Soumaro Kanaté Daouda1*, Aka Kouamé Evrard Vianney Medgar1, Mobiot Aka Christelle Désirée-Thérèse2, Coulibaly Amadou Marcellin1, Kouadio Samah David1, Coulibaly Nahoua Alassane1, Boka Eva Rebecca1, Zambi Doua Audric-Aimé1, Sess Rodolph Arthur Delorh3, Sy Abdel Kader1, Kacou Aka Désiiré1, Traoré Alidou2 and Sie Essoh Jean-Baptiste1
1Trauma, Orthopedics and Reconstructive Surgery Department of the Yopougon University Hospital Center, Côte d’Ivoire
2Orthopedics, Traumatology and Plastic Surgery Department of the Angré University Hospital Center, Côte d’Ivoire
3Orthopedic Trauma Department Saint Joseph Moscati Catholic Hospital Yamoussoukro, Côte d’Ivoire
*Corresponding Author: Soumaro Kanaté Daouda, Trauma, Orthopedics and Reconstructive Surgery Department of the Yopougon University Hospital Center, Côte d’Ivoire.
Received: September 04, 2024; Published: September 20, 2024
Citation: Soumaro Kanaté Daouda., et al. “Epidemiology, Indications and Results of Intermediate Hip Arthroplasty in Tropical Setting”. Acta Scientific Orthopaedics 7.10 (2024): 27-32.
Introduction: Fractures of the femoral neck are common in the osteoporotic elderly following minor trauma. They are usually treated surgically. Arthroplasty treatment of femoral neck fractures is currently poorly codified. In sub-Saharan Africa, the use of intermediate hip arthroplasty is recent. The aim of this study was to analyse the epidemiological profile and indications for intermediate hip arthroplasty, and to assess the short and medium-term functional results.
Patients and Method: We conducted a retrospective study of 77 patients treated with intermediate hip Arthroplasty. The study was conducted over a period of seven (07) years. All patients hospitalized for a femoral neck fracture treated with an intermediate hip arthroplasty and with a minimum follow-up of 5 years were included. Pathological fractures were excluded. Epidemiological, diagnostic, therapeutic and evolutionary data were collected f or each patient. Functional results were assessed using the Postel and Merle d’Aubigné method. Epi info7 was used to analyse the data.
Results: The average age was 57. The patients were 48 men and 29 women. Aetiologies were dominated by domestic and road traffic accidents. The average time between trauma and surgery was 73.48 days. The majority of patients had a pre-injury walking ability of 9 according to the Parker score. Pseudarthrosis of the neck was found in 41 patients (53.25%). The Moore posterolateral approach was used in all cases. The mean follow-up was 7.6 months. We noted 1 early dislocation, 4 loosening and 18 osteoarthritis of the acetabulum. The average functional results were very good in the short and medium term.
Conclusion: The average age was 57. Road traffic accidents accounted for 40.26% of aetiologies. The fractures were old lesions. Despite a high rate of osteoarthritis of the acetabulum, functional results were very good in the medium term.
Keywords: Epidemiology; Hemiarthroplasty; Intermediate Arthroplasty; Functional Result; Tropical Setting
Fractures of the proximal end of the femur, in particular femoral neck fractures, are common injuries in trauma [1]. They occur mainly in the osteoporotic elderly following minor trauma with a life-threatening prognosis [2]. They are less common in young people following violent trauma. They are usually treated surgically. This may involve osteosynthesis or arthroplasty [1, 2]. Osteosynthesis remains the method of choice in patients under 70 years of age. Arthroplasty treatment of femoral neck fractures is currently poorly codified. Unipolar or bipolar hemiarthroplasty (intermediate hip arthroplasty) has long been the treatment of choice for surgical management of femoral neck fractures in elderly patients with no coxarthrosis [3]. In sub-Saharan Africa, life expectancy is 60 years on average [4]. Most series of femoral neck fractures have an average age of 65 years, a relatively young age compared with European series [5,6]. Osteosynthesis, which should be the first choice, is sometimes impossible to perform because of delays in consultation. When osteosynthesis is possible, it is performed open surgery, with the attendant complications of pseudarthrosis of the femoral neck and avascular necrosis of the femoral head [7]. When arthroplasty was performed, it was of the unipolar type.
For the past ten years or so, intermediate hip arthroplasty have been produced in the public sector, notably at the Yopougon University Hospital.
The objectives of this study were to analyse the epidemiological profile of the patients, to analyse the surgical indications and to evaluate the functional results in the short and medium term of intermediate hip arthroplasty.
We conducted a retrospective study of 77 patients treated with intermediate hip arthroplasty in the traumatology, orthopaedics and reconstructive surgery department of the Yopougon University Hospital. The study was conducted over a period of seven (07) years, from 1 January 2012 to 31 December 2018. All patients aged over fifteen (15) years hospitalized for a femoral neck fracture treated with an intermediate prosthesis and with a minimum follow-up of 5 years were included. Pathological fractures caused by tumour or infection, fractures associated with acetabular lesions and cases that could not be analysed were excluded.
Low molecular weight heparin was routinely administered from admission to 6 weeks post-operatively. All our patients received antibiotic therapy from induction of anaesthesia until complete healing. In most cases, this consisted of thirdgeneration cephalosporins combined with imidazole. Fusidic acid combined with fluoroquinolones was used as an oral relay. Patients were monitored clinically and paraclinically until they were able to walk and carry out activities of daily living. Passive rehabilitation began on Day 1 postoperatively. It was entrusted to the rehabilitation specialists. All patients were reviewed at one month post-operatively, then every three months and then every six months. After one year, patients were seen once a year.
For each patient, the following data were collected using a survey form: age, sex, history, previous autonomy, date and circumstances of the trauma, consultation time, clinical examination on admission, Garden classification, preoperative diagnosis, operative time, approach, operative time, hospital stay, intraoperative incidents, evolution at 6 months, 1 year, 3 years and 5 years. The Merle d’Aubigné and Postel Method (PMA score) was used to assess our functional results [8].
The tables were compiled using WORD and EXCEL 2010, and the data was analysed using epi info7.
The mean age was 57, with extremes of 27 and 94. There were 45 patients aged 60 and over (58.4%) and 32 under 60 (41.6%). There were 48 male p atients (62.34%) and 29 female patients (37.66%). The aetiologies are shown in Table 1. The average time from trauma to surgery was 73.48 days with extremes of 1 day and 128 days. Walking independence prior to the trauma was 9 according to the Parker score for 70 patients (90.91%), 8 for 5 patients (6.49%) and 7 for 2 patients (2.6%). Past history is shown in Table 2. Pseudarthrosis of the neck was found in 41 patients (53.25%). Of the recent fractures, 29 (37.66%) were Garden type IV and 07 (09.09%) were type III. The Moore posterolateral approach in its minimally invasive version was used in all cases. The average operating time was 48 minutes. No intraoperative incidents were reported. The mean follow-up was 7.6 years, with extremes of 5 and 9 years. We noted 1 early dislocation at one month postoperatively. No infections or thromboembolic complications were noted. In terms of late complications, we noted 4 (3.08%) prosthetic loosening and 18 (13.86%) Cotyloiditis. 13 cases of cotyloiditis were found in patients under 60 years of age and 5 in those over 60 (all between 60 and 70). At 6 months, all patients had the same Parker score as before the fracture. The functional results are summarised in Table 3.
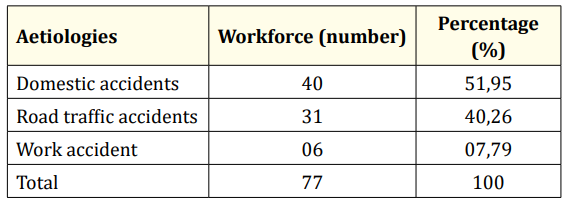
Table 1: Distribution of patients according to aetiology.
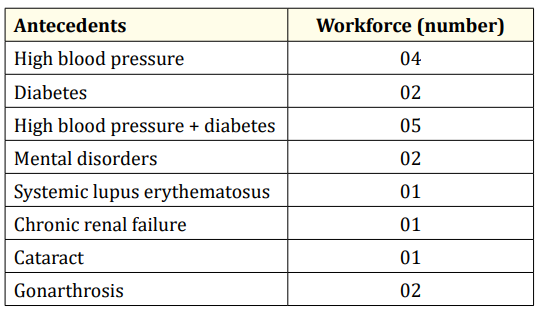
Table 2: Distribution of antecedents.
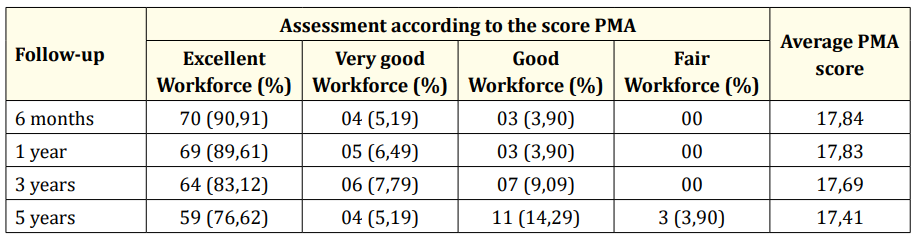
Table 3: Evaluation of patients according to the PMA score according to follow-up.
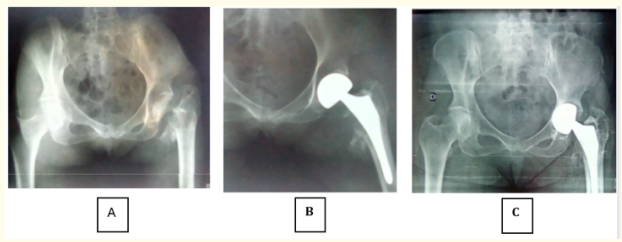
Figure 1: Intermediate hip prosthesis in a 63-year-old patient.
A = Pseudarthrosis of the femoral neck
B = Postoperative control at D1
C = Control at 3 years postoperative with cotyloiditis.
The problem of intermediate hip arthroplasty in our daily practice remains a topical issue. The choice of an intermediate or total prosthesis depends on the surgeon [9-12]. This choice is also linked to working conditions.
Our study was retrospective, with a small sample size and a short average follow-up time. These three factors could constitute biases.
The mean age of our patients was 57 years, with 58.40% aged 60 years and over and 41.60% under 60 years. This age is significantly lower than that found in virtually all publications [13,14]. The youth of our series is due to the relatively low life expectancy in subSaharan Africa compared with European society [4]. In European series, the predominance of females was as high as 80% [14,15], in contrast to our study where the predominance of males was 62.34%. This male predominance has also been found in African series [16]. It could be explained by the mechanism of injury in our series. Contrary to the literature, where domestic accidents accounted for 86.6% of aetiologies [17], road traffic accidents accounted for 40.26%. The proportion of cervical fractures caused by road traffic accidents in our study could be explained by the high proportion of young patients in our series.
The average delay between the trauma and the operation was excessively long at 73.48 days. This long delay was justified by the delays in consultation, which reached 128 days. This delay did not exceed 10 to 15 days for recent fractures. Delayed consultations are mainly due to the use of traditional treatments and the lack of technical facilities in our hospitals [18]. The correction of any chronic medical pathologies and the time needed to raise the necessary funds mean that surgery is almost always delayed beyond the 48th hour, the maximum time recommended by the French Society of Anaesthesia and Intensive Care [19]. As in the rest of the literature, diabetes and hypertension were the most common antecedents [20,21].
We noted 46.75% of recent fractures and 53.25 of neglected or fractures. this distinction has therapeutic and evolutionary significance. Old fractures haves often been treated traditionally. Inappropriate traction, massage and support during traditional treatment lead to remodelling of the perifractural soft tissues and significant displacement. These two factors are likely to lengthen the operating time, as well as functional recovery, due to the degeneration of the gluteal muscles. Traditional massage is likely to lead to postoperative periarticular ossification [22].
The indication for an intermediate hip arthroplasty in our context is multifactorial. In the literature, the difficulty of implant selection in femoral neck fractures is not well codified [9,10]. The indication for an intermediate hip arthroplasty is related to patients with reduced mobility [13,14]. This was not the case in our series, where the population was much younger. There was also a high proportion of old fractures (53.25%). The difficulty in our day-today practice lies in the inadequacy of the technical facilities, the aseptic conditions and the accessibility of the intermediate or total arthroplasty. An intermediate prosthesis costs around €1,500 and a total prosthesis around €2,300. This is a huge budget for many families.
This indication for an intermediate hip arthroplasty instead of a total arthroplasty is also linked to this socio-economic level and the availability of the total prosthesis. In this case, the intermediate prosthesis is a better indication than the unipolar prosthesis. Our mean age was 57, whereas many studies were over 68 [9,16,17,2325]. All authors agree that the intermediate hip arthroplasty is not the right indication for femoral neck fractures before the age of 70 [6,23,25-29].
The choice of approach in prosthetic hip surgery remains at the surgeon’s discretion [9,12]. The aim is to achieve early release and, above all, to reduce dislocation [12,30-36]. We used the Moore posterolateral approach in its minimally invasive version in all our patients. There was no significant difference between the posterior and anterior approach in the short term in terms of dislocation and functional results [12,30-36]. The success of the posterior approach lies in the repair of the capsule and reinsertion of the pelvitrochanteric muscles [26,34,36].
In our series before the trauma, 90.91% of patients had total autonomy and 9.09% had partial autonomy. Previous independence is an essential factor in the choice of arthroplasty. At 6 months, all patients had the same Parker score as before the fracture. Infections and thromboembolic complications remain the most serious complications after arthroplasty [6,21,23,37]. We did not observe any infections or thromboembolic complications. Dislocation is the main complication of hip arthroplasty, whether intermediate or total. It may be related to a technical fault or to the approach [12,30-36]. We have recorded 1 case of early dislocation of a prosthesis. Loosening of the prosthesis can be of various origins. They may be septic or aseptic. In our series, we noted 3.08% aseptic loosening, corresponding to rates found in the literature ranging from 0.5% to 8% [31,36]. In our study, there were 18 cases of cotyloiditis. This high rate of cotyloiditis can be explained by the youth and good preoperative autonomy of our series [38,39]. All authors agree that revision surgery seems to be more frequent after an intermediate prosthesis [22,29,38,39]. This trend becomes more pronounced after a postoperative period of more than two years [6]. Wang., et al. [6] explain these results by the appearance of acetabular disease from the 4th postoperative year onwards year onwards. This observation is also made by Boukebous [29], who even recommends dual mobility total prostheses in patients aged over 75. In his opinion, there are more revision surgeries in intermediate prostheses. From a functional point of view, despite a short follow-up, the average PMA score was very good but progressively regressed. All the intermediate arthroplasty performed had excellent or very good short-term results.
The average age was 57, with males predominating. Road traffic accidents accounted for 40.26% of the aetiologies. Fractures were old lesions in 53.25% of cases. The approach was posterior. The rate of cotyloiditis was high. The main complications occurred in patients under the age of 60. Functional results were very good in the medium term.
Copyright: © 2024 Soumaro Kanaté Daouda., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.