Adriane Muller Nakato1*, Valéria Cabral Neves Luzcynski1, Cristina Okamoto2, Mônica Nunes Lima Cat1, Regina PGV Cavalcante da Silva1 and Nelson A Rosario Filho1
1 Department of Pediatrics, Hospital de Clínicas, Federal University of Paraná, Curitiba, Brazil
2 Department of Pediatrics, Universidade Positivo – Rua Professor Pedro Viriato Parigot de Souza, Curitiba, Brazil
*Corresponding Author: Adriane Muller Nakato, Department of Pediatrics, Hospital de Clínicas, Federal University of Paraná, Curitiba, Brazil.
Received: January 08, 2019; Published: January 22, 2019
Citation: Adriane Muller Nakato., et al. “End-Tidal Carbon Dioxide as a Predictor of the Success of Extubation in Preterm Infants”. Acta Scientific Paediatrics 2.2 (2019):03-07.
Objective: This study aimed to identify the chance of success of extubation by analyzing EtCO2 levels and if this can be a predictor of the success of extubation in preterm infants.
Methods: This was conducted to verify the efficacy of capnometry in 43 premature infants admitted to the Neonatal Intensive Care Unit (NICU) at the Hospital de Clínicas, Federal University of Paraná, Curitiba, Brazil from August 2014 to December 2015. EtCO2 levels were compared with PaCO2 levels, in ventilated premature with and without DPLD. Both parameters were obtained daily until tracheal extubation. The correlation coefficient and degree of bias was adjusted by grouping the preterm infants by gestational age and pulmonary disease.
Results: Pearson’s correlation showed significant correlation in all groups, although higher in preterm infants without pulmonary disease and gestational age greater than 32 weeks (n = 43; r = 0.98; p < 0.0001). The ROC curve shows that EtCO2, in the cutoff point 42 mmHg had 100% sensitivity and 78.3% specificity, with a safe probability of success of extubation. The points above 50 mmHg have a sensitivity of 60% and a specificity of 82.6%, reducing the chances of success.
Conclusions: The data suggest that EtCO2 is a parameter in predict success extubation in premature infants. In addition, reduce blood loss and pain in these premature infants.
Keywords: Capnometry; Mechanical Ventilation; Blood Gas Analyses; Hypercapnia; Premature Infants; Respiratory Insufficiency
End-Tidal Carbon Dioxide (EtCO2 ) is a continuous and non-invasive technique monitoring by capnometry that has the advantage of responding fast to changes in blood CO2 levels, but in preterm infants it is not well accepted [1,2]. This monitoring is important because it can prevent complications of hypocarbia and hypercarbia, as much as it can provide critical information about cardiac and pulmonary function [2,3]. The American Society of Anesthesiologists considers the EtCO2 a basic parameter that should be monitored during invasive mechanical ventilation (IMV) [4].
Capnometry allows a non-invasive estimate of the CO2 concentration or partial pressure in the arterial blood (PaCO2 ) [5]. Some studies showed a good correlation of EtCO2 with PaCO2 in preterm infants [1,6-8], but poorly correlated with preterm infants with Respiratory Distress Syndrome (RDS) [1,7,8]. the pulmonary disease a non-invasive technic is necessary to monitor these preterm infants in IMV continuously during the weaning process and to prevent repeated arterial blood sampling [6,9].
The weaning process of IMV is complex and needs to be carried out carefully. Before the endotracheal tube is removed, the parameters of the ventilator is gradually reduced until spontaneous respiration starts [10-12]. Usually the decision to remove IMV in preterm infants is based on clinical experience of the medical team, and there is not a protocol that could guide clinicians during this weaning period [12-14].
Arterial blood gases may be useful to predict the success of extubation but requires blood samples daily [15]. Capnometry shows a good correlation with PaCO2 and can be use full for following the weaning process in stable preterm infants [12]. This study aimed to identify the chance of success of extubation by analyzing EtCO2 levels and if this can be a predictor of the success of extubation in preterm infants.
This observational study was conducted in preterm infants admitted to the Neonatal Intensive Care Unit (NICU) at the University Hospital from August 2014 to November 2016 with gestational age (between 24 and 36 weeks + 6 days). The study was approved by the Ethics Committee of Federal University of Parana, Curitiba, Brazil. All parents signed an informed consent form to participate in the study.
All infants were on IMV, Puritan Bennett™ 840®, Carlsbad, California, and they were monitored daily, starting on the first day of IMV until the removal of the endotracheal tube. Preterm infants were excluded when they were transferred to other hospitals, airway congenital malformation, central nervous system malformation, handling restrictions, accidental extubation or early death, that it was considered within the first 12 to 24 hours of life.
The EtCO2 in exhaled air was measured by a mainstream portable capnometer (EMMA Emergency Capnometer, Phasein AB, Danderyd, Sweden) placed between the endotracheal tube and the circuit of mechanical ventilator. Values of peak CO2 concentration were displayed breath-to-breath. Time for the signal to change from a specified low value to a specified high value was ≤ 60 ms. The mean of three EtCO2 measurements in pre-extubation day was used in the analysis. For the correlation of partial pressure of arterial carbon dioxide (PaCO2) and EtCO2 the preterm infants were monitored daily, starting on the first day of mechanical ventilation until the removal of the endotracheal tube. Bias was adjusted by grouping the preterm infants by gestational age and pulmonary disease.
Heparinized arterial blood samples from radial artery were analyzed with the equipment GEM Premier 3000® (Instrumentation Laboratory, Lexington, MA), which was calibrated daily. Immediately before blood sampling, the EtCO2 value shown on the display of the portable capnometer was recorded simultaneously to the PaCO2. The interval between the measurements by capnometry and arterial blood gas did not exceed 15 minutes.
Criteria for extubation followed those recommended in the routine practice manual of the NICU/HC-UFPR of 2014, except those with accidental extubation and when the clinical team decided to maintain the extubation. The criteria for extubation are: having a regular spontaneous breathing and cough reflex; FiO2 ≤ 40% to maintain saturation ≥ 90%; PIP <15-18 cm H2O and respiratory rate of 15-20/min; pH above 7.25 and PaCO2 below 50 mmHg [16].
In total, 507 preterm infants were born at this period, 177 of them were in IMV, 72 infants were included and 51 selected by nonprobabilistic form. One infant was big for gestational age, 6 died early and 1 had pulmonary hypertension, they were all excluded. The sample comprised 43 preterm infants that were followed until the extubation. Figure 1 presents a flow chart of the study sample.
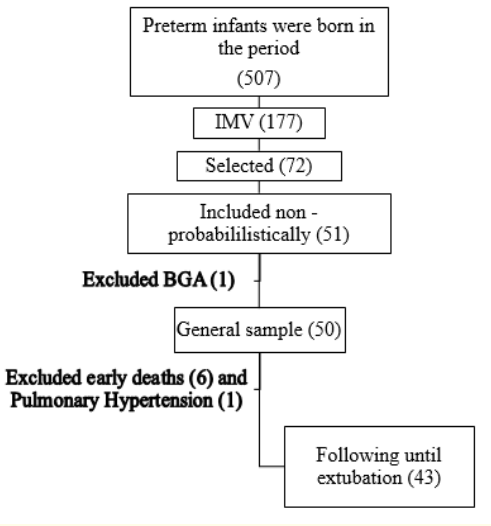
Figure 1: Flow chart of the study sample.
Descriptive data were analyzed with Statistica®, version 10. Receiver Operating Characteristic (ROC) and Univariate Logistic Regression curves were used to evaluate the performance of the capnometry in predicting success or failure in endotracheal extubation. The Mann-Whitney test compared independent samples of the groups. Pearson’s correlation was used to analyze concordance between EtCO2 and PaCO2. The Shapiro-Wilk test was used to demonstrate normality in the groups. Data are shown as mean (± standard deviation) or median (range). A p value < 0.05 was considered significant.
The study population encompassed 43 preterm infants, 24 (55.8%) boys. The mean gestational age of the entire cohort was 28.1 + 3.1 weeks, and the median birth weight was 880 g (485 – 2190 g). Participants were further divided in two gropus according to success or failure of treatment. (Table 1). The ROC curve shows that EtCO2, has a high sensitivity and specificity in predicting extubation failure (Figure 2). The cutoff point 42 mmHg had 100% sensitivity and 78.3% specificity, with a safe probability of success of extubation. The points above 50 mmHg have a sensitivity of 60% and a specificity of 82.6%, reducing the chances of success. Infants who failed extubation had higher CO2 values.
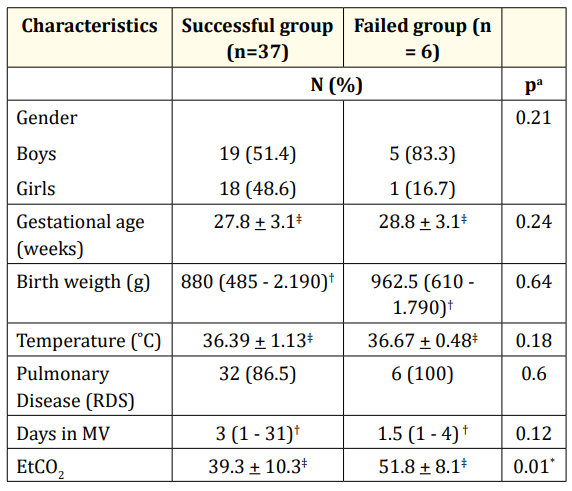
Table 1: Demographic characteristics and EtCO2
measurements (n = 43).
IQR: interquartile range, sd: standard deviation, RDS: respiratory
distress syndrome, MV: mechanical ventilation.
*p < 0.05
a = Mann-Whitney Test
† =Median
‡ = Mean ± sd
EtCO2 and PaCO2 were analysed in different gestational age and with presence or absence of pulmonary disease. Pearson’s correlation showed significant correlation in all groups, although higher in preterm infants without pulmonary disease and gestational age greater than 32 weeks (Table 2).
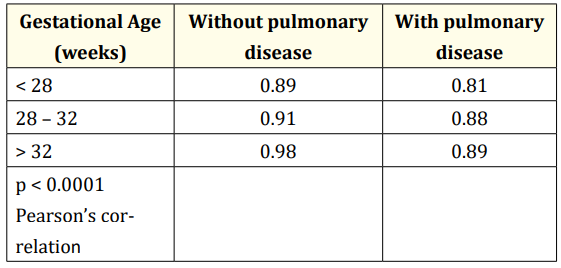
Table 2: Correlation between EtCO2 and PaCO2 in different gestational age and with presence or absence of pulmonary disease.
The Univariate Logistic Regression curve also reveal capnometry as a safe instrument to predict success of extubation. EtCO2 above 42 mmHg may decrease the chances of successful extubation (Figure 3).
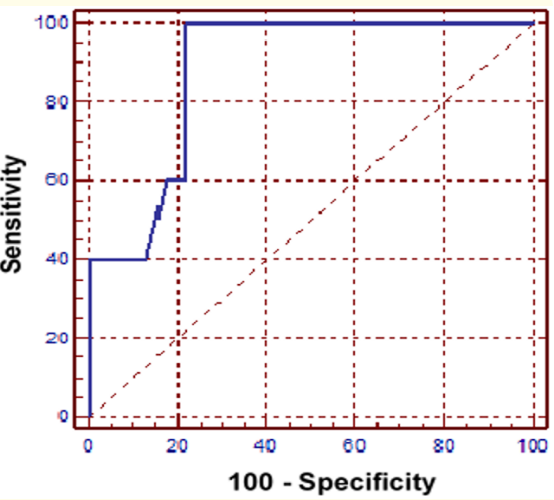
Figure 2: ROC curve (receiver operating characteristic) for analysis of capnometry in predict success or failure in the extubation of mechanical ventilation. Point 42 mmHg had 100% sensitivity and 78.3% specificity.
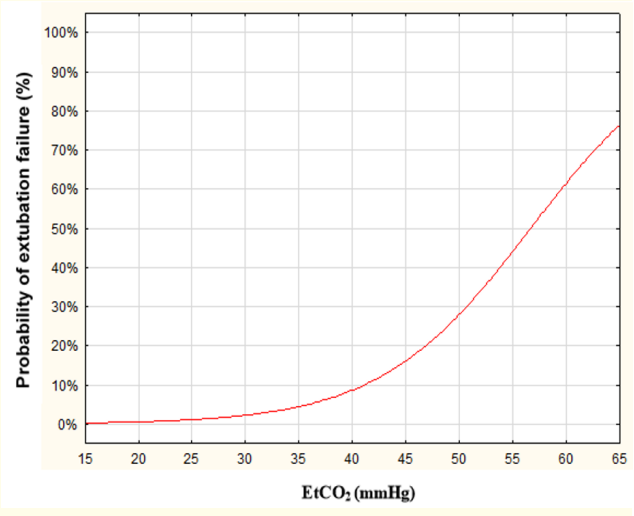
Figure 3: Univariate Logistic Regression of capnometry shows that the EtCO2 above 42 mmHg may decrease the chances of successful extubation.
The decision of extubation is based on clinical conditions, blood gas variables, oxygen support and the level of ventilator support needed, but there is no parameter that can show the extubation success [15,17]. Blood gas monitoring is necessary until the extubation moment and for many times is necessary a sample of blood. The procedure is invasive and thereby increases the risk of infection, and may cause adverse events such as iatrogenic anemia, besides it be painful [4].
EtCO2 is an alternate noninvasive method to monitor CO2 values, although this measurement in infants is not well accepted, particularly in preterm, it was showing a good concordance with PaCO2 [1,9,18]. In our study, concordant values were observed in all groups, but It was better in preterm greater than 32 weeks and without pulmonary disease, that this result agree with other authors. Wu., et al. in 2003 [1], showed a good correlation in premature infants without respiratory distress syndrome (RDS). Contrarywise Watkins and Weindling in 1987 [7], found a poor correlation (r = 0.387, p < 0.01, n = 62), between both parameters in sick preterm neonates attributed to increased physiologic dead space, different ventilation-perfusion and the severity of pulmonary disease. Trevisanuto., et al. in 2012 showed a good correlation (r = 0,69, p < 0,0001, n = 143) in extremely low birth weight infants and this concordance can be decrease with de level of the disease [8].
The capnometry presented satisfactory results and It can be used daily as an additional noninvasive resource for monitoring weaning of the mechanical ventilator in preterm infants. Analysis of the ROC curve showed that the capnometry had a high sensitivity and specificity in predicting extubation success in the point of 42 mmHg. The Univariate Logistic Regression curve agreed to affirm that EtCO2 of 42 mmHg presents a high probability of success and when the EtCO2 increases, the chance of success decreases, which at 51 mmHg, the specificity is only 40%. In a study performed with children after cardiothoracic surgery, there was a greater tendency to extubation failure with higher CO2 level, but It did not present statistically significant differences between the success and failure between the groups [19]. Thus, the present study showed the possibility of monitoring CO2 levels with less invasive way, because preterm infants need more attention due to the high frequency of blood sampling [20]. There are the need for non-invasive techniques to verify the occurrence of hypercapnia or hypocarpy, minimizing the blood samples and thus reduce the risks of anemia and also avoiding discomfort and pain in these preterm infants who are very fragile [21].
Capnometry is a noninvasive technique and is thus safe in the smallest premature infants. The results of our study suggest that EtCO2 is a valid adjunctive parameter when titrating ventilator support and may be useful for real-time analyses of abnormal PaCO2 levels both premature infants with and without pulmonary disease. The preliminary data suggest that EtCO2 is a parameter in predict success extubation in premature infants. In addition, reduce blood loss and pain in these premature infants.
Approved by the Ethics Committee of Federal University of Parana, Curitiba, Brazil, with the CAAE number 18296113.0.0000.0096.
Funding: Adriane Muller Nakato had a scholarship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
There are no conflicts of interest by authors.
We thank the team of the Neonatal Intensive Care Unit, Hospital de Clínicas and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes).
Copyright: © 2019 Adriane Muller Nakato., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.