Singh Sunita*, Rawat Jiledar, Panday Anand
Pediatric Surgery Department, CSM Medical University, Lucknow, India
*Corresponding Author: Sunita Singh, Pediatric Surgery Department, AIIMS, Raipur, India.
Received: December 05, 2018; Published: January 23, 2019
Citation: Singh Sunita., et al. “Acute Spontaneous Scrotal Haematoma in an Infant: Manifestation of Late-Onset Vitamin K Deficient Bleeding Disorder ”. Acta Scientific Paediatrics 2.2 (2019):18-20.
Spontaneous scrotal hematoma is a very rare but, essential differential diagnosis of acute scrotum in infant. This entity is important because it does not needs surgical intervention. We report a 5-month-old male child who presented with spontaneous scrotal hematoma. The probable cause of bleed was late onset vitamin k deficient bleeding disorder; as it the most common cause of bleeding diathesis in developing countries; especially who are exclusively breast feed and in whom no vitamin K prophylaxis given at birth. Other similar cases of scrotal hematoma reported in literature were either associated with neonatal adrenal hemorrhage or as an extension of retroperitoneal hematoma.
Keywords: Acute Scrotum; Late Onset Vitamin K Deficient Bleeding Disorder (VKBD); Testicular Torsion; Scrotal Haematoma
Acute scrotum is a paediatric emergency; however, surgical exploration in all such cases remains controversial [1-6]. Scrotal swelling with discoloration of scrotal wall suggests is neonatal torsion unless proved otherwise [1-3]. Spontaneous scrotal haematoma (SSH) is a very rare but essential differential diagnosis of acute scrotum. It is often missed by treating physician. Scrotal haematoma in infants reported in literature usually arises due to local trauma, intra-abdominal bleeding and abdominal trauma [2-6]. We report SSH as an extremely rare presentation of vitamin k deficient bleeding disorder (VKBD), which is itself a common problem in the developing world [7].
A 5-month-old male child presented to us with acute onset swelling of the right inguinoscrotal region. This was associated with mottling, bronzing and reddish brown discoloration of overlying skin. There was no history of local or abdominal trauma, fever, vomiting or abdominal distension. The baby was delivered at home and vitamin K was not administered as prophylaxis at birth.
On examination, the infant was irritable, pale and having tachycardia. There was neither manifestation of bleeding anywhere in the body, nor signs of strangulated inguinal hernia. The swelling was non tender, of normal temperature. Discoloration was extending slightly in right inguinal and perennial region (Figure 1). The right testis could not be palpated separately. The examination of the abdomen was normal.

Figure 1: Acute onset inguino-scrotal wall discoloration (note there was no abdominal distension).
The baby was resuscitated, and prophylactic vitamin K was administered intramuscularly. The hemogram revealed severe anemia. The baby was planned for colour Doppler study of scrotum to rule out torsion testis and abdominal ultrasonography, but it was not feasible due to poor general condition of the baby. As 12 hours had already passed before the patient presented to us, we operated upon him to rule out testicular torsion.
On scrotal exploration, we noticed huge haematoma within both the scrotal walls (Figure 2). It was associated with devitalisation of overlying skin, but the testes of both sides were normal. The haematoma was evacuated, and debridement of the dead tissue was done. On retrograde questionnaires, there was no family history of any bleeding disorder or any unusual bleeding since birth. In postoperative period baby coagulation profile showed markedly raised partial thromboplastin (PT) and activated partial thromboplastin time (aPTT). The history of exclusive breast feeding raised aPTT and PT, no vitamin K prophylaxis at birth along with the surgical finding in an otherwise normal healthy baby pointed towards the late-onset-VKBD to be the probable cause of bleeding. To confirm the diagnosis, the serum level of “proteins induced in vitamin K absence” (PIVKA-II) was planned but, the baby expired before sample collection. Hence, we could not investigate further on the line of definitive cause of bleeding disorder. The probable cause of death was huge intracranial bleeding as evident by neurological features ( rigidity, unequal pupil size, tense anterior fontanelle and focal seizers) after few hours of surgery. Intracranial bleeding is the most common manifestation of late-onset-VKBD.
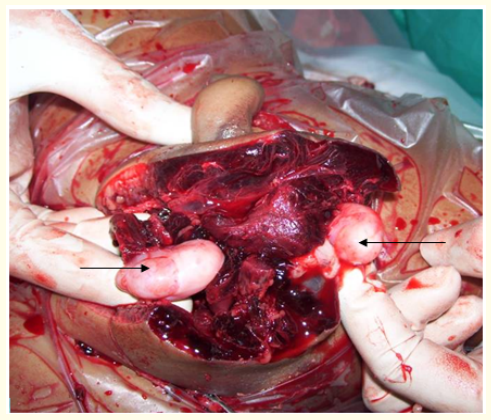
Figure 2: Peroperative photograph after debridement showing bilateral normal testis (pointed by arrows).
In infants, the scrotal swelling can arise in various conditions such as torsion of the testis, torsion of appendages, epididimo-orchitis, scrotal or testicular edema, hydrocele, strangulated inguinal hernia, meconium peritonitis with periorchitis, hematocele, pyocele, testicular tumour, and scrotal wall hematoma [1]. Out of these testicular torsion, strangulated hernia and pyocele need surgical intervention [1,4,5].
Clinically, a hematoma appears as a scrotal swelling with bluish discoloration of the skin [1,5,6]. Scrotal haematoma due to intraabdominal bleeding and abdominal trauma can reach the scrotum either through a patent processes vaginalis or by the retroperitoneal route, dissecting along the retro peritoneum [2,5,6]. The risk factors for neonatal SSH associated with adrenal hemorrage are evidence of bleeding diatheses or maternal gestational diabetes [5].
The scintigraphy is the procedure of choice in the evaluation of testicular perfusion but, facility is not available everywhere [8]. Most of the developing countries still rely on Doppler ultrasonography (DUS). The role of DUS in the small prepubertal testis has been regarded as inconsistent as vascular impedance of the intratesticular vessels tends to remain high until puberty, when diastolic flow increases, however, clue to the torsion of testes are asymmetry in size and echo texture [8,9]. Further, in asymptomatic prepubertal testis, absence of flow usually results from insensitivity of ultrasound equipment for low flow, inappropriate technical factors such as low transducer frequency, low gain, high pulse-repetition frequency or high wall filter, rather than intrinsic testicular defects [8,9]. Because of above mentioned reasons and late (12 hours) presentation of baby, we decided to explore the scrotum to salvage the testis from torsion testis or something else. Bedside abdominal USG by surgeon was done in post operative period to look for the presence of adrenal hemorrhage, but finding were normal [2-6].
In modern era of evidence based surgery, we were not confirmed of etiology of bleeding disorder; however, we believe that probable cause was late-onset VKBD because among other causes of bleeding in otherwise healthy infant (isolated coagulation disorder, immune thrombocytopenia, hereditary clotting factor deficiencies, occult infectious thrombosis, thrombosis, bone marrow hypoplasia and bone marrow infiltrative disease) none were found [10].
VKBD is typically described as a “well baby with bleeding” [10]. It is a syndrome defined as unexpected bleeding attributable to severe vitamin K deficiency in infants 2 to 12 weeks of age. It occurs primarily in exclusively breastfeed infants, who have not received adequate neonatal vitamin K prophylaxis [7,10]. Late-onset VKBD is more severe than early onset or classical disease [10]. The most common presentation of late-onset VKBD is intracranial haemorrhage in infants, that was the probable reason of expiry of baby, as there was unequal sluggish reacting pupils with tense fontanella and focal convulsion in postoperative period [10].
To conclude, SSH as a bleeding manifestation of VKBD is an extremely uncommon entity and has never been reported in the literature. It needs to be included in the differential diagnosis of acute scrotum with proper management to salvage the patient.
Nil
Nil
Copyright: © 2019 : Singh Sunita., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.