V Velev*, I Ivanov, T Tomov, M Dinkova and A Mirtschew
University Hospital for Infectious and Parasitic Diseases “Prof. Iv. Kirov”, Medical University of Sofia, Bulgaria
*Corresponding Author: V Velev, University Hospital for Infectious and Parasitic Diseases “Prof. Iv. Kirov”, Medical University of Sofia, Bulgaria.
Received: September 20, 2018; Published: October 31, 2018
Citation: V Velev., et al. “Steven- Johnson Syndrome in a Primary Varicella Infection. A Case of a 2 - Year Old Child ”. Acta Scientific Paediatrics 1.4 (2018): 31-33.
Steven - Johnson syndrome (SJS) is a severe skin reaction, following the application of some medications and it is rarely the result of some infectious agents. In this work, we describe a two-year-old boy with chicken pox, which on the second day complicates with SJS. We present the clinical course with severe skin lesions and therapeutic behavior with a favorable outcome.
SJS is one of the rare complications of varicella. Pneumonia and encephalitis is more common. All this again shows the need to use a vaccine in a very large number of children.
Keywords: Steven - Johnson Syndrome; Varicella; Skin Reaction
Steven- Johnson syndrome (SJS) is a severe skin reaction, following the application of some medications and it is rarely the result of some infectious agents. Both conditions – SJS and toxic epidermal necrolysis (TEN) include a wide range of severe skin diseases. Currently, the most widely recognized classification is based on the affected body surface. The condition is defined as SJS when the affected area takes up to 10%, and in cases of TEN – more than 30%. When the size of the damaged area is between 10 and 30%, there is an overlap between the two syndromes.
SJS begins with fever and burning eyes which is commonly misdiagnosed like trivial viral infection. After a few hours bullous lesions and ulcers in the skin and mucous membranes occur. The most common cause is some medication and very rarely infections.
A 2- year old boy with a sub febrility up to 37.5ºС, mild cough and several skin eruptions on the face, scalp and the others haircovered body areas. On the second day, lesions appear in the oral cavity, disabling the child to eat and subsequently it is hospitalized. Four hours after the hospitalization the rash intensifies, and the temperature sharply rises. The lesions in the oral cavity increase in number and size and a hemorrhagic rash starts to appear on the lips and the perioral area (Figure 1). There is a slight edema on the upper eyelids and a conjunctival redness. In about 2 hours several bullous lesions with areas of desquamation become evident on the arms and the body (Figure 2). The rash syndrome spread to the preputium and the mucosa underneath. The temperature was higher than 39ºС, with chills.
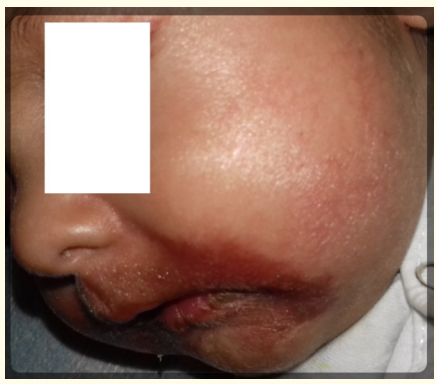
Figure 1: Hemorrhagic rash on the lips and periorally.
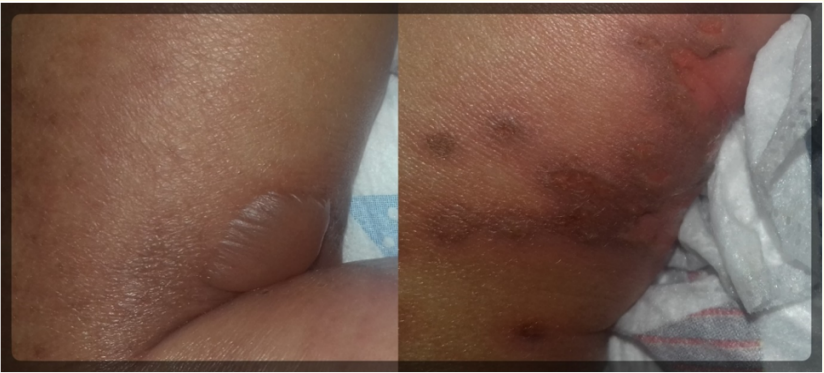
Figure 2: Bullous lesion and desquamation on the legs.
Due to the specific symptomatology with the sharp rise of the temperature, the rash syndrome with bullous lesions, the hemorrhagic perioral lesions, the conjunctival injection and the positive test for IgM against VZV (Varicella zoster virus), we accepted Steven–Johnson syndrome (SJS) in the course of Varicella as a final diagnosis. Another strong argument is the fact that up until the 6th hour of the hospitalization, the child was on no medications, including antipyretics [1,2].
According to our data, this is the youngest patient in Bulgaria with the diagnosis of SJS, which makes it evident that SJS should be suspected in any case of application of medications or infections, regardless it is significantly rare among children.
Venous infusions of glucose-saline solutions of Acyclovir 3 х 10mg\kg, Methylprednisolone 1mg\kg were started. After the three-day course of Methylprednisolone and the five times a day application of Acyclovir, the child made a full recovery.
Although SJS has a slightly milder course, it is quite rare, affecting between 1.2 and 6 people in a million annually. However, the mortality can reach up to 5%. There is an evident connection between the older age of the patients and the prevalence of SJS [1,2].
The medications, mostly related to triggering SJS, are mainly antibacterial, particularly Sulfonamides, Vankomycin, Penicillins, and others like Allopurinol and Barbiturates. Some of the most commonly reported infectious agents include EBV, CMV, Myicoplasma pneumonie [2].
Despite being very unlikely, VZV has also been noted as SJS- inducing agent [3].
This severe and complicated case of chicken pox is another proof that this infection should not be overlooked [4,5]. It is a positive fact that this is a disease against which a reliable vaccine has been made. In Bulgaria, this vaccine is not yet routinely given to children, but we hope that the health authorities will take this step soon
The authors would like to acknowledge the patient and her family for allowing this manuscript to be possible.
None declared.
Copyright: © 2018 V Velev., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.