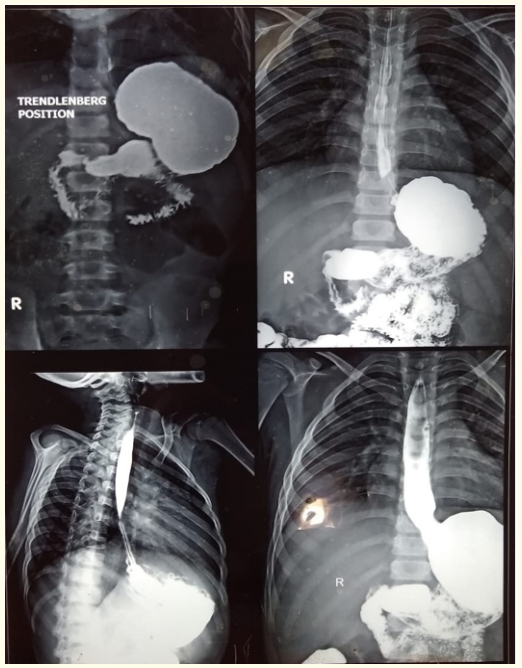
Figure 2: Barium meal study shows normal anatomy of GI tract.

Figure 3: Grade 3 clubbing.
Gastroesophageal reflux is known to be a cause of disorders eg, chronic pulmonary disorders [2] and sudden infant death syndrome [3] and a consequence of underlying diseases eg, esophageal atresia [4] and mental retardation [5]. GER may be found with associated lesions eg, in patients with cow’s milk protein allergy [6], torticollis [7], cystic fibrosis [8] and congenital heart disease [9].
In 1976, Herbst., et al. [1] reported three cases of GER with protein-losing enteropathy, finger clubbing, and iron deficiency anemia. One of these patients presented with cocking of the head. This abnormal posturing has been attributed to an attempt to decrease the pain of esophagitis resulting from GER [10]. The relationship between iron deficiency anemia and esophagitis is well known, as all gastrointestinal diseases with a mucosal damage may provoke this form of anemia. Chronic pulmonary diseases associated with gastro esophageal reflux may explain the presence of clubbing. Functional stenosis or decreased clearance of the esophagus may provoke stasis followed by bacterial contamination of the gut that would lead to alteration of the intestinal mucosa with resulting protein loss and hypoproteinemia causing pitting pedal edema.
Our patient had all the clinical features of Herbst traid. He had iron deficiency anemia, grade 3 clubbing of both upper limb and lower limb, hypoprotienemia with generalized edema. He presented with severe anemia, recurrent episodes of epigastric pain abdomen and respiratory illness. He was treated with PRBC transfusion and other symptomatic measures during previous admissions. Because of lack of awareness about the underlying condition, definitive treatment could not be given. Repeated admissions for similar complaints made us to suspect Herbst triad. Upper GI endoscopy showed Hiatus hernia and reflux esophagitis. Child underwent surgical correction for hiatus hernia following which GER and related symptoms regressed promptly. Follow up an year later showed, finger clubbing had totally vanished and serum protein and serum iron levels were within normal range.
In our case, correlating both clinical and laboratory findings (present and past), child is having refractory iron deficiency anemia, grade 3 clubbing of both upper limb and lower limb, hiatus hernia of grade 2. The child was diagnosed to have Herbst triad for which child went surgical correction for hiatus hernia which is the definitive treatment following which child showed symptomatic improvement. At the end of 1 year follow up, finger clubbing had totally vanished and normalization of serum protein and serum iron levels have been observed.
Nil
Nil
Nil
Copyright: © 2019 Sachin KR., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.