Vinay Sharma MD *
University of Minnesota, Department of Pediatrics, USA
*Corresponding Author: Vinay Sharma MD, University of Minnesota, Department of Pediatrics, USA
Received: November 21, 2018; Published: November 26, 2018
Citation: Vinay Sharma MD. “Delayed Cord Clamping: Ancient Phenomena but New Perspective”. Acta Scientific Paediatrics 1.5 (2018):22-23.
In 1801, Erasmus Darwin suggested that ‘Another thing very injurious to the child, is the tying and cutting of the navel string too soon; which should always be left till the child has not only repeatedly breathed but till all pulsation in the cord ceases. As otherwise, the child is much weaker than it ought to be’. That perception changed in 1900’s with the invent of modern day medicine and the practice of immediate cord clamping(ICC) cemented its place in normal maternal and newborn care, though it was perceived that early cutting of umbilical cord would offer benefit to the mother and would pose no “inconvenience” to the newborn. Umbilical cord clamping is not just a symbolic separation of infant from mother, but it can have a significant impact on infant’s wellbeing after the birth. There is substantial evidence supporting the natural approach of delayed cord clamping (DCC) at birth. This practice is now endorsed by the major governing bodies affiliated with maternal-newborn care (Table-1).
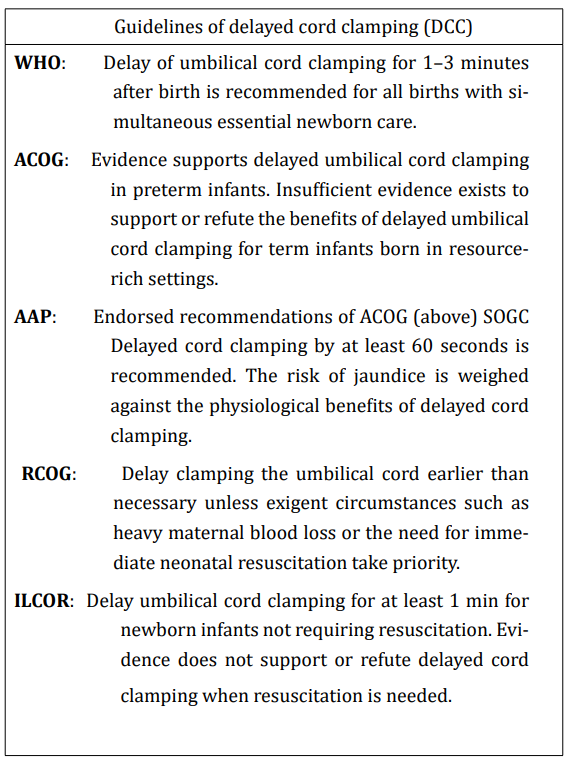
Table 1: Guidelines of delayed cord clamping (DCC).
Abbreviations: WHO: World Health Organization; ACOG: American College of Obstetricians and Gynecologists; AAP: American
Academy of Pediatrics; SOGC: Society of Obstetricians and Gynaecologists of Canada; RCOG: Royal College of Obstetricians and Gynaecologists; ILCOR: International Liaison Committee on Resuscitation.
Each of the governing bodies has their interpretation of the available evidence, which is evident in their recommendations (Table-1). ACOG, SOGC and AAP limit DCC in infants who are premature while RCOG, ILCOR and WHO recommend delayed clamping of the cord in all newborns. Also, recommendations on how long to delay the clamping of the umbilical cord differs; recommendations vary from 30 seconds to 3 minutes. This incongruity in recommendations may lead to confusion amongst the providers, which can create an impedance in the implementation and widespread success of these practices. It makes it imperative to learn the role of DCC in transitional circulation in order to make an educated decision for their patients.
In fetuses, the placenta does the gas exchange, and lungs receive only 10% of the cardiac output. The transition from fetal to newborn life represents one of the most significant physiological challenges that any human will encounter. As lung aeration can only occur after birth and is a pre-requisite for newborn survival, it is an ideal trigger for initiating the physiological changes that underpin the transition to newborn life. That transition is initiated by first breath which leads to a decrease in pulmonary resistance and increasing its pulmonary blood flow. If infant receives immediate cord clamping (ICC), there is a sudden increase in systemic resistance by occlusion of umbilical arteries and drop in effective blood volume (preload) as an effect of blocking umbilical vein, which can cause significant changes in vital parameters like heart rate and blood pressures during this transitional. These associated changes with ICC would become even more apparent in infants who are born premature or asphyxiated; little hemodynamic fluctuation can worsen insults to the vital organs which would impact their short and long-term outcome. In newborns with DCC; uninterrupted supply of oxygenated blood through umbilical vein to the left atrium through foramen ovale stabilizes the cardiac output to provide stable oxygen and blood supply to the vital organs during this transition. In the infant with asphyxia, this oxygenated blood can be vital for the time effective ventilations are established. It has also been proven that for preterm infants by minimizing these transient fluctuations in vital parameters, the incidence of necrotizing enterocolitis and intraventricular hemorrhage can be decreased. Also, this oxygenated blood when pushed to lungs can decrease pulmonary pressures and could further help with improving ventilation. With a better understanding of the transitional physiology, this is apparent that performing DCC till the time ventilation is established, which could spontaneous cry in healthy newborn to endotracheal intubation in compromised newborns can benefit all newborns.
In term infants about one-third of blood flows through the placenta and two-thirds flows through the fetus at any point. Amount of blood flowing through the placenta in inversely proportional to the gestational age. In healthy term infants, ICC results in around 30% of feto-placental blood volume remaining in placenta, whereas DCC reduces the residual volume by 10% with 60 seconds and by 17% with the delay in cord clamping by 3-5 minutes. There are also other factors like uterine contractions, and spontaneous breathing in neonates that can influence the transfer of placental blood to the newborn after the delivery, while the placement of baby after delivery have little influence on the transfusion of placental blood.
With practice of DCC, there is a small increase in the incidence of jaundice that requires phototherapy in term infants undergoing delayed umbilical cord clamping. There is no evidence that it increases the chances of bilirubin encephalopathy.
Copyright: © 2018 Vinay Sharma MD. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.