Dr Vishnu Vikraman Nair*1, Dr Sarabjeet Kohli2, Nilesh Vishwakarma2, Abhishek Kulkarni3 and Nikil dewnany4
1Fellow In Spine Surgery, Bombay Hospital and Medical Research Centre, Maharashtra, India
2Professor - MGM hospital and medical college, Navi Mumbai
3Senior resident - MGM hospital and medical college, Navi Mumbai
4MBBS Student - K J Somaiya medical college, Mumbai
*Corresponding Author: Dr Vishnu Vikraman Nair, Consultant Spine Surgeon Director - Nair Spine & Knee Clinic, Mumbai.
Received: July 19, 2024; Published: September 20, 2024
Citation: Dr Vikraman Nair., et al. “Improving Surgical Proficiency: A Comparative Study of Single Level Percutaneous Transforaminal Endoscopic Lumbar Discectomy Performed by a Surgeon at Different Stages After Training”. Acta Scientific Orthopaedics 7.10 (2024): 13-19.
Objectives: Undertaking a study which helps to understand the progression and difficulty associated with Percutaneous Transforaminal Endoscopic lumbar discectomy (PETLD).
Methods: The clinical data of 90 patients with single level Lumbar disc prolapse, operated by PETLD by one surgeon with minimum of 1 year follow up data in a Tertiary health care center was retrospectively analyzed. The patients will be divided into 2 groups: Group A – Early operated ( < 45) and Group B – Late operated ( > 45) and their results will be compared by using Surgical time, complications, reoperation rates, Visual analogue score (VAS) and Oswestry disability index (ODI) scores.
Results: The average operational time for Group A was 115.16 ± 11.73 minutes, whereas for Group B it was 112.62 ± 10.72 minutes (p-value > 0.05). The mean duration of hospital stay for Group A was 4 ± 0.81 days, but for Group B it was 3.6 ± 0.78 days (p-value > 0.05). Among the 45 patients in the Early operated group the complication rates were a total of 26.6%. In contrast, the late operated Group B did not exhibit many complications and only had a 2% complication rate. The average postoperative Oswestry Disability Index (ODI) score was 32.11 ± 11.79 in Group A and 27.44 ± 7.43 in Group B, respectively (p-value < 0.05). Similar trends were observed in the comparison of ODI scores at the 1-year follow-up between Group A (32.00 ± 11.89) and Group B (20.56 ± 7.85) (p-value < 0.05). The Visual Analogue Scale (VAS) scores also showed a similar trend like the ODI scores immediately after surgery and at one-year follow-up, with statistically significant difference (p-value < 0.05).
Conclusion: Percutaneous transforaminal endoscopic decompression for lumbar disc prolapse is slowly becoming the gold standard although, our study also shows that the second 45 cases had much better results and fewer complications than the first 45 attributing the difficulties and training required for this surgery.
Keywords: Endoscopic Spine; Transforaminal; Disc Prolapse; Local Anaesthesia
The field of spine surgery, akin to other surgical modalities, persistently undergoes progressive transformation towards lesser invasive procedures. This shift is driven by patient’s inclination towards treatments characterized by diminished morbidity, reduced pain, and expedited recovery, all of which align with their demanding and fast-paced lifestyles. The demand for endoscopic spine surgery in the treatment of spine problems is increasingly prevalent with each successive year. During the 1980s, John McCulloch pioneered the microdiscectomy technique, which involved the utilization of specialized retractor devices in conjunction with an operating microscope. This innovative approach facilitated enhanced visualization by means of a significantly reduced surgical pathway [1]. Following this, Richard Fessler, Kevin Foley, and their colleagues successfully devised a tubular retractor system that continues to be widely regarded as the benchmark for microdiscectomy surgery [2].
Transformational endoscopic discectomy is typically conducted utilizing local anesthesia, resulting in minimal postoperative pain. This procedure aims to preserve normal paraspinal structures and minimize the potential risks of postoperative epidural scar formation and instability. However, it is important to note that this technique is associated with a significant learning curve [3,4].
The objective of this study is to examine the learning curve observed in a solitary surgeon when they initiate the performance of Transforaminal Endoscopic Discectomy procedures for singlelevel lumbar disc prolapse. Additionally, the study aims to compare surgical proficiency and outcomes.
Institutional review board approval from the local ethics committee was taken (Approval number – DHR-EC/2023/03/01). Since the study is retrospective, the requirement of informed consent was waived off by the ethical committee, but still Informed consent was taken from all patients during treatment, and the use of this data for future use in research analysis was explained.
All surgeries were performed by a single surgeon in a single institution who underwent a training fellowship under a trained endoscopic surgeon for 2 months and completed multiple cadaveric courses for the same. Over the course of a 2-month training programme, highly skilled specialists performed 3-4 cases of transforaminal endoscopic spine surgery on a daily basis at 2 hospitals. Despite the shorter duration, the training session was very demanding.
All data related to 90 patients who underwent TLD surgery after the training period from 2018-2021 with a single-level lumbar disc prolapse were retrospectively analysed. These patients were evaluated postoperatively at 24 hours, 3 months, and 1 year using visual analogue scoring (VAS) and Oswestry Disability Index (ODI).
Patients were included in the study if they suffered back pain and combinations of referred pain in buttock, groin, thigh and below the knee which were treated conservatively for at least 3 weeks and on MRI had significant single level prolapse of disc causing compression of the nerve root. Patients were excluded if they were pregnant, had evidenced facet joint cysts, cauda equina syndrome, systemic neuropathy or spinal tumors.
Patients with discitis, canal stenosis, instability and Patients not consenting to undergo surgery.
All surgeries were performed using KARL STORZ 25 degree scope with 3.7mm working channel and 6.3mm outer diameter. and an Operating working sheath, Dilation sleeve, Puncture needle- 1.2mm diameter, guide wire- 0.1mm diameter, Metal mallet, punch sleeve, Grasping forceps and bendable grasping forceps. Prone positioning of the patient on an adjustable radiolucent frame is most desirable for endoscopic transforaminal discectomy. (Figure 1) After prone positioning the level is identified and scrubbing, and painting is done. Markings are done using a scale under C-arm guidance (Figure 2).

Figure 1: Prone positioning.
Figure 2: Level marking.
The skin, subcutaneous tissue, fascia, and muscle layers are infiltrated with local anesthesia of 10ml (Lignocaine 2% (5ml) + Bupivacaine 0.5% (5ml)) at a point of marking done at 10-14 cm lateral from the midline (Figure 3). A lateral entry point is made using the marking as a guide, in a range of 10-14 cm lateral to the posterior midline where the local infiltration was given. Now we use a transforaminal spinal needle to reach the foramen with the needle tip positioned at the medial pedicular line in the anteroposterior projection and on the posterior vertebral borderline in the lateral projection. The needle was then advanced to the midline in the AP projection. (Figure 4) In certain instances, the L5-S1 cases proved challenging to address using the inside-out strategy. Therefore, we opted for a transiliac approach, employing a high-speed burr for these particular patients.
Figure 3: Local anaesthesia infiltration.
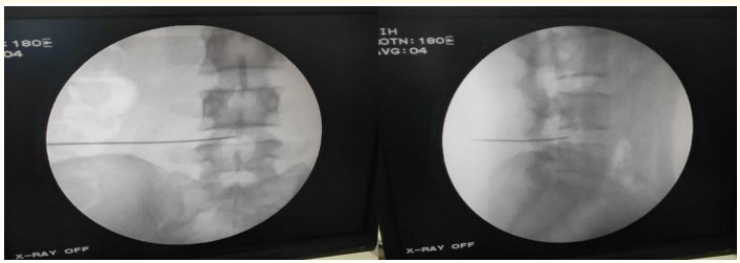
Figure 4: Needle insertion.
We now pass a guide wire after removing the stylet and take the needle out. Skin incision is then taken and serial dilators are used over the guidewire up to the disc space. While passing serial dialators into the disc space, we used sedatives (Inj Propofol) to reduce the patients pain. Once we have reached the desired level the guide wire is removed, and operating sheath is inserted into the disc space. (Figure 5). The dilator is removed, and endoscope is inserted. The disc is directly visualized (Figure 6) and removed. Bleeding is controlled by increasing the pressure of fluid or by bipolar cautery.

Figure 5: Serial dialators on guide wire.
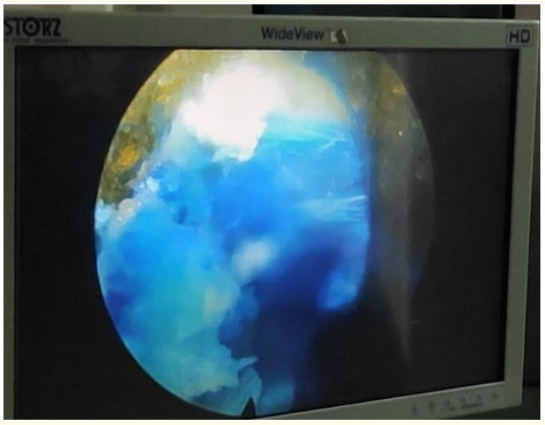
Figure 6: Stained disc material.
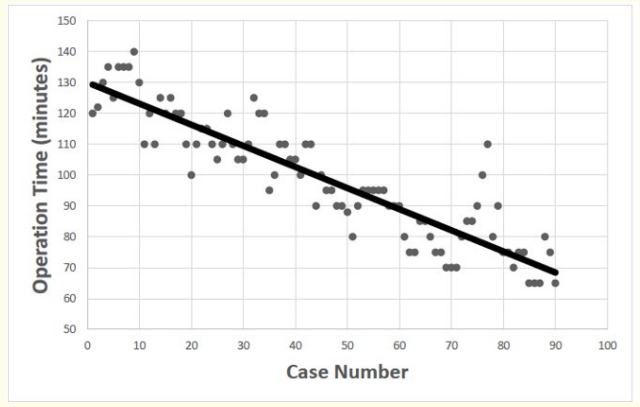
Figure 7: Linear regression analysis-Operation time.
Removal of multiple disc fragments are done and visualization of epidural fat or nerve root and decompression around the root is done with protective measures to not damage the root. Intraoperative relief of leg pain can be seen once adequate decompression is done. After discectomy endoscope is withdrawn and skin incision is closed with a single tag suture.
The data management and statistical analysis were conducted using SPSS version 23.0, developed by SPSS Inc. in Chicago, IL. The statistical tests employed in this study were Pearson’s chi-square test, independent t-test, non-parametric Mann-Whitney U test, one-way analysis of variance, and interrater correlation coefficient test. These tests were selected based on the specific characteristics of the factors being examined. A comprehensive study was conducted, which involved the utilisation of linear regression analysis to examine the learning curve in relation to the duration of operations. The findings are presented as means ± standard deviations or as mean and 95% confidence interval (CI), depending on the distribution of the data. A threshold of p < 0.05 was used to determine statistical significance.
The study cohort comprised 90 patients who were categorized into two groups: Group A, referred to as the “Early” group, and Group B, referred to as the “Late” group. In Group A (Early), there were a total of 45 individuals, consisting of 27 males and 18 females. The mean age of this group was 43.87 years, with a standard deviation of 12.94 years. The age range for this group was between 37 and 77 years. In Group B (Late), there were a total of 45 individuals as well, with 28 males and 17 females. The mean age of this group was 49.24 years, with a standard deviation of 11.53 years. (p-value-0.81). In Group A, there were a total of 7 patients diagnosed with diabetes and 5 patients diagnosed with hypertension. Similarly, in Group B, there were 5 patients with diabetes and 4 patients with hypertension. Additionally, 7 patients in Group A reported alcohol consumption, while 6 patients in Group B reported the same. Furthermore, 6 patients in Group A had a history of smoking, compared to 7 patients in Group B. The average body mass index (BMI) in Group A was 30.93 ± 4.10 kg/ m2, while in Group B it was 30.8 ± 4.04 kg/m2. In Group A, the average length of symptoms to surgery was 8.76 ± 1.8 months, while in Group B, it was 8.87 ± 1.76 months. The distribution of discectomy levels was seen in both groups, encompassing L3-L4, L4-5, and L5-S1. The largest occurrence was found at the L4-5 level in both Group A (60%) and Group B (57.8%). In Group A, 9% of patients exhibited neurodeficit, whereas in Group B, this figure was 7%. The prevalence of paracentral disc protrusion was found to be highest in both Group A, with 71.1%, and Group B, with 68.9%.
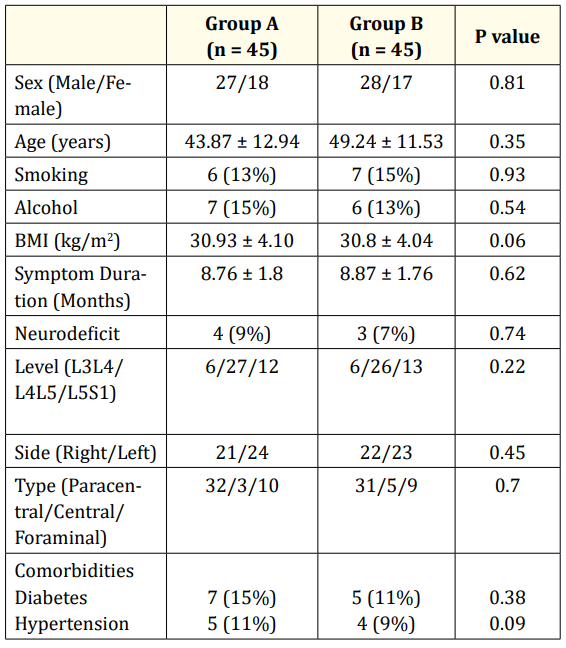
Table 1: Demographics.
The assessment of surgical outcomes was conducted by employing the Visual Analogue Score (VAS) and the Oswestry Disability Index (ODI). The pre-operative Visual Analogue Scale (VAS) scores in Group A (mean ± standard deviation: 7.18 ± 1.13) and Group B (mean ± standard deviation: 7.24 ± 0.91) were found to be similar, with no statistically significant difference (p-value > 0.05). On the first day after surgery, both Group A and Group B saw a notable reduction in VAS scores. Group A had an average score of 4.56 ± 1.20, while Group B had an average score of 3.16 ± 0.99. However, the p-value (> 0.05) indicated that this difference was not statistically significant. Three months after surgery, Group A had a Visual Analogue Scale (VAS) score of 4.11 ± 1.11, while Group B had a VAS score of 2.62 ± 1.12. The p-value was found to be less than 0.05. In the last follow-up, the Visual Analogue Scale (VAS) scores revealed a statistically significant distinction between Group A (3.91 ± .28) and Group B (2.16 ± 1.41), with a p-value less than 0.05. In the analysis of ODI scores throughout the post-operative period, both Group A and Group B exhibited a significant drop in scores. Specifically, Group A demonstrated a mean score of 68.78 ± 14.51, while Group B had a mean score of 58.89 ± 13.61. This difference was found to be statistically significant with a p-value less than 0.05. At the 3-month mark following the surgical procedure, Group A exhibited an Oswestry Disability Index (ODI) score of (32.44 ± 10.26), while Group B shown an ODI score of (20.56 ± 7.85). The p-value was found to be less than 0.05. Similar to the postoperative (ODI) scores, the ODI scores at the final follow-up likewise demonstrated a statistically significant difference between Group A (mean 32.00 ± 11.89) and Group B (mean 20.56 ± 7.85), with a p-value less than 0.05 (Table 2) Operative Time, Blood loss and Hospital stay.
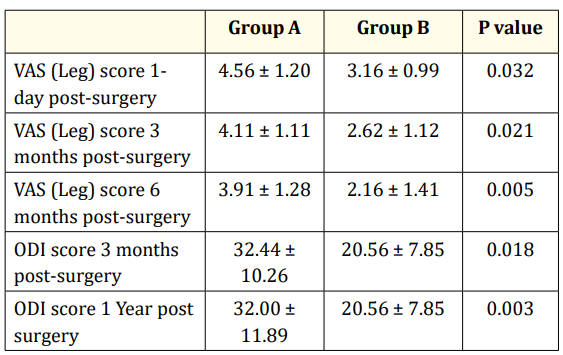
Table 2: Functional Outcome comparison analysis.
When comparing the operative duration between Group A (Early) and Group B (Late), there was a notable disparity observed in the average mean operative time without a statistical significance. Group A exhibited an average operative time of 115 ± 12 minutes, while Group B shown a duration of 82 ± 10 minutes. (p-value > 0.05) The average duration of the surgical procedure exhibited an initial increase for the first 40-45 instances, followed by a subsequent decrease to a lower range after 45 cases. But the operating time did fluctuate to the higher side in a few cases. In this research, we examined the comparison of blood loss between two groups. We found that the late group (Group B) experienced a lower amount of blood loss (81.3 ± 7.57) compared to the early group (Group A) which had a blood loss of 92.3 ± 11.06. However, upon statistical analysis, we did not see any significant difference between the two groups (p-value > 0.05). Comparable trends were observed in the length of postoperative hospitalization, with Group B exhibiting a slightly reduced mean duration of 3.6 ± 0.78 days compared to Group A’s mean duration of 4 ± 0.81 days. However, this difference did not reach statistical significance (p-value > 0.05) between the two groups.
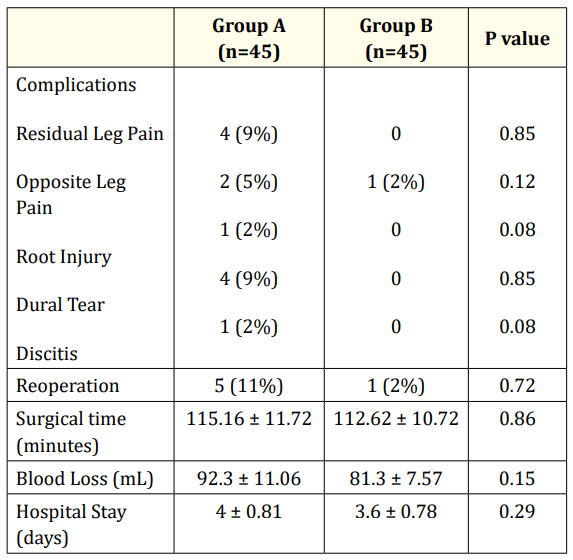
Table 3: Complication comparison.
The early group (Group A) exhibited a notable increase in complication rates as compared to the late group (Group B). Group A exhibited a complication rate of 28.89%, whereas Group B demonstrated a much lower complication rate of 2.22%. (p-value < 0.05) The observed problems in Group A consisted of residual leg pain (8.88%), discitis (2.22%), opposite leg pain (4.44%), and dural tears (6.66%). In contrast, Group B only exhibited a single issue, namely opposite leg discomfort (2.22%). The rate of reoperation within 1 year follow up period was also higher in Group A- 11% in comparision to Group B – 2% (p-value < 0.05). (Table 3).
Percutaneous transforaminal endoscopic discectomy has been proved over the years to become gold standard in treating disc prolapses causing nerve compression. The only dilemma which arises during the innovation of newer techniques is the steep learning curve associated with it which causes many surgeons to take a step back from going into learning these new techniques. The growing awareness among patients regarding endoscopic operations has led to an increased demand for this surgical technique, mostly driven by the desire for improved aesthetic outcomes [5,6]. The concept of endoscopic discectomy was originally introduced as a means of achieving indirect decompression. However, it has since evolved into the concept of targeted fragmentectomy [7]. Using a triangular working zone (kambins triangle) [8] and using a posterolateral approach, all the morbidity and pain related issues associated with traditional open discectomy and microdiscectomy, which involved a part of the lamina to be removed to visualize the disc anteriorly.
The findings of this current study have demonstrated that percutaneous endoscopic lumbar discectomy exhibits a pronounced learning curve, as evidenced by the increased incidence of complications and reoperation rates in Group A (early operated) compared to Group B (late operated), with a statistically significant p-value. Both groups received surgery in an identical setting, where they shared the same operating room, equipment, and surgical instruments, among other comparable factors. The demographic data shown similarities across both groups and did not demonstrate any statistically significant differences. However, when examining the results in terms of the Visual Analogue Score (VAS) and the Oswestry Disability Index (ODI) between Group A and Group B, a notable disparity was observed. Specifically, Group B exhibited considerably superior outcomes throughout the initial postoperative follow-up and the final follow-up. Yeung and Tsou [9] observed a satisfactory success rate of 89.7% in posterolateral disc excision procedures. However, a small proportion of patients (10.3%) experienced poor outcomes, which can be attributed to various complications. These complications included deep infection in two patients, thrombophlebitis in two patients, dysesthesia in six patients, and dural tear in one patient. In another study, Chae et colleagues conducted a total of 153 endoscopic discectomies on patients diagnosed with lumbar disc herniations. The researchers reported a satisfaction rate of 94.77% among the treated individuals [10].
A similar learning curve study done by Lee., et al. during the initial days of endoscopic spine surgery reported 47 out of 51 patients had effective discectomies done, while 4 patients required open decompression later [11].
The literature discusses several consequences, including infections such as discitis, late recurrence, root damage, dysesthesias, dural rupture, vascular injury, and mortality [12,13]. Regarding the overall rates of complications, there was a notable disparity observed between patients in Group A (%) and those in Group B (%). However, when examining the specific complications individually, no significant distinction was found between the two groups. There was no statistically significant difference observed between the two groups in terms of average surgical time, blood loss, and hospital stay.
During this investigation, we have successfully identified and optimized the challenging and critical stages of this technique, which, when executed proficiently, yield the anticipated optimal results. The next step involves the precise positioning of the needle. During the preoperative planning phase, it is crucial to accurately identify the level and location of the disc prolapse. Subsequently, the needle placement should be directed towards the specific site of the disc prolapse. The second consideration is to ensure that the insertion into the intervertebral disc occurs via the kambin’s triangle, while minimizing excessive manipulation, as this could potentially lead to irritation of the dorsal root ganglion. The third requirement involves the performance of a foraminotomy procedure, which is necessary to ensure the lateral liberation of the nerve root. One notable distinction between central and lateral disc herniations is to the variation in needle location. Central disc herniations typically exhibit a preference for a lateral entrance point and a horizontal trajectory, whereas lateral herniations tend to be associated with a more medial entry point and a vertical trajectory.
An additional facet of the process of planning and initiating Transforaminal endoscopic discectomy involves the preoperative assessment and the careful selection of patients. A retrospective analysis was conducted on a cohort of 1586 patients who had undergone percutaneous endoscopic lumbar discectomy (PELD) for the treatment of intracanalicular disc herniations. The findings of this study suggest that open surgery may be a viable option for individuals with herniations characterized by significant canal compromise and high-grade severity [14]. In the initial stages, it is advisable for surgeons to prioritize the performance of surgical procedures on uncomplicated paracentral or lateral disc prolapses at the L4-L5 level, gradually advancing towards managing situations with migrating discs. Several proficient surgeons have expanded their repertoire to include the surgical treatment of extraforaminal and central disc protrusions [15].
In our series, after around 45-50 cases, the surgeon attained a high level of confidence in accurately identifying all anatomical landmarks and acquiring proficiency in the technique of triangulation within the scope. The limitations of this study include its reliance on the personal experience of a sole surgeon, which may not be representative of the broader population of surgeons with varying experiences in spine surgery. The early operated group exhibited a higher incidence of recurring leg pain necessitating a second surgery (11%) compared to the late operated group (2%). This disparity may be attributed to the greater learning curve associated with achieving complete nerve decompression and ensuring thorough discectomy, thereby minimising the risk of any residual loose fragments.
Percutaneous transforaminal endoscopic decompression for lumbar disc prolapse has demonstrated a high level of effectiveness in achieving favorable functional outcomes for patients. This efficacy is comparable to that of typical open or micro lumbar discectomies, while also avoiding the occurrence of postoperative back discomfort. Furthermore, this approach offers the additional advantage of promoting early mobilization, which contributes to increased patient satisfaction. However, our study also demonstrates that while the initial 45 cases yielded satisfactory results, the subsequent 45 cases exhibited significantly improved outcomes and a reduced risk of complications, indicating the presence of a pronounced learning curve associated with this surgery.
Copyright: © 2024 Dr Vikraman Nair., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.