Diksha Gupta1, Linda Chen2, Seleshi Demissie2 and Pushpom James2*
1
Touro College of Osteopathic Medicine, Harlem, New York
2
Staten Island University Health, Staten Island, New York
*Corresponding Author: Pushpom James, Staten Island University Health, Staten Island, New York.
Received: September 19, 2018; Published: November 02, 2018
Citation: Sangita D Kamath., et al. “A Case Report on Choroidal Metastases from Adenocarcinoma of Lung – Tip of the Iceberg!”. Acta Scientific Paediatrics 1.5 (2018):00-00.
Objectives: This quality improvement project aims to increase pediatric resident’s compliance with asthma classification of hospitalized patients and improve rates of spacer prescription with MDIs. These are initial steps towards preventing an unnecessary asthma readmission.
Methods: Pediatric patients admitted to the floor or the PICU at our 714-bed tertiary care hospital with asthma exacerbations were recruited. The interventions included reviewing asthma classification guidelines and education on spacer use with MDIs. Chart reviews on resident’s compliance with classifying asthma and prescribing spacers before intervention were labeled as “control group” (CG), and the data collected after the intervention, was the “intervention group” (IG).
Results: Our study is based on n = 97 patient encounters (CG n = 40, IG n = 57). Demographics of the two groups were similar in gender and mean age; however, there were statistically significant higher PICU admissions in the intervention group, 31.6% compared to 12.5% in the control group (p = 0.032). Asthma classification rate was 15.0% (CG) and 49.1% (IG), which is a statistically significant improvement (p < 0.001). The rate of spacer prescription was 7.5% (CG) and 21.1% (IG), which is not statistically significant (p = 0.090).
Conclusion: This study was successful in improving asthma classification rates. The rate of spacer prescription did not significantly improve, likely due to high rate of nebulized medication prescriptions. Next step for this quality improvement project is to continue to stress the need for asthma classification and improve spacer prescription, by providing literature on the efficacy of MDI with spacer use in asthma management.
Keywords: Asthma; Readmissions; Spacer
PICU: Pediatric Intensive Care Unit; CG: Control Group; IG: Intervention Group; MDI: Metered Dose Inhaler; CAC-3: Children’s Asthma Quality Measures; IRB: Institutional Review Board; PDF: Adobe Portable Document Format; ICD: International Classification of Diseases; SAS: Statistical Analysis System; NC: North Carolina.
Asthma is the most common chronic disease of childhood with uncontrolled asthma leading to deterioration of lung function, development of irreversible airways obstruction, and poor quality of life.
Implementation of the Joint Commission Children’s Asthma Quality Care Measures (CAC-3) [1]. has been shown to be effective in reducing asthma readmission rates. As our hospital’s compliance with these quality measures was poor, we decided to implement full compliance with the quality measures in a stepwise manner.
Assessing asthma severity and control and educating patients on using an MDI with spacer are both vital to achieving control, post discharge.
When a child is hospitalized with an asthma exacerbation, the focus is often on stabilizing the child and the use of clinical pathways to decrease length of stay. There is often minimal emphasis on maintaining asthma control and preventing readmission of these patients.
A stepwise approach to asthma management incorporates four components according to the National Heart, Lung, and Blood Institute: [2].
Assessment (asthma severity and control) is one of the important first steps in asthma control and one that should be an integral part of the discharge process.
Education - Poor understanding of disease severity and inadequate management of the disease can lead to poor compliance with medications.
Control of environmental factors and comorbid conditions
Medication - Mode of medication delivery is a factor that influences the success of treatment adherence. Spacers can improve and simplify inhaler technique. Long term compliance with nebulized inhaled corticosteroids tends to be poor, due to the time involved with this method of delivery [3].
The rate of post emergency room follow-up after a hospitalization for an asthma exacerbation to a pediatrician was 23.6% in 7 days and 40.3% within 30 days [4]. However, the follow-up with pediatricians within 30 days was not associated with decreased emergency room visits for asthma over the year [4]. It is therefore imperative to provide more education and services during a hospitalization, to prevent unnecessary readmissions and repeat emergency room visits. If MDI/spacer education is routinely provided at the time of discharge, this may improve compliance with controller therapy. Studies have shown that the most common mistakes with MDI use include not exhaling before starting, not shaking the MDI and inhaling for a very short time [5] with statistically significant improvement at 1 hour with improved technique.
According to researchers Osmond., et al, the largest barriers to the implementation of MDI with spacer prescriptions include concerns regarding parental expectations for use of nebulizers, hospital staff beliefs regarding the effectiveness of MDI/spacer use, changes in nursing work load and lack of a physician champion for change [6]. Although there are barriers to MDI/spacer use, there are advantages that need to be highlighted and taken into consideration when choosing the right method to use for asthma control. Powell., et al, state that less time is required to administer the MDI/spacer treatment, and this results in better compliance, this is more cost effective, a portable device, and easier to use than nebulized medication [7]. Spacer use with MDI provides space and
time for the propellant droplets to evaporate and decelerate, reducing the particle size. This in turn decreases the oropharyngeal deposition and potential systemic absorption through the gastrointestinal tract [8]. Furthermore, Alhaider., et al, mention advantages to using MDI/spacer are the elimination for the need for nebulizer compressors with a power supply and disposable nebulizer kits [9].
Since many hospitalizations and emergency room visits for bronchial asthma exacerbations are preventable, emphasis on verbal instruction in addition to physical demonstration of correct inhaler technique [10] needs to be made during hospitalizations for bronchial asthma exacerbations. The rate of readmission for an asthma exacerbation is 30% [10]. When asthma is classified, appropriate anti-inflammatory medications could be prescribed, resulting in a decrease in the readmission rate.
We decided to target asthma classification by residents to improve the prescription of controller medication at the time of discharge, as the first step to a more comprehensive discharge plan focused on preventing unnecessary asthma readmissions. Knowing that ease of using a MDI /spacer for the administration of controller medications, was likely to improve compliance, compared to using nebulized controller medication, we decided to also try to promote spacer prescription and demonstration.
A preliminary chart review of two month’s data showed that resident’s rate of classifying asthma was approximately 1 in 20 cases, and documented spacer education and prescription was rare.
The main interventions were awareness, education, and reinforcement.
Awareness was facilitated by announcements during resident conferences and by email notifications.
Education was provided by reviewing asthma classification guidelines and discussing the importance of prescribing a spacer with mouth piece or mask to use with MDIs. Spacer education demonstrations and instructions to facilitate residents electronically prescribing spacers were provided. Educational material (PDFs, electronic videos) was also emailed to residents.
Reinforcement was provided by Asthma Classification Reference Cards (to attach to identification badges and at computer workstations) and frequent follow up.
The sample size for this study was a sample size of convenience and was not based on any formal statistical power calculations. Data from 97 patients (40 pre-intervention and 57 post-intervention patients) were included in the statistical analyses.
Pediatric patients admitted to the floor or the PICU for acute asthma exacerbations at our 714 bed New York City based teaching hospital, where there are 1800 pediatric inpatient admissions a year.
ICD-9 and ICD-10 codes were used to identify these patients.
A chart review was performed examining resident’s compliance with classifying asthma and prescribing spacers 6 months before and after intervention.
Descriptive statistics for demographic and baseline disease characteristics were presented. Categorical data were summarized using frequency counts and percentages and continuous variables were summarized by descriptive statistics, including mean and standard deviation. Categorical variables were compared using the Chi-Square analysis while the two-sample t-test was used to compare continuous control and intervention groups. All statistical tests were two-sided and conducted at the 0.05 level of significance. Data analyses were conducted using the SAS* System Verizon 9.3 (SAS Institute Inc, Cary, NC.).
Demographics and clinical characteristics between the two groups were similar. The mean age of patients in the control and interventional groups were 7.4 and 6.7 years respectively. The percent of male patients was 50.0% in the control group and 57.9% in the intervention group (table 1). The intervention group was noted to have significantly higher PICU admissions, 31.6% compared to 12.5% in the control group (P = 0.032).
The data showing improvement in asthma classification rates was statistically significant, but the rate of spacer prescription did not significantly improve, likely due to a high rate of nebulizer prescriptions (rate of prescribing nebulizers in CG 42.5% and IG 45.6%).
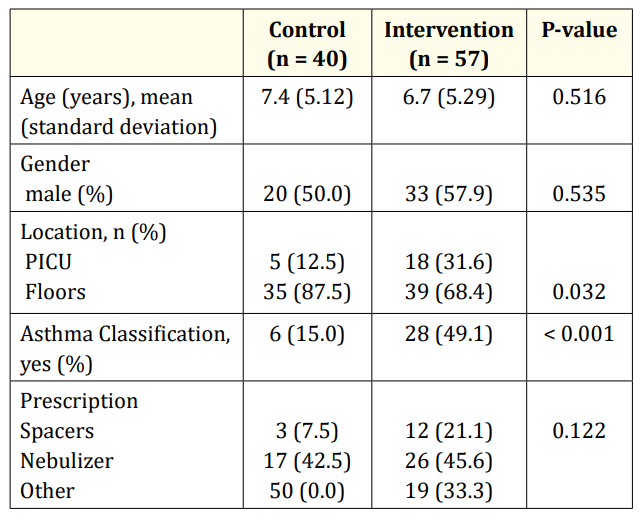
Table 1: Demographic and clinical Characteristics.
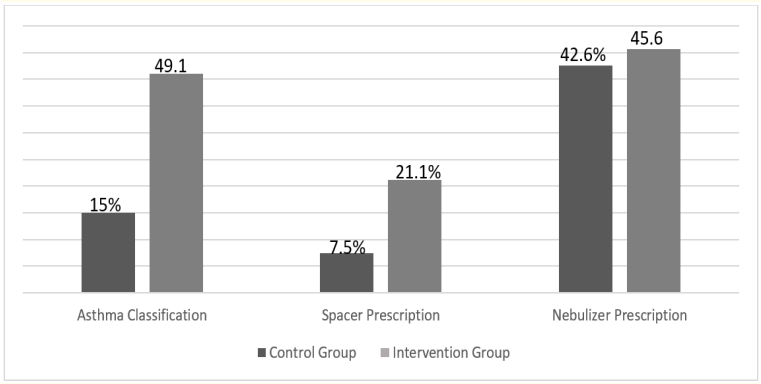
Figure 1: The rate of asthma classification between the control and intervention group in patients prescribed spacer versus nebulizer treatment.
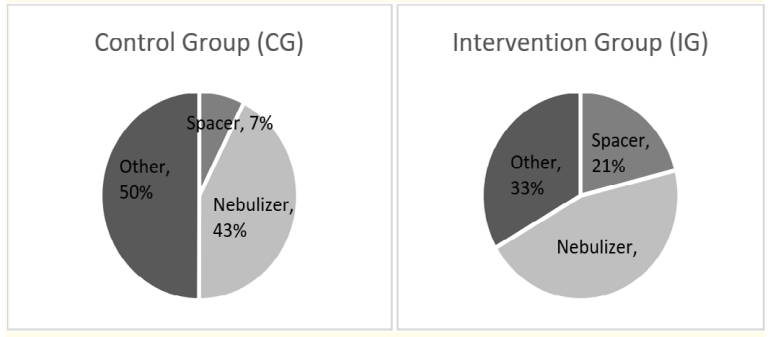
Figure 2: Distribution of patients discharged with spacers, nebulizers or other treatments between the control and intervention group.
Resident classification of asthma severity was statistically improved. The prescription of MDI/spacers increased, but was not statistically significant, likely due to a high rate of nebulizer prescriptions (rate of prescribing nebulizers in CG 42.5% and IG 45.6%). Literature showing the advantages of MDI/spacers compared to nebulized therapy was not part of the educational materials provided to residents [11], which may have contributed to the persistently high nebulizer prescription rate.
CAC3 requires documentation of quick reliever and controller prescription, environmental or other trigger control, a follow up appointment and an asthma action plan [4].
The increased compliance with Children’s Asthma Care 3 showed a sustained decrease in 6-month asthma readmission rate from 17% to 12%, validating CAC-3 as a quality measure [4].
We decided to try to decrease asthma readmission rate by initially focusing on the asthma severity classification by residents and promotion of discharge with a spacer and mask/mouthpiece.
Transitioning patients to MDI with spacer medication prior to discharge may improve control.
Next steps are to go beyond Children’s Asthma Care 3 by promoting a comprehensive discharge plan to include not only asthma classification, but prescription of controller and rescue therapy using a MDI/spacer, trigger control information and providing follow up with primary physicians. Referral to pulmonologists and social service will be made if indicated.
This study was successful in improving asthma classification rates, but the rate of spacer prescription did not significantly improve, likely due to high rate of nebulizer prescriptions.
Considerations for improvement: Providing literature on the efficacy of MDI with spacer use in asthma management to residents including the fact that compliance with long term nebulized corticosteroids is poor, because of the time involved maybe helpful in increasing spacer prescriptions.
Encouraging residents to classify asthma severity and encourage MDI with spacer prescription are important first steps towards preventing a child with asthma from being readmitted with an asthma exacerbation.
No funding was secured for this study.
Authors have no financial disclosures relevant to this study.
There are no conflicts of interest to disclose.
Copyright: © 2018 Pushpom James., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.