Safaa A EL Meneza1*, Mariam A Abu-Shady1, Mohamed Aref2 and Abeer Nabil Abd Elbaseer1
1
Pediatrics Departments, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
2
Clinical Pathology Departments, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
*Corresponding Author: Safaa A EL Meneza, Pediatrics Departments, Faculty of Medicine, Al-Azhar University, Cairo, Egypt.
Received: August 06, 2018; Published: September 06, 2018
Citation: Safaa A EL Meneza., et al. “Neutrophil CD64 as Marker to Differentiate Early Sepsis from Noninfectious Respiratory Disorders in Newborn Infants”. Acta Scientific Paediatrics 1.3 (2018):10-15.
Objective: It is important to differentiate early sepsis from non-infectious respiratory disorders. The aim of this work is to identify the reliability and utility of CD64 as novel immunological rapid indicator in diagnosis of early-onset neonatal infection among full term infants.
Design: This prospective study was conducted on 80 term neonates.
Setting: NICU of Al-Azhar University Hospital.
Participants and Intervention: Sixty (60) of these neonates had been suffered from respiratory distress (RD). Complete blood count, CRP, blood gases, blood culture, and CD64 by flowcytometry were estimated.
Outcome Measures: The roles of these markers for predicting early sepsis were determined.
Results: The percentage of neutrophils expressing CD64 was highly significant increase in all respiratory distress cases with infection when compared to respiratory distress cases without infection as p < 0.001. The results of the present study also demonstrated a highly significant rise of both CD64% and its expression intensity in newborn infants with gram negative septicemia as compared to those with gram positive septicemia and Candida infection (p < 0.01).
Conclusion: Neutrophil CD64 is superior to other sepsis markers for detecting systemic infection or sepsis, since it is not only combines high sensitivity with high specificity but also provides early and rapid results than cultures and CRP.
Keywords: Neutrophil CD64; Marker; Early Sepsis; Newborn Infants
Early onset sepsis can be presented as a fulminant, multisystemic illness during first few days of life or with nonspecific clinical signs of infection. Therefore the diagnosis of early sepsis in newborn infants may need to be differentiated from other conditions that mimic sepsis. Moreover, it is important to differentiate early sepsis from non-infectious respiratory disorders as respiratory distress (RD), aspiration pneumonia, lung hypoplasia, tracheoesophageal fistula and transient tachypnea of the newborn [1]. Sepsis is a major healthcare problem from the perspective of mortality and economics worldwide. A survey done by Ministry of health in Egypt showed that the incidence of neonatal sepsis in 80 neonatal units was 10% of cases admitted to NICUs [2].
Laboratory investigations may be coasty and time consuming; it include complete blood count (CBC), acute phase reactants as C reactive protein (CRP) and microbiological tests as blood culture, CSF, urine, bronchoalveolar lavage, stool and surface cultures. Sepsis score by Rodwell., et al. [3] can be helpful. CRP is synthesized within six to eight hours of exposure to an infective process or tissue damage, with a half-life of 19 hours, and may increase more than 1000 fold during an acute phase response [4].
CD64 is normally expressed in very low concentrations by unstimulated neutrophils. It is considerably upregulated on the trigger of bacterial invasion, and has been shown to be involved in the process of phagocytosis and intracellular killing of pathogens. More importantly, neutrophils from preterm infants express CD64 during bacterial infections to the same degree as those from term infants, children, and adults [5]. So in newborns, neutrophil CD64 have been found to be promising markers for diagnosis of early and late infections [6].
We hypothesized that CD64 can be used as single and rapid test to remove the current subjectivity and uncertainty in the diagnosis and therapeutic monitoring of infection and sepsis, hence can differentiate non-infectious causes of RD from early sepsis among full term infants. This will help to restrict antibiotic therapy which has outstanding importance to reduce both morbidity-mortality rates and multiple drug-resistances in NICU.
The aim of this work is to identify the reliability and utility of CD64 as novel immunological rapid indicator in diagnosis of earlyonset neonatal infection (within 48 hours of age) among full term infants.
It is prospective study that enrolled consecutive infants presenting with early RD, which may be due to sepsis or other causes.
CBC, CRP, blood gases, blood culture and CD64 by flowcytometry were estimated in all included infants at the time of evaluation. The roles of these markers for predicting early sepsis were determined. The study was approved by the Al-Azhar University council.
NICU of Al-Azhar University Hospital.
This prospective study was conducted on 80 term neonates. Sixty (60) of these neonates had been suffered from RD and 20 term healthy neonates as control group. Inclusion criteria include gestational age > 37 weeks, post-natal age < 48 hrs, clinical symptoms of RD, born to mothers with a risk factor for neonatal RD or sepsis, e.g. chorioamnionitis, prolonged rupture of membrane (PROM) > 24 hr, intra- partum fever > 38°C, and infants of diabetic mother, and informed consent from parents. Statistical analysis was done by using SPSS 12 program.
Our cases were assigned to 3 groups according to presence or absence of sepsis and RD:
Results are shown in tables 1-6 and figures 1-4.
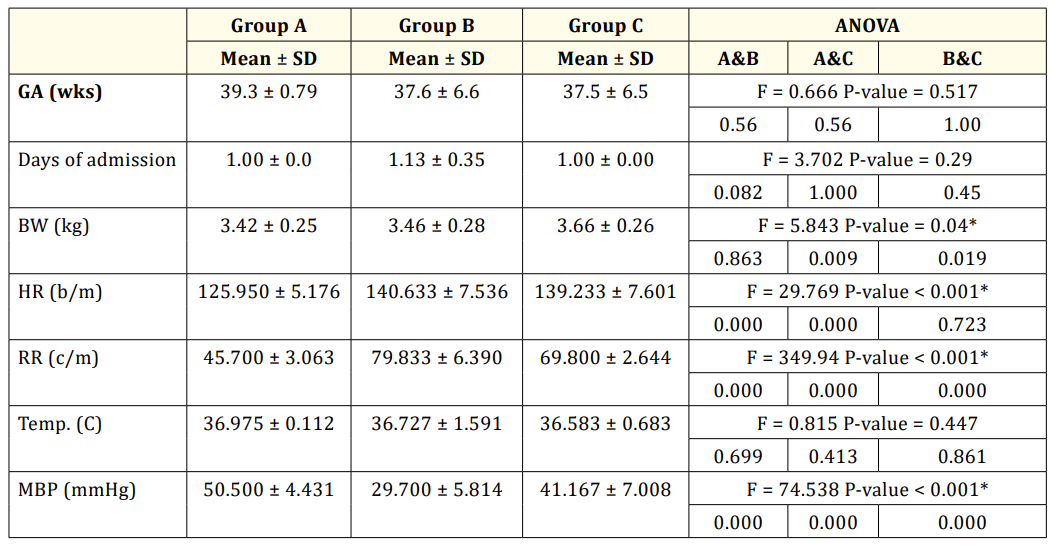
Table 1: Clinical characteristics of the studied groups.
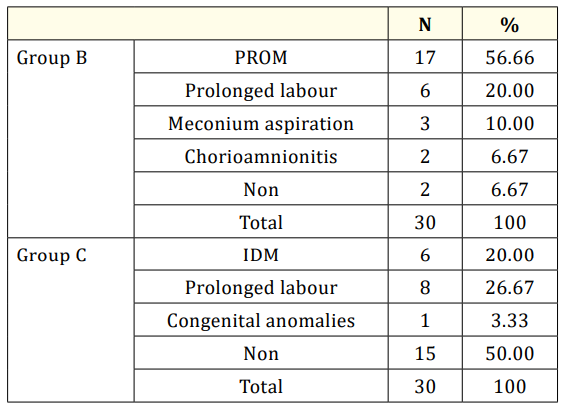
Table 2: Comparison of risk factors in groups B and C.
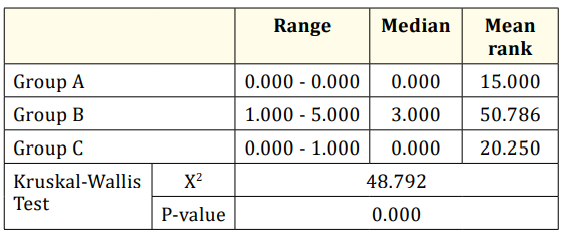
Table 3: Comparison of Rodwell score between group B and C.
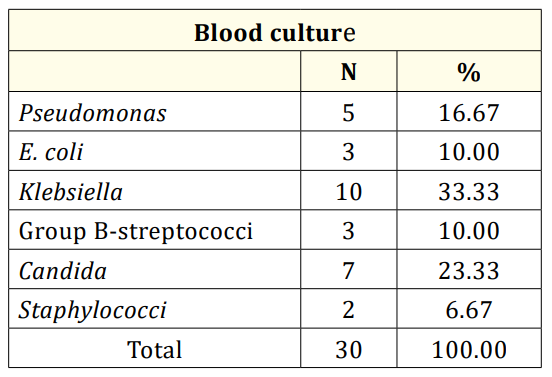
Table 4: Identification of microorganism in the blood cultures of group B.
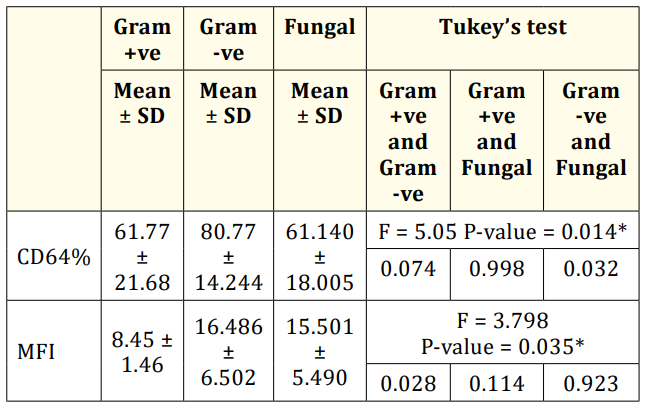
Table 5: Comparison of CD64% and MFI and the organisms of blood culture in patients group B.
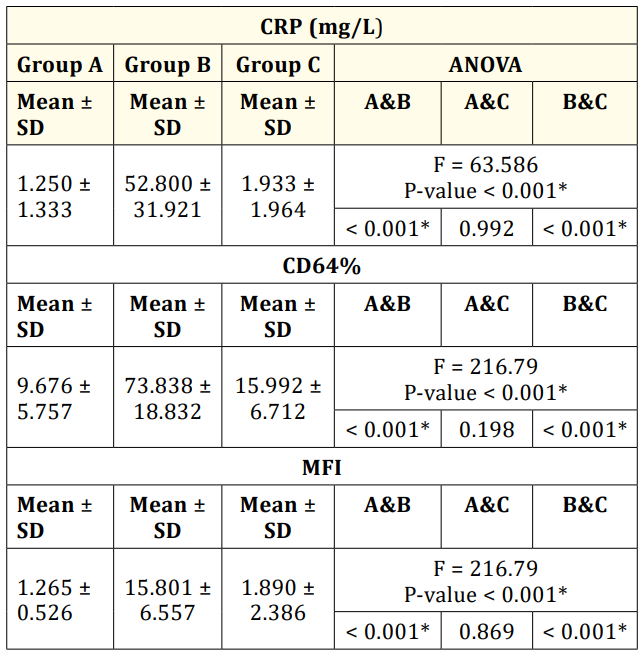
Table 6: Comparison between groups A, B and C in CRP (mg/L), CD64 and % MFI.
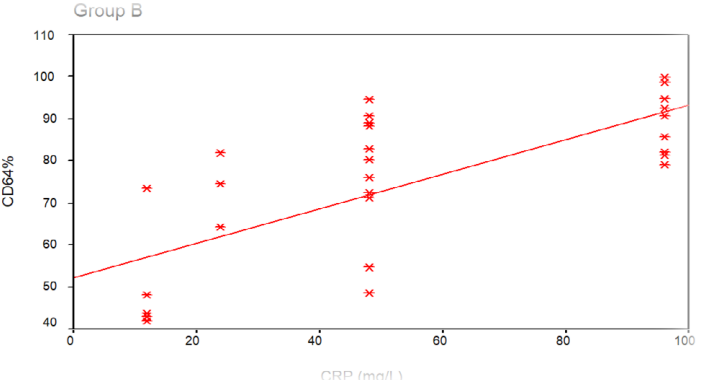
Figure 1: Correlation between CRP and CD 64% in group B.
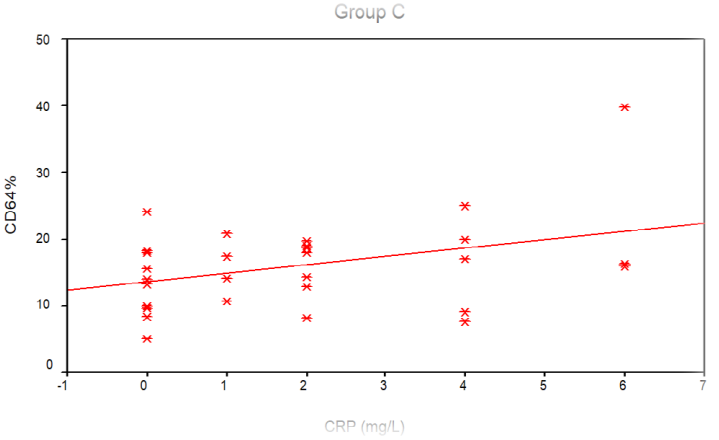
Figure 2: Correlation between CRP and CD 64% in group C.
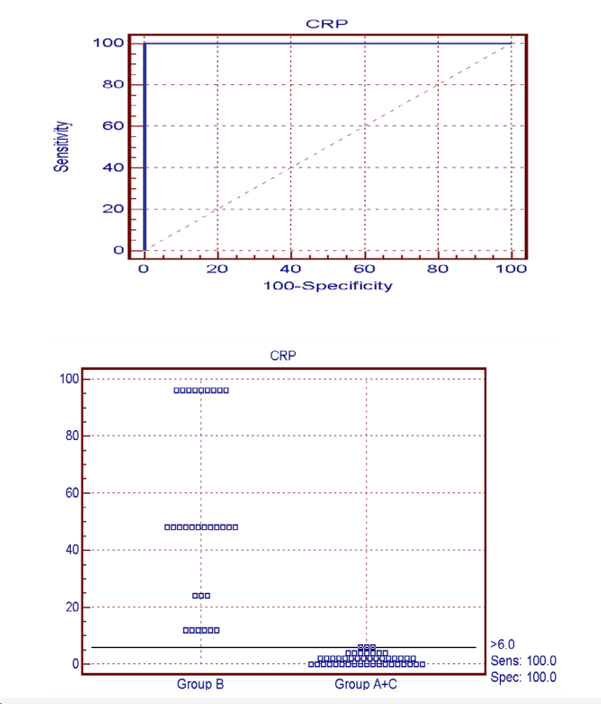
Figure 3: The ROC curve between group B versus groups A+C in CRP. This figure shows the Cutoff value between group B versus A+C > 6 by sensitivity 100%, specificity 100%, PPV 100% and NPV 100% with accuracy 100%.
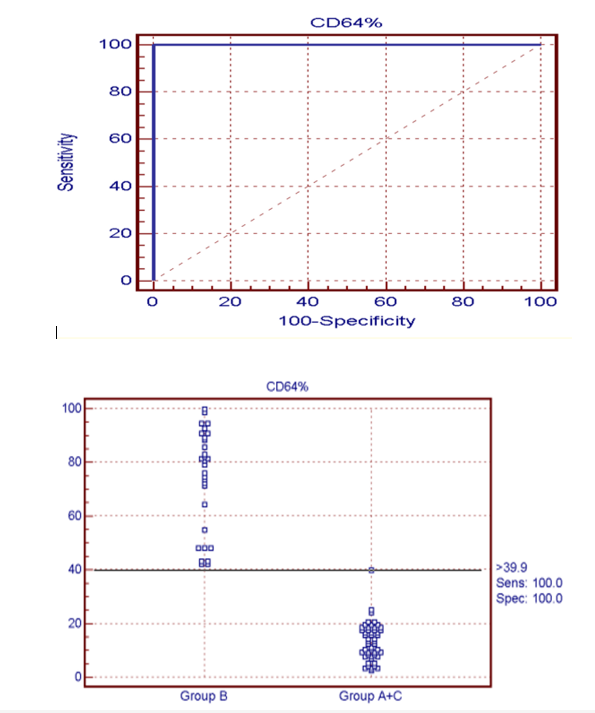
Figure 4: The ROC curve between group B versus groups A+C in CD64%. This figure shows the Cutoff value between group B versus groups A+C > 39.9 by sensitivity 100%, specificity 100%, PPV 100% and NPV 100% with accuracy 100%.
The current study aimed to investigate the reliability of CD64 in the diagnosis of early-onset neonatal infection in full term infants suffering from RD. Eighty infants were enrolled and assigned to 3 groups according to presence or absence of RD/sepsis. The three groups were matched for gestational age, gender, and age of presentation of RD, as patients of group B and C were admitted to our NICU in the first day of life complaining of RD.
As regards risk factors in the studied groups, we found that group B had significant increase in percentage of PROM (56.66%), which was consistent with Liberman., et al. [7] study, who found that PROM > 24 hours is a major risk factor for neonatal sepsis. However 50% of cases of group C had no risk factors at all.
Respiratory distress is the most common symptoms occurring in up to 90% of infants with sepsis; also pneumonia can augment the clinical signs of RD. In our study there was 36.7% of the infected group suffered from pneumonia. Pneumonia in the newborn can be congenital or acquired. Congenital (early onset) pneumonia is characterized by early onset of RD within 3 - 6 hours after birth. The clinical and radiological findings may be very similar to those of hyaline membrane disease or aspiration pneumonia. In acquired (late onset) pneumonia, the onset of RD is usually after the first 24 hours or at any time in neonatal period. It commonly follows aspiration, mechanical ventilation or septicemia [8].
No single laboratory test has been to found to have acceptable specificity and sensitivity for predicting infection. The differential diagnosis of sepsis must be considered. In our study we evaluated several markers as CBC, CRP, and CD64. We used the Rodwell., et al. [4] seven point hematological scoring system for diagnosis of neonatal sepsis, we found highly significant increase in group B than in group C or group A, p < 0.001.
Bacterial cultures should generally reveal the organism of infection within 36 - 48 hours. In this study, most of blood cultures in group B demonstrated the presence of gram negative bacillus Klebsiella (33.33%). Our study was consistent with the results of Laysela., et al.[9] who studied the early markers of neonatal sepsis, but was in contrast to Pak., et al. [10] who stated that E. coli was considered to be the most common responsible organism for early onset sepsis, as we had only 10% cases with E. coli organisms.
In our study, CRP was one of the diagnostic marker of neonatal infection, it was significantly increased among infants with RD and sepsis (Group B) more than (Group C) those with RD without sepsis P < 0.001. CRP at cut off > 6 had high sensitivity and specificity with 100% accuracy. This result was constant with Ng [6] and EL Meneza., et al. [11] results who found CRP as a diagnostic marker for neonatal sepsis had high sensitivity and specificity, however its concentration was increased slowly in the initial phase, and the sensitivity at the time of sepsis evaluation was only 60%.
CD64 represent highly potent trigger molecules for activated neutrophils, CD64 signaling can lead to events as antibodymediated phagocytosis, clearance of microbes, and the release of intracellular cytokines reactive oxygen species [12]. In this study, flowcytometry was used to assess the prevalence of CD64-bearing neutrophils and the mean fluorescence intensity (MFI) of their expression in blood samples from the three groups. The percentage of neutrophils expressing CD64 was with highly significant increase in group B cases when compared to group C cases and healthy neonates of group A as p < 0.001. There was no significant difference between the non-infected respiratory distress cases of group C and control group A. These results were constant with the results of Mishra., et al [4].
As regards to our results, CD64 can be used for differentiation between infected and non-infected neonates presented with RD as the high affinity in CD64 was involved in the process of phagocytosis and intracellular killing of pathogens, also was expressed at a very low level on the surface of unstimulatedneutrophils. During bacterial infection, the expression of CD64 on activated neutrophils was markedly increased [4]. Our study was consistent with Pak., et al. [10] results which found that CD64 was capable of differentiating infected from non-infected conditions such as hypoxic-ischemic encephalopathy, meconium aspiration syndrome and transient tachypnea of the newborns, presenting with similar clinical signs and symptoms.
CD 64 was a sensitive infection marker for both early and late onset neonatal infection, in term and preterm infants [10]. The CD64% cutoff value > 39.9 had sensitivity 100%, specificity 100%, PPV 100% and NPV 100% with accuracy 100%.
The results of the present study also demonstrated a highly significant rise of both CD64% and its expression intensity in newborn infants with gram negative septicemia as compared to those with gram positive septicemia and Candida infection (p < 0.01). This was concordance with the study done by Wallace., et al. [13] who found that the cross linking of Fc gamma RI (CD64) and CD14 (one of the major receptor of endotoxin), in case of gram negative organisms, give rise to rapid and transient phosphorylation of multiple phagocytic intracellular protein enhancing the function.
ROC curve analysis showed no significant difference for the accuracy of CRP and CD64. Accuracy of CD64 and CRP was 100% specificity, sensitivity, PPV, and NPV and the accuracy of MFI was 99.2% with sensitivity 100%, specificity 98%, PPV 96.8% and NPV 100%.
The advantage of using CD64 as a diagnostic marker is that the flowcytometric analysis can be performed with minimal blood volume (0.05 ml of whole blood). The results can be available within 4 hours; the measurement is quantitative and thus enables comparison of results among different centers. The persistent expression of CD64 for at least 24 hours gives the marker a wide diagnostic window and the very favorable diagnostic utilities render CD64 one of the post-infection markers for the identification of early and late onset neonatal sepsis [14]. Early diagnosis of Sepsis is important to ameliorate morbidity of vital organs and affect patient survivals [15,16].
CD 64 is a probably emerged as useful highly sensitive marker for detection of early onset neonatal infections in full term infants. Measurement of neutrophil CD64 may allow neonatal clinicians to discontinue antibiotic treatment at 24 hours in infants who are clinically stable and whose CD64 expressions are below the optimal cutoff level. Prospective studies incorporating CD64 into a sepsis scoring system are warranted. Also flowcytometry have allowed measurement using only minimal blood volume. Neutrophil CD64 is superior to other sepsis markers for detecting systemic infection or sepsis, since it is not only combines high sensitivity with high specificity but also provides early and rapid results than cultures and CRP
Judicious selection of a panel of sepsis markers with complementary properties could greatly increase the ability of neonatologists to diagnose infection and discern valuable prognostic information.
Copyright: © 2018 Safaa A EL Meneza., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.