Rayeesa Faheem Syed1*, Rajesh Rachha2 and Srinivas Thati3
1MBBS, MS Orthopaedics, Arthroplasty Fellow, AIG Hospitals, Hyderabad, Telangana, India
2D-Ortho, FEBOT, FRCS (Tr and Orth), Senior consultant, AIG Hospitals, Hyderabad, Telangana, India
3MBBS, MS Orthopaedics, MRCS, FEBOT, FRCS (Tr and Orth), Senior consultant, Director and HOD, Department of Orthopaedics, AIG Hospitals, Hyderabad, Telangana, India
*Corresponding Author: Rayeesa Faheem Syed, MBBS, MS Orthopaedics, Arthroplasty Fellow, AIG Hospitals, Hyderabad, Telangana, India.
Received: June 04, 2024; Published: September 20, 2024
Citation: Rayeesa Faheem Syed., et al. “Chondrofiller and Treatment of Cartilage Defects in the Knee”. Acta Scientific Orthopaedics 7.10 (2024): 03-07.
Background: Focal chondral defects of the knee are common. Several surgical techniques have been proposed for the management of chondral defects. In this study, early functional outcomes with use of ChondroFiller liquid in the knee articular cartilage defects were evaluated.
Methods: A retrospective study of 11 patients who underwent knee arthroscopy and ChondroFiller liquid application for ICRS Grade IV defects were followed up from 6 months to 18 months. Functional outcomes of the patients were evaluated from IKDC subjective evaluation forms.
Results: Mean age of patients was 46.6 years. Isolated chondral lesions were associated with better outcomes (Mean IKDC score 66.25). Chondral lesions are seen in association with other injuries in 63.64% of cases. Chondral lesions over medial femoral condyle are more common (81.8% ) and are associated with better outcomes when compared with lateral tibial plateau lesions. Female patients and high BMI were associated with poorer outcomes.
Conclusion: ChondroFiller liquid could serve as a good treatment option for Grade IV chondral defects in select patients. Future studies on bigger cohort could help in developing an algorithm for patient selection for use of ChondroFiller.
Keywords: ChondroFiller; Cartilage Defects; Knee
CF: ChondroFiller Liquid; MFX: Microfractures; OAT: Osteochondral Autograft Transplantation; ACI: Autologous Chondrocyte Implantation; mACI: Matrix-Induced Autologous Chondrocyte Implantation; ACL: Anterior Cruciate Ligament; ICRS: International Cartilage Repair Society; IKDC: International Knee Documentation Committee Subjective Knee Evaluation
Articular cartilage is a hyaline cartilage and is 2 to 4 mm thick. It is composed of a dense extracellular matrix (ECM) with a sparse distribution of highly specialized cells called chondrocytes. The ECM is principally composed of water, different collagen types with collagen II making up the majority of 90-95% of the ECM, and proteoglycans, with other non-collagenous proteins and glycoproteins present in lesser amounts [1]. Its principal function is to provide a smooth, lubricated surface for articulation and to facilitate the transmission of loads with a low frictional coefficient. Unlike most tissues, articular cartilage does not have blood vessels, nerves, or lymphatics. Once damaged, articular cartilage has a very low regeneration potential due to low cell turnover and a lack of vascularization [2].
Injury or degeneration of the articular cartilage is associated with high morbidity and has an impact on the activity level and quality of life. Historically, the different modalities of treatment available for articular cartilage defects are abrasion chondroplasty, microfracture, mosaicplasty, autologous-chondrocyte implantation (ACI), or matrix-associated chondrocyte implantation (MACI) and osteochondral autograft transplantation (OAT). Although various procedures have been described, the outcomes of the procedures are variable.
With advancements in cell therapy and tissue engineering, hydrogels with material properties comparable to the articular hyaline cartilage serve as an alternative to other modalities of surgical management. In the current study, we focus on the commercially available collagen I-based hydrogel ChondroFiller liquid (Meidirx Biomaterials GmbH, Esslingen Germany), for management of articular cartilage defects.
The aim of the study was to assess early functional outcomes in treatment of articular cartilage defects of knee joint using ChondroFiller.
A retrospective study was conducted on 11 patients who were surgically treated with ChondroFiller for International Cartilage Repair Society (ICRS) grade IV articular cartilage defects (Table 1). Pre-operative and post-operative knee function scores (IKDC scores) were recorded on these patients to evaluate the functional outcomes over 6 months to 18 months interval.
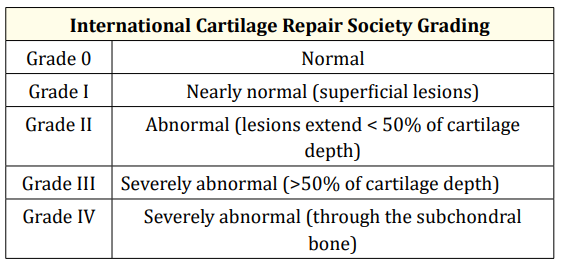
Table 1: International Cartilage Repair Society Grading.
ChondroFiller liquid is a two component collagen gel, which is extracted from rat tail tendons. The collagen type I concentration in ChondroFiller liquid is 8 mg/mL. ChondroFiller liquid is registered as a medical device and is CE certified. The two components of the gel permit a purely arthroscopic application in a prepared cartilage defect. Before using, the implant is stored at -20°C and has to be defrosted up to 37°C in an incubator before implantation [5].
Surgical procedure: All the patients underwent knee arthroscopy surgery with a pneumatic tourniquet. Diagnostic arthroscopy was initially done and underlying associated injuries like meniscal tears and ACL injuries were addressed in the same sitting. Grade I and II chondral lesions were treated with thermal ablation technique. Chondral lesion debridement to a stable margin and application of ChondroFiller liquid was done at the end of other interventions. In few cases with larger defects, microfracture technique was combined with use of ChondroFiller. After addressing the associated injuries, the regular arthroscopic procedure was switched to a dry arthroscopy. Joint maintained dry and Carbon dioxide insufflation was routinely done before the use of ChondroFIller liquid and intra-articular pressure was maintained at 2-3 Pascals. In the arthroscopic view, the collagen gel was filled into the defect by a cannula until the defect was filled completely. Figure 1 and 2 demonstrate the process of use of ChondroFiller liquid to fill the chondral defect with the liquid transforming into a gel-like consistency. The gelification of the implant takes 5-10 minutes and can be estimated by the change of the color (transparent to white). Compression dressing was applied and removed on the 1st post-operative day. Range of movement (ROM) knee brace was used to allow controlled range of movement exercises. Patients were advised non-weight bearing ambulation with 2 elbow crutches or walker frame for 6 weeks.
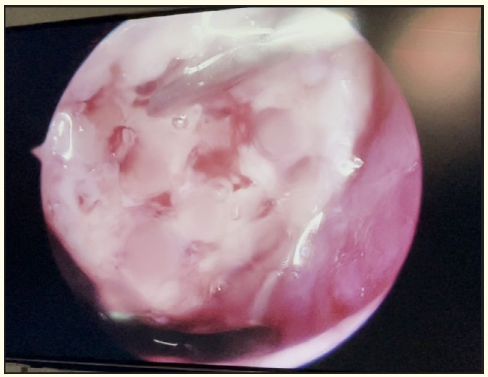
Figure 1
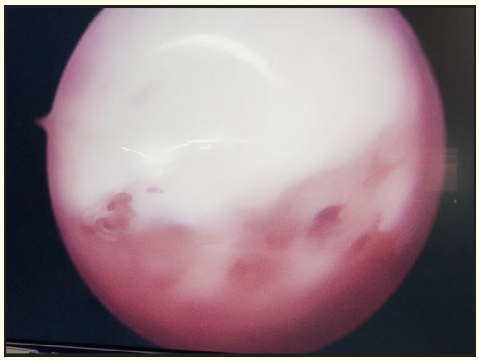
Figure 2
A total of 20 patients who underwent ChondroFiller application for knee cartilage defects from December 2022-2023, were enrolled for the study. 2 patients were acute post-traumatic cases, hence, excluded from study. 7 were lost to follow-up. 11 patients that met the inclusion criteria with focal cartilage defect on MRI images or diagnostic arthroscopy were followed up. Patients with Grade IV osteoarthritis, inflammatory arthritis, >1/3 meniscal excision, acute post traumatic articular cartilage defects were excluded from the study. Informed consent was taken from all patients prior to the study. Ethics committee approval was taken before the commencement of the study.
The average age of the patients in the study group was 46.63 years (27-66 years) (Figure 3). Gender distribution was 5 male and 6 female patients (Figure 4). Mean chondral defect size as confirmed on diagnostic arthroscopy, was of size 11.82mm-17.82mm. Pre-op scores ranged from 5-29 as per IKDC functional knee scoring (Mean pre-op score: 17.55) and post op scores ranged between 31-82 (Mean post-operative score 56.45). Patients younger than 35 years showed better improvement with the procedure. The average preop scores in these patients were 31, and post op scores improved to 81.5. Male patients reported better post-operative functional outcomes than female patients (Mean post-operative scores in males was 72.2 and 34.5 in female patients). Patients with isolated chondral injury (4 patients) had better post-operative scores (Mean post op scores of 66.25) than patients who had associated injuries in the knee. ACL reconstruction was done in 2 patients (Mean post op score 53). Medial meniscal root repair was performed in 2 patients (Mean post op score of 35). Partial meniscal excision was done in 3 patients (Mean post op score of 60) (Figure 5). Patients who had isolated chondral defect over medial femoral chondyle reported better results in the post-operative period than patients who had involvement of lateral tibial plateau. Patients with higher BMI reported poorer functional scores.
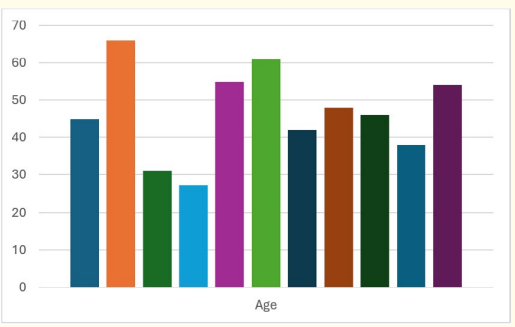
Figure 3: Age distribution.
Figure 4: Gender distribution.
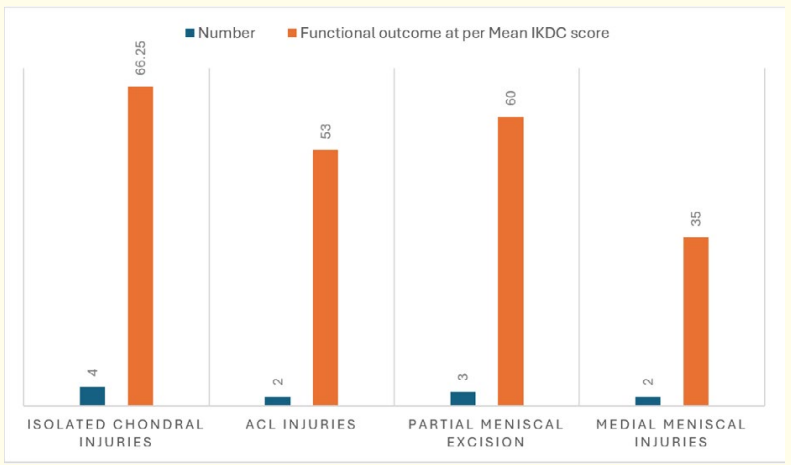
Figure 5: Associated injuries.
Articular cartilage is a highly specialized connective tissue of diarthrodial joints. Its principal function is to provide a smooth, lubricated surface for articulation and to facilitate the transmission of loads with a low frictional coefficient. The mechanical behavior of this tissue depends on the interaction of its fluid and solid components. The unique and complex structure of articular cartilage continues to make its treatment and repair a significant challenge [1].
The collagen type I in ChondroFiller liquid is obtained by acid extraction from rat tail tendons. In clinical practice, ChondroFiller liquid is directly injected into the cartilage defect (Outerbridge grade III-IV) and forms a pressure-resistant gel to fill the defect. It acts as a scaffold and provides the cells with a matrix into which they can migrate [2].
While the incidence of articular cartilage injuries varies between 61% to 63% in knee arthroscopies, as per previous studies, cases of single, well-defined ICRS grade III or IV chondral or osteochondral defects of at least 1 cm2 in patients younger than 40, 45, or 50 years were found in 5.3%, 6.1%, and 7.1% of all arthroscopies, respectively, or 10.0%, 9.1%, and 9.2% of the arthroscopies in the respective age groups, as per a study conducted by Hjelle., et al. [3]. In another large retrospective study involving 136 surgeons, Curl., et al. [4]. found Outerbridge grade IV lesions were documented in 20% of all arthroscopies, but the majority (72%) were found in patients over 40 years of age. Patients under 40 years showing documented grade IV lesions accounted for 5% of all cases.
The average age of the patients with chondral lesions on knee arthroscopy was 43 years (range, 1 to 92 years); more male than female patients had chondral lesions (61.6% v 38.4%, respectively) in a study on 31,516 knee arthroscopies by Curl., et al. [4]. The mean age in our study was 46.63 years. In a study by Schneider U.5 the mean age was 47.2 years in the ChondroFiller group.
Associated knee injuries with chondral injuries like ACL tear or meniscal injuries and their effect on the functional outcomes after treatment with ChondroFiller was excluded by the study conducted by Schneider U [5]. In the study conducted by Hjelle., et al. [3], in cases of focal chondral or osteochondral defects, a concomitant meniscal or anterior cruciate ligament injury was found in 42% (n = 81) and 26% (n = 50), in arthroscopy on 1000 knee joints. Concomitant injury of both meniscus and anterior cruciate ligament injury was found in 12% (n = 23). In our study, we noted that isolated chondral injuries were present in 4 patients (36.36%). Concomitant ACL injuries were treated in 2 patients (18.18%) and medial meniscal root repair was done in 2 patients (18.18%). Partial meniscal excision was performed in 4 patients (Lateral meniscus in 2/11 (one of them also had ACL reconstruction and hence, included in ACL reconstruction category), Medial meniscal root tear debridement in 1 and medial meniscal partial excision in 1).
Medial femoral condyle articular cartilage defect was seen to be most common area of chondral defect in all the previous studies [3-5].
Previous studies of use of ChondroFiller liquid in hip arthroscopies for femoro-acetabular impingement syndrome, provided good to excellent outcomes in a study conducted by Mazek., et al. [6]. on 26 patients.
In current literature, there are not many studies on use of ChondroFiller liquid in knee joint. In one of the studies conducted on knee joint, for use of ChondroFiller, the mean IKDC patient values in the CF-group showed a significant increase of up to 72.1 (+/-13.2) after six months from a preoperative mean score of 43.3 (+/-10.4) in a study conducted by Schneider U [5]. on 13 patients treated with ChondroFiller liquid. In our study, the mean preoperative IKDC scores were 17.54 and mean post-operative IKDC scores improved to 56.45.
In the current study, younger patients (<35 years), with isolated articular cartilage defects and defects over the medial femoral condyle showed better results with use of ChondroFiller liquid. Male patients and patients with BMI <25 reported improved functional outcomes.
One limitation of the study was the small sample size. The study was conducted in a retrospective manner. MRI scans could not be performed on the patients in the post-operative period for radiological assessment of healing or progression of the lesions to correlate with the functionality.
Prospective studies with bigger cohort and longer post-operative follow up period would provide as a guide for management of difficult chondral lesions.
None.
Copyright: © 2024 Rayeesa Faheem Syed., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.