Fadi M Jan1, Hesham M Aldhalaan2, Nadia H Dandachi1, Doaa H AlAbbas1, Ahmed M Elmardenly3, Maher A Khalifa3 and Mohammed M Jan1*
1 Department of Pediatrics, Faculty of Medicine, King Abdulaziz University, Jeddah
2 Pediatric Neuroscience department, King Faisal Specialist Hospital and Research Center, Riyadh
3
Pediatric Neurology Unit, Pediatrics Department, Dr. Erfan and Bagedo Hospital, Jeddah, Kingdom of Saudi Arabia
*Corresponding Author: Mohammed M Jan, Department of Pediatrics, Faculty of Medicine, King Abdulaziz University, Jeddah.
Received: September 25, 2018; Published: October 31, 2018
Citation: Mohammed M Jan., et al. “Chronic Functional Constipation causing Recurrent “Anal Spasms”: An Epilepsy Mimicker”. Acta Scientific Paediatrics 1.4 (2018): 45-48.
The diagnosis of epilepsy depends heavily on detailed history and timely observation. Several non-epileptic causes of paroxysmal events can be confused with recurrent seizures [epilepsy mimickers]. These include gastro-esophageal reflux, breath holding spells, self-gratification, movement disorders, and others. In this paper we present four children, aged 2-5 years, who were initially misdiagnosed as epilepsy and referred because of lack of control on multiple antiepileptic drugs. They would adopt positions and have facial features that mimic motor seizures. Clinical re-evaluation revealed that these events were the result of frequent anal spasms that occurred as the child was trying to withhold defecation. Severe chronic functional constipation was documented in all of them resulting in painful defecation and soiling. Anal fissure contributed to the painful anal spasms in most cases. All abnormal movements resolved by appropriate stool softeners. We conclude that recurrent anal spasms due to stool withholding should be considered as one of the epilepsy mimickers.
Keywords: Chronic; Functional; Constipation; Anal; Spasms; Epilepsy
The diagnosis of epilepsy depends heavily on detailed history and timely observation [1]. Neurological examination and investigations, such as electroencephalography [EEG] or neuroimaging, may all be normal. Therefore, the diagnosis is predominantly a clinical one [2]. Several non-epileptic causes of paroxysmal events can be confused with recurrent seizures [epilepsy mimickers], including gastro-esophageal reflux, breath holding spells, selfgratification, movement disorders, and others [3]. The possibility of misdiagnosis is a very real one with significant undesirable consequences, such as unnecessary investigations, medications, or hospitalization. Identifying these non-epileptic paroxysmal events would therefore prevent such mismanagement and alleviates associated parental distress.
On the other hand, chronic constipation is one of the most common causes of patient visits to pediatric clinics [4]. Up to 10% of visits to health centers and up to 25% of referrals to pediatric gastroenterologist are related to constipation [5,6]. If no fundamental organic cause is found, the constipation is considered functional [7]. Untreated constipation may cause fecal impaction, fecal soiling, and predisposes to the development of anal fissure [8,9]. In this paper we present four children with severe chronic functional constipation who were initially misdiagnosed as epilepsy. The episodes were related to recurrent anal spasms with stool withholding causing motor changes that were interpreted as seizures. We highlight this association that is rarely reported and propose that it should be included as one of the epilepsy mimickers.
A 4-year-old boy was referred for a second opinion with a 1-year history of recurrent seizures that failed to respond to multiple antiepileptic drugs [AEDs]. He was born following a full-term unremarkable pregnancy with induced vaginal delivery. Perinatal history was complicated by a cardiac murmur that was due to a patent ductus arteriosus. It was surgically ligated, and the child seemed to develop and function normally apart from on and off constipation. Social and family histories were unremarkable apart from positive consanguinity. At around the age of 3 years the child started to develop recurrent episodes of abnormal posture, intermittent muscle stiffness, and abnormal movements. No clear loss of consciousness, color change, or post-ictal change was noted. The episodes never occurred during sleep. He was diagnosed with epilepsy following obtaining an electroencephalogram [EEG] and a brain magnetic resonance imaging [MRI]. The parents were told that the EEG was abnormal, and the child was placed on Valproic acid with no benefit. He was evaluated by several other physicians and then switched to Carbamazepine. The episodes recurred with varying frequency with no apparent generalizations. Because of lack of response, the parents were advised to see a child psychiatrist who found no psychosocial risk factors. Levetiracetam and topiramate were tried with no response. The child was then referred to the last author [MMJ] at the department of pediatrics of King Abdulaziz University hospital in Jeddah, Saudi Arabia for further assessment. At that time, he would have up to 6 of these episodes on daily bases. Detailed neuro-developmental assessment was within normal limits for age. Review of video recordings, which were prepared by the frustrated parents, revealed that the child would typically adopt a standing posture with stiffening and crossing of legs associated with irritability and facial grimace. He seems to be in pain for a minute or two and then relaxes abruptly. Stool withholding behavior was suspected and further gastrointestinal history was obtained. Upon detailed questioning, the parents described a long history of chronic constipation since the age of 1 year. No long-lasting solution was achieved, and the child continued to have repeated cramping abdominal pain and soiling to the extent of requiring being in diapers for most of the daytime. The child will always pass some stool following the recurrent stool withholding episodes.
The child resisted ano-rectal examination. Review of previous EEGs and MRI revealed normal results. The child was therefore referred to pediatric gastroenterology and the AEDs were weaned slowly. Severe chronic functional constipation was diagnosed with fecal impaction, but no anal fissure was found. High fiber diet was started with stool softeners. The child was followed with abrupt and complete resolution of the presenting spells. He was seen 3 months later in a great condition and off all AEDs.
In addition to the case illustrated above, we have encountered 3 similar cases during our practice. They presented in a very similar pattern and all were associated with severe chronic functional constipation as summarized in the table. Anal fissure contributed to the painful spasms and painful defecation in all of them. Abnormal motor movements were secondary to the withholding of hard stools, characterized by stiffening and crossing of legs associated with irritability and facial grimace. No cyanosis, loss of consciousness, or post-ictal phase were noted. The episodes were frequent and usually would last for few minutes, but typically less than 2 minutes and always associated with soiling. All cases were initially misdiagnosed as epilepsy and referred because of lack of control on multiple antiepileptic drugs [table]. Neurological examination and investigations were always normal. Videotape documentation was obtained in all cases. Once the diagnosis was suspected, the antiepileptic drugs were weaned slowly, and the child was referred to pediatric gastroenterology [GI]. All their symptoms resolved completely with appropriate stool softeners and dietary advice. On longer-term follow up [mean 1 year], one child had some recurrences related to poor compliance with the constipation management and another child was lost to follow up (Table).
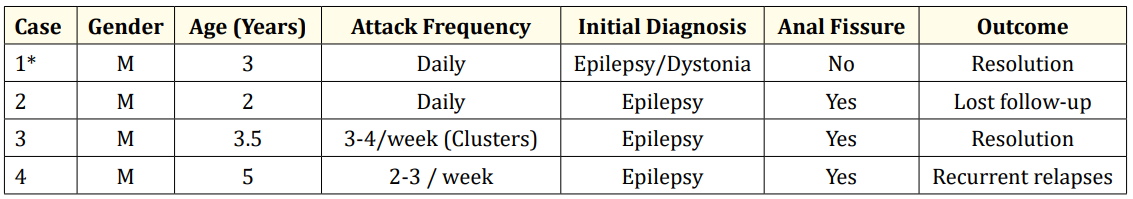
Table: Summary of the four patients with chronic functional constipation.
Chronic constipation results in painful defecation, particularly if associated with anal fissure. Memory of this experience would explain the anal spasms and associated stool withholding behavior that slowly develops to prevent exaggeration of the pain that is associated with defecation. The more the child holds on, the harder the stool will become, causing a vicious cycle of harder stool and more pain [10]. The development of anal fissure increases the pain severity and causes spasm of the internal anal sphincter leading to reduced local blood flow and delayed healing [11]. The fear of defecation is then reinforced, and the problem becomes chronic with increased amount of concentration and physical effort needed as the stool builds up resulting in the changes in posture and appearance that mimic seizures [12].
Misdiagnosing the stool withholding behavior as seizures has been rarely reported [12-14]. These reported cases were very similar to ours with tendency for the symptoms to start in infancy. Males were more often affected, similar to what is usually reported in children with chronic constipation associated with fecal overflow [15]. The associated soiling was misinterpreted as seizure associated sphincter dysfunction. Patients were subjected to many unnecessary investigations and treatments. We suspect that stool withholding mimicking seizures is more common than what is being reported in the literature or may be under recognized. Our report further highlights this association, which should be considered in the differential diagnosis of epilepsy mimickers.
The recurrent anal spasms with stool withholding and associated leg crossing posture may superficially simulate self-stimulatory behaviors and therefore may be mistaken for self-gratification phenomena [16]. This phenomenon, which is in fact more common in females rather than males, may also be mistaken for epilepsy [17]. Some authors suggested a link between chronic constipation with stool withholding and this self-stimulatory behavior, so called “anal masturbation” [18]. However, this is less likely to be self-stimulatory but rather represent a habit exaggerated by constipation and painful defecation.
We conclude that recurrent anal spasms due to stool withholding should be considered as one of the epilepsy mimickers in children with chronic functional constipation. The abnormal movements resolved completely with stool softeners and easier defecation. Accurate history, observation, and videotaping of the events would prevent such misdiagnosis and unnecessary investigations, treatments, which will contribute significantly to parental anxiety and distress.
Copyright: © 2018 Mohammed M Jan., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.