Nam DH*, Tuan TA, Dien TM, Dung VC, Son DT , Khanh NN and Dat NP
Vietnam National Children’s Hospital, Hanoi, Vietnam
*Corresponding Author: Nam DH, Vietnam National Children’s Hospital, Hanoi, Vietnam.
Received: September 18, 2018; Published: December 21, 2018
Citation: Nam DH., et al. “Aplication of the Method of Continuous Venovenous Hemofiltration in Treatment of Acute Crisis with Organic Acidurias”. Acta Scientific Paediatrics 2.1 (2019):08-11.
Background: Organic acidurias are treatable diseases if the patients have early diagnosis and management. The diseases are usually diagnosed when patients have acute crisis and need acute management. Continuous venovenous hemofiltration (CVVH) is one of emergency methods to remove NH3 and toxic metabolites.
Objective: Evaluate results of CVVH method in management of acute crisis with organic acidurias.
Materials and Methods: Descriptive prospective study on six patients with organic acidurias having acute crisis were received CVVH between January, 2014 and March, 2015.
Results: Six patients from 2 days to 29 months of age presented acute crisis with deep coma, severe metabolic acidosis, hyperammonaemia. After receiving CVVH, plasma ammonia levels were significantly decreased from 822 µmol/l (151-3000 µmol/L) to 171 ± 54 µmol/L within 12 hours. Serum pH were increased from 7.1 ± 0.2 to 7.32 ± 0.05 within 48h with CVVH. Average CVVH duration was 4.1 ± 4.3 days. Length of stay in the ICU was 6.4 ± 5.4 days. Results of receiving CVVH: Three patients were survived with normal development; One patient was withdrawn treatment due to deep coma; Two patients died due to MODS, one patient of this group had nosocomial infection.
Keywords: Children; CVVH; Organic Acidurias; Acute Crisis; Ammoniac
Organic acidemias (OA) are a group of inheritable genetic metabolic disorders which characterized by elevated serum carboxylic acid levels (non-amine organic acids). OA is a rare condition with the prevalence rate is 1 in every 10,000 to 1 in every 15,000 children. OA can be recognized in every age but usually occurs before 1 year old. OA acute crisis usually exacerbates due to infection, poor feeding [1,2]. During the acute crisis, clinical picture usually is acute metabolic encephalopathy due to elevated ammonia and severe acidosis. When the conservative treatment failed in acute crisis, patients usually die or have a bad outcome if can not receive continuous veno-venous hemofiltration (CVVH). CVVH is the only emergency treatment to quickly eliminate ammonia and toxic metabolites to correct metabolic pathways [3- 5]. Our study was aimed at answering the following question: How effective is CVVH in OA acute crisis treatment?
From January 2014 to March 2015, six patients who were diagnosed with OA and having treatment in Department of Metabolic, Genetic and Endocrine diseases had acute crises and received CVVH in Pediatric Intensive Care Unit, Vietnam National Children’s Hospital, Vietnam.
Study design: Descriptive, prospective.
Diagnosed and confirmed by urine organic acid analysis, AND have presentations of acute crisis AND start to receiving CVVH when:
At PICU admission, all patients initially received conservative treatment consisting of protein-free parenteral nutrition, nil per os and high caloric intake (10 mg/kg/min glucose) and receiving CVVH. We used Baxter system (PRISMA) with weight-dependent catheters and Hemosol dialysis solution (Phuong Dong supplier). Blood flow was 5 mL/kg/min and replacement rate was 60 mL/ kg/minute. Dialysate flow depended on patients status and fluid management. Heparin was used for anticoagulation and adjusted during dialysis to achieve an activated clotting time (ACT) between 140 and 160s.
Statistical analysis was performed using SPSS (version 16.0 for Windows, IBM, North Castle, NY, USA).
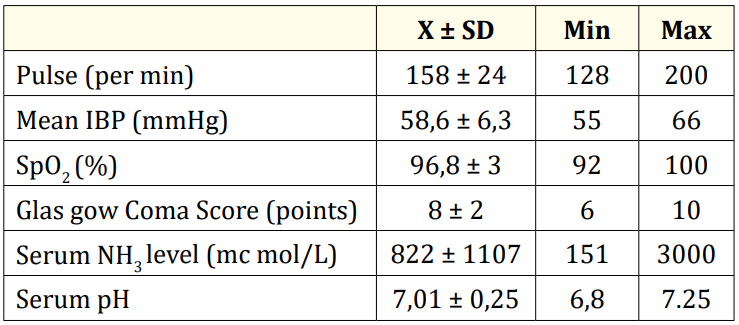
Table 1: Clinical presentation and laboratory results before CVVH.
Comment: All of the patients had deep coma, severe acidosis and high serum ammonia level before receiving CVVH.
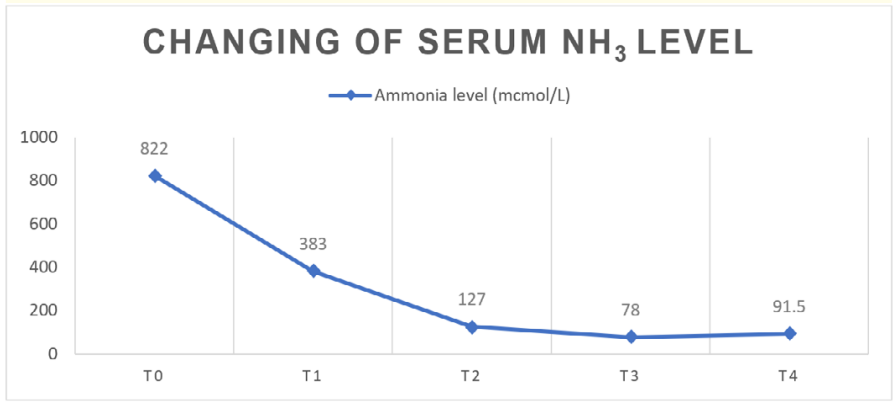
Figure 1: Changing of serum ammonia level during CVVH. Comment: After 12 h of CVVH, ammonia level was reduced to under 200 µmol/L and after 24 h of CVVH, to under 100 µmol/L.
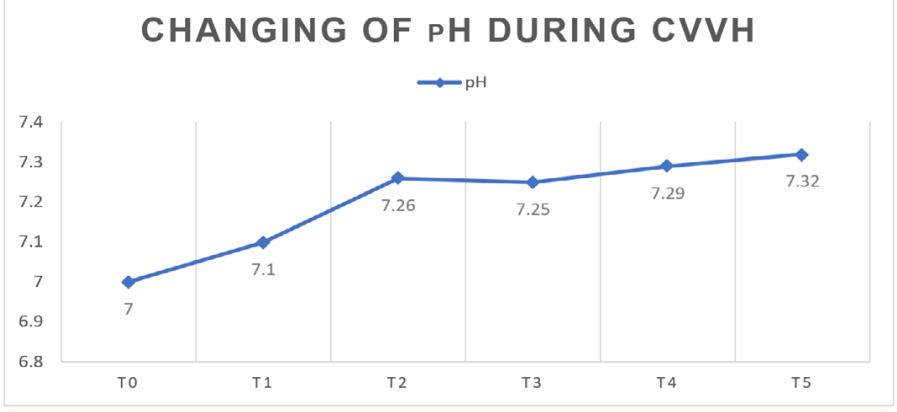
Figure 2: Changing of pH during CVVH. Comment: Serum pH level increased during CVVH. After 36 h of CVVH, pH approximatelyreached normal level.
Based on the results of the study, we found that six patients had similar morbidity prevalence in accordance with the pattern of inherited chromosomal recessive disease of OA disorder. Age of acute crisis exacerbation was between 2 days old and 29 months old. In literature, the age of acute crisis exacerbation can be any time depends on the clinical and investigations and exacerbating factors (e.g infection, changing of food) [6,7].
We had two severe patients with septicemia and propionic metabolic disorder. Four patients with OA. These patients admit to ER in severe condition (deep coma, unstable hemodynamic, hyperammonemia, severe acidosis) and already had poor prognosis. After having respiratory and cardiological support, all of them started to receive CVVH (blood flow was 5 mL/kg/min and replacement fluid was 60 mL/kg/hr, dialysate flow was adjusted up to hemodynamic). We kept ACT between 140 and 160s.
During the follow-up, we recognized that ammonia level was significantly reduced after 12 hours of CVVH: 822 to 171 +/- 54 mcmol/L after 12 hr CVVH; and 50% ammonia reduction time was 4.7 +/- 2.5 hr of CVVH. Ammonia level decreased under 200 mc mol/L within 20 h. The effectiveness of ammonia reduction in our study was similar to the result of Anja., et al. The acidosis was corrected after 24 h of CVVH. This result shows that CVVH is effective to correct metabolic pathways in this group [8].
However, mean duration of CVVH in our study is longer than duration in Kevin and Anja's studies. We consider that the reason is our patients were admitted to PICU lately, most of them had MODS and the time of starting CVVH were late. About treatment outcome, three of six patients survived (50%). All patients stopped CVVH when ammonia levels were below 200 mc mol/L, good urinary output, stable clinical presentations. These patients were followed up in PICU within 1 - 2 days, after that were transferred to Department of Endocrine, Genetic and Metabolic Diseases for continuous treatment. Three patients died (50%). Mortality causes were deep coma (1 patient), septic shock with MODS (2 patients). The patient died due to deep coma admitted to hospital after severe prolonged brain injury (GCS 6 points at admission). This patient’s ammonia level was reduced after CVVH but mental status was not better. To avoid long-term neurological complications, we should recognize symptoms of acute crises earlier and start CVVH as soon as conservative treatments failed. Two patients died of septic shock despite metabolic disorder and ammonia level had improved. Thus, infection management, especially hospitalacquired infection, is very important to have better outcomes. Our results are similar to Kevin study's result which showed that there were only two of five patients with metabolic disorders survived in their case series [9].
Ad serve events and complications of CVVH: none of our patients had electrolytes disorders. One patient had filter obstruction due to catheter position. We solved this problem after resecuring catheters. One patient had septicemia due to multi-resistant antibiotic E. coli, this patient already had MODS before CVVH and received CVVH within 36 h but still have deep coma, thus, was withdrawn treatment. In Falk’s study, in total four patients had CVVH, there was one patient died of HAI. Consequently, HAI control is a key point of intensive care [10].
CVVH was an effective treatment in order to eliminate ammonia and correct metabolic acidosis in children with OA acute crisis.
Copyright: © 2019 Nam DH., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.