David Gouveia*, João Martins, Pedro Ribeiro, Miguel Relvas, Joana Freitas, André Pinho, Vitorino Veludo and António Sousa
Department of Orthopedics and Traumatology of Unidade Local de Saude São João, Porto, Portugal
*Corresponding Author: David Gouveia, Department of Orthopedics and Traumatology of Unidade Local de Saude São João, Porto, Portugal.
Received: July 24, 2024; Published: August 29, 2024
Citation: David Gouveia., et al. “Grisel’s Syndrome in a Child-A Case Report”. Acta Scientific Orthopaedics 7.9 (2024): 37-40.
Grisel’s syndrome consists of atraumatic subluxation of the atlantoaxial joint without associated history of trauma. Initial pharyngeal inflammation spreads to the prevertebral fascia through contact with the peri-odontoid venous plexus and pharyngovertebral veins, inducing fasciitis, abnormal relaxation of the atlantoaxial ligaments, reactionary muscle contraction, and subsequent ankylosis. Medical treatment with NSAIDs, muscle relaxants, and cervical immobilization is generally sufficient; however, cervical traction may be necessary. Surgical treatment with C1-C2 arthrodesis is indicated in cases of conservative treatment failure or the appearance of neurological signs/symptoms. Close collaboration between pediatricians, otolaryngologists, and pediatric orthopedic or spine surgeon is essential for early diagnosis and treatment, which is the main prognostic factor for the success of medical treatment, avoiding surgery.
Keywords: Grisel’s Syndrome; Atlantoaxial Subluxation; Juvenile Torticollis
GS: Grisel’s Syndrome
Grisel’s syndrome (GS) is defined as atraumatic rotatory subluxation of the atlantoaxial joint, generally associated with infections or surgeries of the head and neck [1-3].
It is a rare condition, mainly observed in children [3].
The high incidence of cases in children is likely linked to a combination of several factors: greater ligamentous laxity, C1C2 hypermobility, cervical muscle weakness, immature bone formation, and a higher rate of upper respiratory tract infections [4,5].
The diagnosis is based on clinical and radiological findings. GS should be considered in patients presenting with painful torticollis, fever, absence of trauma, and a history of infection/surgery of the head and neck [1-3]. Plain radiographs and computed tomography (CT) of the cervical spine are necessary to confirm the diagnosis and classify it according to the Fielding-Hawkins grading system (Table 1) [6]. Magnetic resonance imaging (MRI) is crucial to assess the spinal cord when neurological signs and symptoms are present and can provide useful information about the condition of the surrounding soft tissues [7].
There is no standard treatment, although there is a consensus on progressively more invasive treatment according to the Fielding-Hawkins grade and the delay in diagnosis [1-3]. Types I and II often present without neurological deficits and are generally treated conservatively with nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, physical therapy, and a cervical collar. Types III and IV are more severe, generally associated with neurological deficits, and are mainly treated surgically [1-3,6].
Surgical options are varied and minimally described in the literature [8].
Therefore, the aim of this work is to report a case of GS in a child undergoing C1-C2 arthrodesis after conservative treatment failure and discuss the various existing treatment options.
We present the case of a 10-year-old girl from a rural area with a medium socioeconomic background, who presented to our hospital with a two-week history of torticollis, without any preceding trauma.
The child had a history of recurrent pharyngitis, usually treated with oral antibiotics and NSAIDs.
After a new episode of pharyngitis, which resolved with medical treatment, she developed cervical pain, restricted neck movements, and irreducible torticollis.
On physical examination, 2 weeks after the onset of symptoms, she presented with fixed left-sided cephalic rotation, head tilt > 20°, without neurological changes (Figure 1).

Figure 1: Two weeks after the onset of symptoms, fixed left-sided cephalic rotation and head tilt > 20°.
CT of the cervical spine revealed left-sided atlantoaxial rotatory subluxation without ligament injury, confirmed by MRI (Figure 2). The time to diagnosis of GS was 3 weeks.
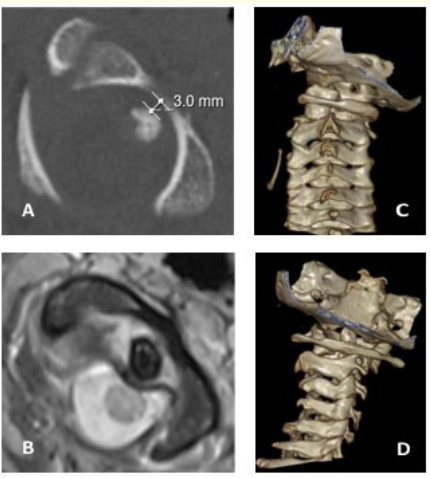
Figure 2: Ten-year-old girl with persistent torticollis for 2 weeks. A: Cervical CT showing 3 mm anterior displacement of C1 (Fielding-Hawkins type III). B: Cervical MRI T2-weighted showing ligamentous rupture. C and D: Preoperative rotation of 20° in 3D reconstructions.
Cervical traction was adjusted under general anesthesia with Gardner-Wells tongs and closed reduction under radiological control was initially attempted. Traction was started with 5% of body weight and increased to 15% after 48 hours (Figure 3). Bed rest traction was maintained, associated with NSAIDs and muscle relaxants for 7 days.

Figure 3: A: Cervical traction adjusted under general anesthesia and closed reduction. B: Initially radiological control showed no loss of reduction or consequent subluxation.
Reassessment CT showed loss of reduction and consequent subluxation. Due to the lack of clinical and radiological improvement, surgical treatment with open reduction and posterior C1-C2 arthrodesis using a modified Gallie technique was necessary.
Under general anesthesia, the child was placed in the prone position with head fixation in a neutral position after mild cephalic traction. A posterior approach was performed, and the posterior elements of C1 and C2 were exposed subperiosteally. Under microscopic control, the articular facets were exposed bilaterally. Facet reduction was performed under fluoroscopy. A metal wire was placed under the posterior arch of C1, looping around the C2 spinous process, followed by the placement of an autologous iliac crest bone graft with a notch in the midline to fit between the C1 posterior arch and the C2 lamina/spinous process. There were no intraoperative or postoperative complications.
After 2 years of follow-up, the child is asymptomatic with normal cervico-cephalic alignment and successful arthrodesis (Figure 4).
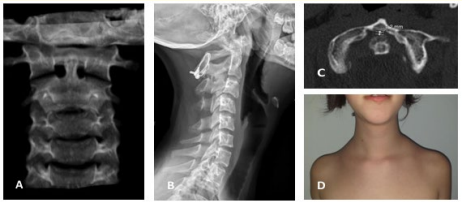
Figure 4: At 2 years of follow-up. A and D: Normal cervico-cephalic alignment. B: Achieved arthrodesis. C: Cervical CT showing no anterior displacement of C1 (distance 1.2 mm).
GS is a type of atraumatic subluxation of the atlantoaxial joint without associated ligament injury. Anatomical studies have demonstrated the existence of a peri-odontoid vascular plexus that drains the posterior-superior region of the pharynx [9]. GS may result from this relationship between the peri-odontoid vascular plexus and the pharyngo-vertebral veins. Pharyngeal inflammation/infection spreads through these plexuses to the prevertebral fascia, inducing fasciitis, abnormal relaxation of the atlantoaxial ligaments, reactional muscle contraction, and subsequent ankylosis [6]. This hypertonia of the neck extensor muscles leads to progressive rotatory subluxation of the C1-C2 joint [8].
Given the nonspecific symptoms, the diagnosis is based not only on the clinical context but also on radiological findings, with cervical CT being crucial [7]. Late diagnosis increases the risk of neurological complications, and MRI can complement and reveal abnormalities in soft tissues and neurological structures, such as laxity of the transverse and alar ligaments [7,10]. Radiological evaluation helps rule out differential diagnoses of traumatic or neurological etiology (with expansive processes of the posterior fossa). After radiological evaluation, atlas deviation relative to the odontoid process can be classified using the Fielding-Hawkins grading system (Table 1) [6].
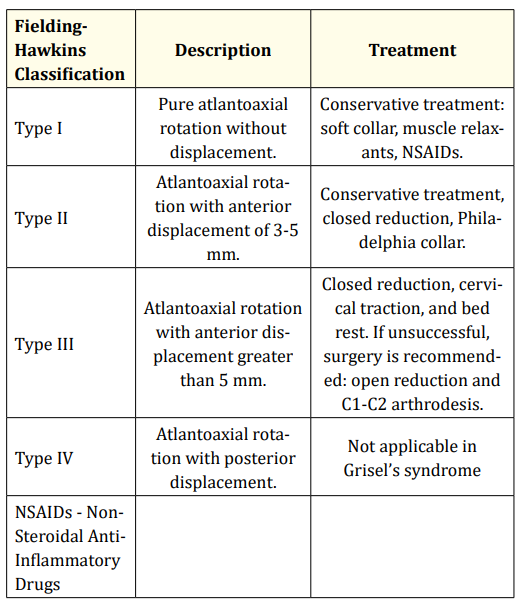
Table 1: Treatment strategy according to the Fielding-Hawkins classification in Grisel’s syndrome.
Currently, there is no standard treatment for GS [1]. In most cases, medical treatment is sufficient, although cervical traction may be necessary [8]. Some authors have reported good results with long-term Halo traction, with surgery being indicated as a last resort [11].
The Fielding-Hawkins classification is commonly used in the literature to guide therapeutic strategy in GS [2,6,8,11]. Fielding and Hawkins [6] described a classification system to estimate the severity of atlantoaxial joint rotatory subluxation on CT in traumatic injuries. The degree of subluxation and instability increases with the type. Types I and II are not associated with neurological injury. Type III has an incidence of 15%. Type IV refers to fixed rotation with posterior displacement and does not seem to describe the subluxations found in GS [12]. Kraft and Tschopp [13] described type 0, consisting of persistent torticollis without radiological evidence of subluxation.
For each type, regular clinical follow-up is necessary to identify possible symptom progression. Similarly, rapid radiological reassessment is essential.
Table 1 summarizes our treatment protocol. First-line treatment in cases without neurological injury is conservative. In type I, the use of NSAIDs, muscle relaxants, and immobilization with a soft collar seems sufficient. Reduction and immobilization with a rigid cervical collar are recommended for type II. Type III requires cervical traction and bed rest.
The success of reduction after cervical traction seems to depend on the duration of previous symptoms [11,12]. Arthrodesis is indicated only in case of failure of conservative treatment or firstline in case of neurological deficits [11,12,14].
In the described case (Fielding-Hawkins type 3 subluxation), reduction was not maintained after medical treatment and cervical traction for 7 days. The child then underwent surgical treatment.
When surgery is necessary, C1-C2 arthrodesis with wires or screws is an option [14]. In patients with atlantoaxial instability without associated bone or ligament injury, the Gallie technique can be chosen as a safe and effective method if preoperative reduction can be achieved [15]. Compared to screw arthrodesis, the Gallie technique offers shorter convalescence, less pain, shorter surgical time, less intraoperative blood loss, less radiation exposure, lower hospital costs, and similar fusion rates [15]. In cases of late diagnosis, surgical treatment is usually necessary [10-12].
The diagnosis of GS should be considered in children with cervical pain, persistent torticollis, particularly after head and neck surgery/infection. Diagnosis requires close collaboration between pediatricians, otorhinolaryngologists, and orthopedists. Early diagnosis, adequate clinical and radiological evaluation (with cervical CT), avoids neurological complications and increases the likelihood of cure without the need for surgical treatment.
Copyright: © 2024 David Gouveia., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.