Doaa M Youssef1*, Muftah Th Ben Yousef1, Amal S Alshal2 and Abdel-Raziq El-Shiekh1
1 Pediatric Department, Zagazig University, Egypt
2 Assistant Professor of Biochemistry, Zagazig University, Egypt
*Corresponding Author: Doaa M Youssef, Pediatric Department, Zagazig University, Egypt.
Received: July 27, 2018;; Published: August 22, 2018
Citation: Doaa M Youssef., et al. “Effect of Phototherapy Treatment of Neonatal Jaundice on Blood Endothelin and Nitric Oxide Levels: Clinical Significance in Preterm Infants”. Acta Scientific Paediatrics 1.2 (2018):24-28.
Neonatal hyperbilirubinemia is one the commonest cause of admission in NICU, phototherapy is the golden stand red therapy long time ago, which showed efficacy and it's side effects should be studied in depth. Both nitric oxide (NO) and endothillin1 (ET1) are potent vasodilation and vasoconstrictor which may be affected by phototherapy; so we aimed to investigate impact of phototherapy on their levels both in full term and preterm and if there is relation with hemodynamical stability in treated neonates. In this study we tested 38 neonate before and after phototherapy and We measured NO and ET1 levels also we assessed Heart rate blood pressure before and after therapy, we found significant rise in both NO and ET1 after phototherapy both in full term and preterm with no difference between full term and preterm, we found also a significant correlation between each of age, Heart rate and diastolic blood pressure and each of NO and ET1, but there is no significant correlation of systolic blood pressure and both NO and ET1. We concluded that we have to monitor heart rate and blood pressure specially diastolic in neonates treated with phototherapy for hyperbilirubinemia as they may be affected as a result of effect of phototherapy on both NO and ET1.
Keywords: Phototherapy Treatment; Neonatal Jaundice; Endothelin; Nitric Oxide
Neonatal jaundice is defined as yellowish discoloration of skin, sclera of eyeball, and mucous membranes caused by deposition of bilirubin these tissues. Depending upon the cause, jaundice may be present at birth or any time during the neonatal period. Jaundice due to either indirect (un-conjugated) or direct (conjugated) bilirubin within the first 24 hours of life should be taken seriously [1].
Phototherapy has remained the standard of care for the treatment of hyperbilirubinemia in infants for four decades. Efficient phototherapy rapidly reduces the serum bilirubin concentration [2] and it is generally regarded as safe method; the reported side effects have been subjected to extensive and controversial debate, and include rashes, loose green stools, water loss, oxidative injury, dehydration and ocular hazards [3].
One of the most noticeable clinical complication of phototherapy is “bronze baby syndrome”, a grayish-brown discoloration of the skin that occurs exclusively in infants with cholestatic jaundice [4]. Phototherapy treatment has been suggested to alter heart function by increasing the heart rate and diminishing the variability of heart rate and cardiac output while affecting blood vessel function by diminishing the mean arterial blood pressure and increasing peripheral blood flow. After phototherapy treatment closure of PDA may be affected via alteration of the fluid homeostasis and cardiovascular function [5]. Effect of phototherapy on the autonomic nervous system modulation of heart rate in term neonates are apparent as significant diminution in heart rate variability was documented during phototherapy, a phenomenon assumed to be centrally mediated. The reasons for this decrease are yet unknown [6].
NO has been noted to relax the smooth muscle and walls of arterioles. The complex endothelial cells lining the blood vessels release a puff of NO at each systole, which gets diffused into the underlying smooth muscle cell, and thus permits the surge of blood to pass through easily [7].
The pharmacological action of ET-1 is very unusual compared with other vasoactive mediators such as ANGII. It remains the most powerful constrictor of human vessels discovered with a remarkably long-lasting action [8].
Nitric oxide (NO) and endothelin-1 (ET-1) are natural counterparts in vascular function, and it is becoming increasingly clear that an imbalance between these two mediators is a characteristic of endothelial dysfunction and is important in the progression of vascular disease [8].
We aimed at this study to evaluate the effect of Phototherapy used for treatment of neonatal hyperbilirubinemia on the blood levels of nitric oxide (NO) and Endothelin (EN) and their hemodynamic effects on both full term and preterm neonates.
Thirty eight newborn with hyperbilirubinemia requiring phototherapy in the neonatal intensive care unit of Zagazig university hospital were studied. Among them twenty (20) patients were full term and eighteen (18) were preterm. All patients were treated with phototherapy for more than twenty four (24) hours.
Blood samples were collected before and after phototherapy. The amount of endothelin (ET) in the blood samples was determined by radio immuno assay and nitric oxide (NO) levels were determined using nitrate reductase.
Heart rate (HR) and blood pressure (BP) were monitored and recorded before and after twenty four (24) hours of phototherapy.
We included both preterm and full term neonates, both genders (Male - Female) during first month of life.
We excluded neonate with the following criteria: Neonates with clinical sepsis or laboratory evidence of sepsis, Neonates with direct hyperbilirubinemia, those with Major congenital malformation of cardio vascular, pulmonary, central nervous system, history of birth asphyxia and congenital infection.
All neonates were subjected to clinical assessments by: Complete history taking, Complete physical examination WT, CNS, CVS, Respiratory, ABD, Investigation either Routine Investigations [CBC, Blood group, Comb's test and Serum bilirubin (total and direct)], or Special Investigations by ELIZA [Endothelin (EN) and nitric oxide (NO) before and after twenty four (24) hours of phototherapy].
The collected data were tabulated and analyzed using SPSS version 16 software (SpssInc, Chicago, ILL Company) Categorical data were presented as number and percentages while quantitative data were expressed as mean ± standard deviation, and range. Quantitative data were tested for normality using Kolmogorov Smirnov test, assuming normality at P > 0.05, using Student "t" if normally distributed. The accepted level of significance in this work was stated at 0.05 (P < 0.05 was considered significant).
We found that age of the studied group ranged from one day to 15 days with mean of 6.3 ± 8.72 days, weight ranged from 1800 gm to 3900 gm. 52.6% of the studied neonates were males and 47.4% females. 18 were preterm and 20 full term, total bilirubin of the studied group ranged from 7.97 to 33, while direct bilirubin ranged from 0.38 to 2.9 with mean of 0.76 ± 0.48.
Table 1 shows a high statistical significant increase in both endothelin and nitric oxide as both of them were higher after treatment in both full term babies and preterm, while there were no differences as regard Hb, bilirubin total or direct between full term and preterm.
Table 2 shows that there was no statistical significant difference between pre-term and full-term infants regarding heart rate, systolic BP and diastolic BP before and after treatment with phototherapy.

Table 1: Difference in laboratory data among full-term and pre-term.
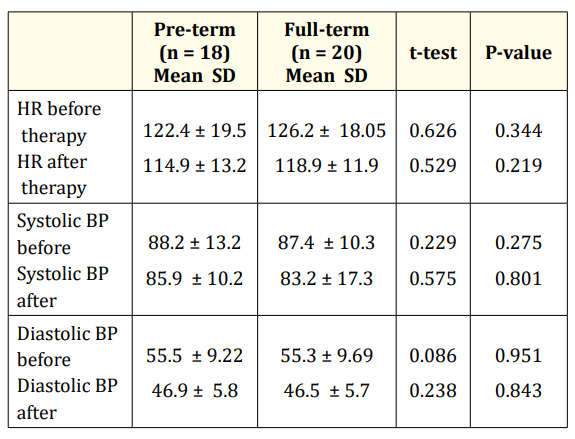
Table 2: Difference in heart rate and blood pressure among pre- and full-term.
While table 3 shows that there was no statistical significant difference between pre-term and full-term infants regarding endothelin and nitric oxide levels before and after treatment with phototherapy, table 4 shows there is significant rise in both NO and ET1 after phototherapy in both full term and preterm.
We found a significant correlation between each of age, Heart rate and diastolic blood pressure and each of NO and ET1, but there is no significant correlation of systolic blood pressure and both NO and ET1 as shown in table 5.

Table 3: Difference in endothelin and nitric oxide level among pre- and full-term.

Table 4: Difference in endothelin and nitric oxide before and after phototherapy among full-term and preterm.

Table 5: Correlation between both endothelin and nitric oxide with age and delta change (between basic and after phototherapy) and clinical data of the studied group
Phototherapy is the most common therapeutic intervention used for the treatment of hyperbilirubinemia. Although it has become a mainstay since its introduction in 1958, a better understanding of its efficacy and safety is necessary for more predictable and improved clinical practices and outcomes.
ET and NO are the strongest vasoconstrictor and vasodilator respectively. Their effects are completely opposing and under physiological conditions they regulate angiostasis and blood flow. In some pathological conditions however, the dynamic balance between ET and NO is disturbed, causing changes in hemodynamics that might lead to severe clinical symptoms.
In present study we investigated 40 neonate (18 preterm and 20 full term), treated for hyperbilirubinemia without other pathological condition and we measured serum NO and endothelin before and after therapy with recording their clinical data specially HR, systolic and diastolic blood pressure.
The present study showed a significant rise in ET levels and NO after phototherapy in both full term and preterm newborn infants.
Others [9,10] also have reported that NO level was significantly higher than the baseline level only in preterm infants with GA ≤ 32 weeks ET and NO are vasoactive substances with opposing effects. They regulate blood vessel tension and hence maintain the blood flow under physiological conditions. There is a feedback regulation between them; the release of NO will be promoted when ET combines with its ß receptor at the blood vessel endothelium, and NO can inhibit the release of ET contrarily in pathological conditions, however, the dynamic equilibrium between NO and ET is upset, leading to changes in hemodynamics and clinical symptoms.
We found that HR and diastolic blood pressure significantly change after phototherapy both in preterm and full term but there was no significant change in systolic blood pressure. ET and NO are vasoactive substances with opposing effects. They regulate blood vessel tension and hence maintain the blood flow under physiological conditions. There is a feedback regulation between them: the release of NO will be promoted when ET combines with its B receptor at blood vessel endothelium, and NO can inhibit the release of ET contrarily.
We found negative correlations between both NO and endothelin levels with Age, HR, and diastolic blood pressure but there is no correlation between each of the two parameters and systolic blood pressure, These correlations were found in both full term and preterm.
This match a study by another study [10] revealed a significant decrease in both systolic and diastolic blood pressure and a significant increase in HR after 24 hours of phototherapy in both groups of newborns. These results are consistent with previous reports. These results have led to the speculation that phototherapy induces vasodilatation via increased NO production which led to the significant fall in MABP. The significant increase in HR may be compensatory to the fall of MABP or due to the effect of increased NO level. Increased NO level is associated with an increase in heart rate, and this is thought to be due to a neurally mediated reflex response.
Another hypothesis is that NO can affect pacemaker activity leading to an increase in heart rate. Although the present study revealed a significant decrease in MABP and a significant increase in HR in full term and preterm newborn infants, these changes occur within the normal range of MABP and HR in the neonatal period [9].
We concluded that phototherapy leads to rise in both NO and endothelin ET that may impact hemodynamics especially HR and diastolic blood pressure, We recommend close monitoring to vital signs particularly HR and Blood pressure during phototherapy treatment of jaundiced newborn.
World Journal of Pediatrics 14.1 (2008): 31-35.
Journal of Neonatology Research 4.1 (2014).
Copyright: © 2018 Doaa M Youssef., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.