Keerthi AR, Sai Divya Yadavalli and Kumaravel S*
Department of Pediatric Surgery, JIPMER, Pondicherry, India
*Corresponding Author: Kumaravel S, Additional Professor and Head, Department of Pediatric Surgery, JIPMER, Pondicherry, India.
Received: July 30, 2018; Published: August 29, 2018
Citation: Kumaravel S., et al. “Preoperative Nutritional Screening as a Predictor of Post-Operative Outcomes in Children Undergoing Major Surgery - Retrospective Evaluation of Modified Malnutrition Universal Screening Tool”. Acta Scientific Paediatrics 1.2 (2018):33-37.
Aim: To assess the nutritional status in children pre-operatively and to evaluate its role in predicting postoperative outcomes using modified Malnutrition Universal Screening Tool (MUST).
Methods: A retrospective review of 158 children admitted under Pediatric surgery JIPMER, was carried out using modified MUST. They were divided into three risk groups according to MUST as high, medium and low. Parameters such as age, diagnosis and procedure done, weight of the child and postoperative complications were studied.
The postoperative complications such as sepsis, surgical site infection, leak, re-exploration in each child was correlated to their Nutritional risk groups obtained using MUST.
Result: A total of 158 children of age 1 - 13 years satisfying the inclusion and exclusion criteria were evaluated. 92 were boys and 66 were girls. A total of 90 children fell under MUST-0 (Low risk), 33 under MUST-1 (medium risk) and 35 under MUST-2 or more (high risk).
The percentage of children having postoperative complication under MUST-0 (Low risk) was 5.6% while that in MUST-1 (medium risk) was 27.3% and MUST-2 or higher (high risk) was 48.6%.
Hence, on comparison with Total MUST Score 0 (low risk) MUST-1 (medium risk) had 6.3 times more risk of postoperative complications (p = 0.002) and MUST-2 or more (high risk) had 16 times more risk of postoperative complications (p = 0.001).
Conclusion: This study confirms the long held belief under-nutrition is related to increased complications. Modified MUST score predicts the children at risk of postoperative complications. Caution while taking up under nourished children for elective surgery is probably prudent.
Keywords: Malnutrition Universal Screening Tool (MUST); Pediatric Perioperative Screening; Nutritional Screening; Surgical Outcomes
MUST: Malnutrition Universal Screening Tool; STAMP: Screening Tool for the Assessment of Malnutrition in Pediatrics; STRONGkids: Screening Tool for Risk On Nutritional status and Growth; SGNA: Subjective Global Nutritional Assessment; SSI: Surgical Site Infections; BMI: Body Mass Index
Over the past few decades, enormous progress has been noted in decreasing pediatric surgical mortality and morbidity primarily due to improved surgical techniques and anesthesia. However, currently other factors that impact surgical outcomes are being increasing looked at. One such important factor is undernutrition.
The prevalence of malnutrition particularly undernutrition, among pediatric inpatients ranges from 24 - 80% in different studies/ countries [1,2]. A large number of these patients are undernourished when admitted to the hospital and in majority of these patients; undernutrition develops/worsens further while in hospital [3].
It is also a well-known fact that undernutrition is associated with various negative outcomes such as increased risk of infection and postoperative complications, impaired wound healing and increased hospital stay. Many of these can be prevented if special attention is paid to nutritional care. While other features of a patient’s primary disease such as dehydration, fever etc. are being routinely looked for and treated, it is unacceptable that nutritional problems that are associated with significant and multiple risks are not identified and treated. Though there are many guidelines for assessment of nutritional status in adults such as MNA, NRS and MUST, a reliable and universally accepted tool is not available for children [4]. Consequently, many different tools have been developed such as STAMP (Screening Tool for the Assessment of Malnutrition in Pediatrics) [5], STRONGkids (Screening Tool for Risk On Nutritional status and Growth) [6], SGNA (Subjective Global Nutritional Assessment) [7] and others which differ in criteria used to assess nutritional status, their aims and applications [8].
In a developing country like India, a nutritional screening tool needs to be developed that not only identifies patients who are malnourished but also predicts and identifies poor surgical outcomes. Hence, the Malnutrition Universal Screening Tool (MUST) modified within our institution by replacing BMI with criteria more suitable for assessing under-nutrition in children has been used. Through this tool not only nutritional status of pediatric patients were assessed but also an attempt has been made to correlate the scores to predict the surgical outcomes and identify patients at risk of poor outcomes.
A retrospective study was conducted in a tertiary care hospital in a developing nation (JIPMER, Pondicherry, India). All consecutive children who underwent major surgery and fulfilling the following inclusion and exclusion criteria during the period of January to April 2016 were included in the study. Infants i.e. less than 1 year of age and children beyond 13 years of age were excluded (local hospital policy for admission in pediatric surgery is less than 13 years). All children who had minor surgery or day care cases were excluded from the study. Neurosurgical and cardiac surgery cases were excluded. Children were mostly admitted for genitourinary including renal/bladder surgeries, gastrointestinal surgeries and thoracic surgeries.
Sample size was calculated using a calculator for proportions with a confidence level of 99%, a power of 85%, and proportion in group 1 to be 60% was found to be 157.
The MUST modified tool assesses nutritional risk of a child based on three criteria, viz. weight loss in the last 3 - 6 months, presence of acute diseases or absence of nutritional intake for more than 5 days in the perioperative period, lastly presence and severity of existing malnutrition, for which we have used the Gomez classification for malnutrition. Each component is scored from 0 - 2 and a total score calculated. Low risk is assigned if total score is zero, medium risk if score is one and high risk if score is two or more (Table 1).
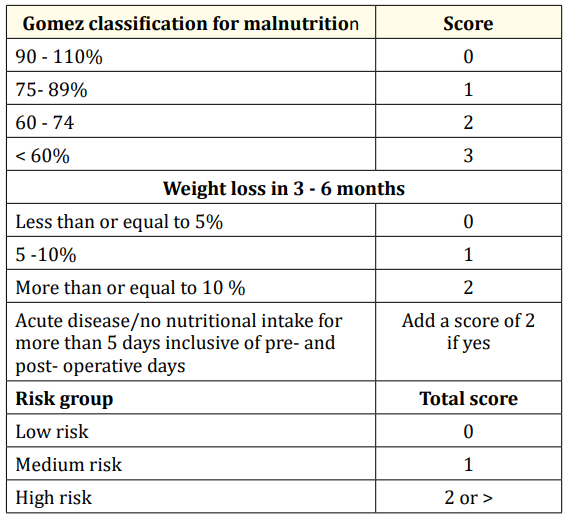
Table 1: Malnutrition Universal Screening Tool (MUST) - modified.
The Demographic details, admission and discharge weight, procedure done, postoperative complications such as Surgical site infection(SSI), leak, reoperation, sepsis and others, were extracted from the records and entered in a pro-forma. The percentage for reference weight for age was calculated by obtaining weight of the child included in the study and weight of a normal child of same age using IAP charts for boys and girls separately:
Percentage for reference weight for age = weight of the child x 100
weight of a normal child of same age
Statistical analysis was done using software package SPSS v 21 and parameters such as Postoperative complications and Total score obtained on using MUST were analysed using Pearson ChiSquare test.
A total of 158 children were evaluated in the age group of 1 - 13 years of which 92 were males and 66 were females.
90 of 158 children fell under MUST-0, 33 under MUST-1 and 35 under MUST-2 or more (Table 2). Out of the 90 children under MUST-0, 85 (94.4%) had uneventful postoperative course while 5 (5.6%) had postoperative complications. Similarly, of the 33 under MUST-1, 24 (72.7%) had an uneventful postoperative course while 9 (27.3%) children had postoperative complications. Among the 35 children with MUST-2 or more, 18 (51.4%) had no postoperative complications while 17 (48.6%) had postoperative complications.
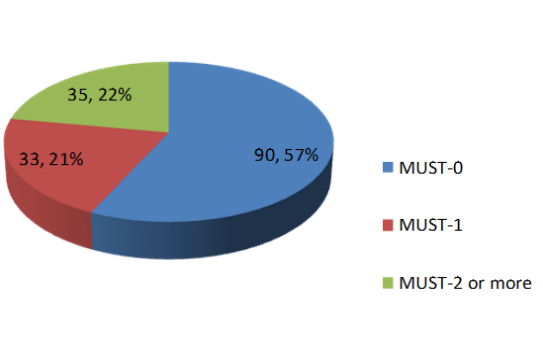
Figure 1: Distribution of children as per MUST score.
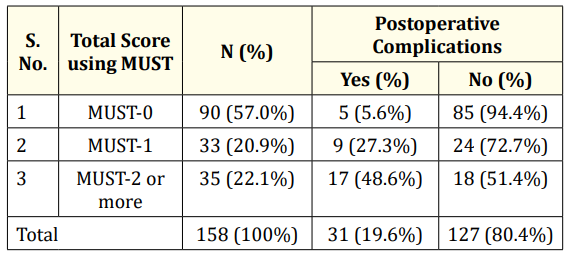
Table 2: Correlation between postoperative
complication and MUST score.
N: Number of Children; MUST: Malnutrition Universal Screening
Tool
In comparison with total MUST Score 0, children falling under MUST-1 had 6.3 times more risk of postoperative complications with a p value of 0.002 and an odds ratio of 6.375, while children with MUST-2 or more had 16 times more risk of postoperative complications with a p value of 0.001 and an odds ratio of 16.056. Among the 31 patients with postoperative complications, 24 (77.4%) developed surgical site infection (SSI) of which 12 belonged to MUST-2 or more, 7 to MUST-1 and 5 to MUST-0 with a p value of 0.0005.
The proportion of patients malnourished in paediatric surgical population under study was 43% as estimated by Gomez classification; 25.3% having mild malnutrition, 14.5% moderate malnourishment and 3.16% with severe malnourishment.
The current study is an evaluation of the screening tool, MUST modified for children in assessing the nutritional status among pediatric inpatients preoperatively and correlation with their postoperative outcomes.
The original MUST tool was validated for use in different settings and was able to predict length of stay and mortality in elderly hospitalised patients [9,10]. But when studied in cardiac surgical patients, risk categorization obtained using the tool was not associated with outcomes [11]. However MUST (modified) seemed to be successful in being co related with complications of surgery in our study, with a 6.3 times increased risk if score was 1 and 16 times more risk if score was 2 or more. The modified version of MUST was developed for use in children by excluding BMI which is not a suitable measure of under-nutrition in the pediatric age group.
Among the 31 patients with postoperative complication in our study, 24 (77.4%) developed surgical site infection of which 12 belonged to MUST-2 or more, 7 to MUST-1 and 5 to MUST-0 with p value of 0.0005 (Table 3) showing a significant co-relation of MUST scores and development of Surgical Site Infections (SSI). Previously identified risk factors include age, race, procedure duration [12]. We believe under-nutrition as assessed by MUST may also be added to this list.
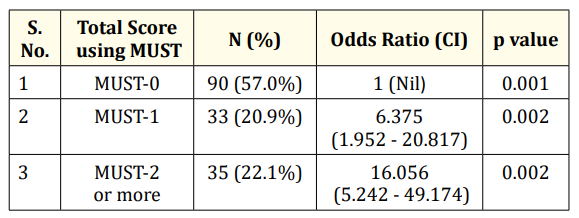
Table 3: Postoperative complication risk prediction
using MUST score.
N: Number of Children; CI: Confidence Interval; MUST:-
Malnutrition Universal Screening Tool
In a recent study involving hospitalized children (not undergoing surgeries), higher incidence of infectious complications was observed in high risk group compared to children categorized as having moderate risk. The study also showed that a correlation existed between other poor clinical outcomes including, prolonged hospitalization, greater weight loss and higher expenses, and risk stratification [13]. Our study confirms the same in children undergoing surgery i.e. increased postoperative complications with increasing risk scores.
However, there is a lack of literature evaluating the ability of nutritional risk assessment tools in assessing surgical outcomes.
As ours is a retrospective study we have presented only a limited data with a very narrow focus. More data including length of stay, specific complications, etc. should probably be studied on a prospective basis which we are planning. No attempt was made in studying nutritional intervention to see if it impacts incidence of postoperative complications in this study. On account of these findings, we believe that further prospective studies evaluating the reproducibility of the MUST modified tool in surgical patients are necessary as it could potentially be an ideal tool for use in developing countries.
From the proportion of malnutrition in the sample population i.e. 43%, a high prevalence of malnutrition was estimated in children undergoing surgeries in a developing country, which emphasizes the need for further studies aimed at identifying a tool suitable for nutritional risk assessment in developing countries.
This study confirms the long held belief that under-nutrition among surgical patients peri-operatively is related to increased postoperative complications. MUST score adapted to children predicts the children at risk of postoperative complications. Further studies involving larger groups of children are needed to confirm these findings and to clearly establish a valid tool for predicting surgical outcomes as related to nutrition in the setting of a developing country. We would also recommend caution while taking up undernourished children for elective surgery and an attempt at improving nutrition is probably prudent and should be the subject of future studies.
There exists no financial interest or any conflict of interest.
Copyright: © 2018 Kumaravel S., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.