Manuel Becerra1, Enrique Cifuentes1,2, Carolina Becerra3, Héctor Foncea1*, Chu-Long Yuan Lu1, Nicolás Rojas1,2, Ivan Radovic1,2, Leonardo Villarroel1
1Orthopedic Surgeon, Hip Unit, Instituto Traumatológico Dr. Teodoro Gebauer Weisser, Chile
2Orthopedic Surgeon, Hip Unit, Clínica Red Salud, Chile
3M.D., University of Valparaíso, Chile
*Corresponding Author: Héctor Foncea, Orthopedic Surgeon, Hip Unit, Instituto Traumatológico Dr. Teodoro Gebauer Weisser, Chile.
Received: July 29, 2024 ; Published: August 26, 2024
Citation: Héctor Foncea., et al. “Outcomes of Dual Mobility Total Hip Arthroplasty. Descriptive Analysis”. Acta Scientific Orthopaedics 7.9 (2024): 21-27.
Introduction: Instability is one of the most frequent complications in total hip arthroplasty (THA). To reduce the risk, prosthetic models such as the dual mobility system (DM) have been designed.
Objective: To perform a descriptive analysis of the results of THA with a DM component.
Materials and methods: A retrospective study was carried out by collecting data from patients operated on for THA between 2016 and 2019 in two centers: a public sector traumatology hospital and a private care hospital in the central area of Chile. Inclusion criteria were patients of all ages who underwent DM-THA surgery due to primary osteoarthritis, femoral neck fracture or revision surgery. Patients with septic loosening, incomplete data, and with less than 6 months of follow-up were excluded. Demographic, clinical and radiographic data were obtained from clinical record. Subsequently, measurements of global offset, acetabular inclination and limbs length were carried out and the results were analyzed using statistical models, hypothesis tests and logistic regression model.
Results: Out of a total of 1241 records evaluated, 78 patients met inclusion and exclusion criteria. 70.5% were women and 29.5% men. Mean age was 73.5 years (SD = 13.7), with an average BMI of 25.8 (SD = 4.8). The cause of indication for DM-THA was 64% due to femoral neck fracture, 24% degenerative pathology, 9% revision surgery and 3% others. Percentages of arterial hypertension, type 2 diabetes mellitus, and neurological diseases were 41%, 14%, and 16%, respectively. There were 5 (6.5%) episodes of dislocation, 3 of which were conventional and 2 intraprosthetic. Radiographic study showed an average acetabular inclination of 39º, an average global offset of 4 mm less than the contralateral and a 2.6 mm higher discrepancy in the operated limb. There was no significant association between dislocation and cause of indication of THA, age, BMI, measurement of the prosthetic head, gender, alcohol consumption, neurological diseases, spinal pathology, ASA, number of previous surgeries, approach or intraoperative complications. The survival of patients from surgery at 1 year and 3 years was 91.76%, falling to 56.7% at 5 years.
Conclusions: Rate of dislocation of DM-THA is higher than that reported in the literature in our sample of the Chilean population. Future studies should identify other factors that explain these findings.
Keywords: Dual-Mobility; Arthroplasty; Hip; Descriptive Analysis
Total hip arthroplasty (THA) is one of the most common and successful orthopedic procedures, however, instability is a complication present in all series, being the second reason for revision at any time and the first cause of early reoperation [1-4]. Reported dislocation rates range from 0.2% to 7% after primary procedures and up to 21% in a second intervention [5-7]. To address this problem, different designs have been developed, such as constricted prostheses, larger diameter heads and the double mobility system (DM) [8,9].
Concept of DM was introduced by Bousquet and Rembert in France in 1974 and has become globally popular due to its ability to provide greater joint stability [10]. This design includes two movable joints, one between the prosthetic head and the insert and other between the insert and the cup. The double joint point allows a greater range of motion without impingement and allows a higher head-to-neck ratio, resulting in a longer jump distance and a lower likelihood of dislocation. In addition, it manages to combine Charnley’s low-friction principles with Mckee-Farrar concepts of larger femoral heads to improve stability [11,12].
Although some studies have published that DM design could add potential drawbacks such as greater wear of acetabular polyethylene, higher incidence of aseptic loosening and higher risk of infection [13-16], it has been seen that with the new generations of DM and polyethylene these complications have decreased [17,18]. In any case, the higher cost of the implant and the risk of intraprosthetic dislocation (Figure 1) make it necessary to have studies that show a real benefit of its indication.
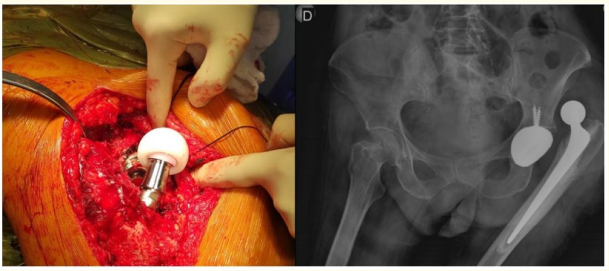
Figure 1: Intraprosthetic dislocation of dual mobility total hip arthroplasty. Left: clinical image. It is observed how the liner remains attached to the femoral head. Right: AP pelvic x-ray showing dislocation of left hip prosthesis. Above the dislocated prosthetic head there is a shadow that could correspond to the PE liner fixed to prosthetic head.
The objective of this study is to perform a descriptive analysis of the results of DM-THA in a sample of Chilean population.
Our work corresponds to a retrospective study by collecting data from a sample of patients undergoing THA between 2016 and 2019 in two centers: a public sector traumatology hospital and a private care hospital in the central area of Chile. Patients of all ages who underwent DM-THA surgery due to primary osteoarthritis, femoral neck fracture or revision surgery were included. Patients with septic loosening, tumoral fracture, incomplete data, and with less than 6 months of follow-up were excluded. Demographic data (age, sex), morbid history, height, weight, surgical technique, implants and complications were obtained from the clinical record. Postoperative radiographs were analyzed and two specialists with more than 20 years of experience performed global offset, acetabular tilt and limb length measurements.
The results were studied using classic exploratory analysis, hypothesis test (Chi-square, Mann Whitney test) and logistic regression model.
Between 2016 and 2019, 1241 patients undergoing THA were identified. Of these, 78 patients met the inclusion and exclusion criteria. 70.5% were women and 29.5% men. The mean age was 73.5 years (SD = 13.7), being very similar in men and women (74.6 vs. 73.0 years, respectively). Figure 2 shows age groups and dispersion. The groups with the highest number of participants were between 70-79 and 80-89 years old. The mean BMI was 25.8 (SD = 4.8).
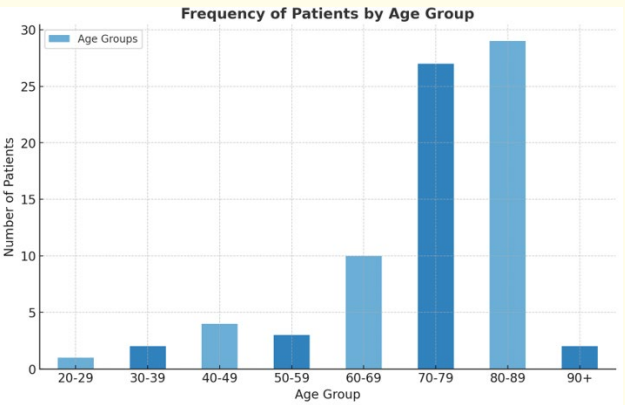
Figure 2: Frequency of patients by age group. This figure displays the distribution of patients across different age groups. Histogram shows the number of patients in each age range. The majority of patients were found within the 70-79 and 80-89 age groups.
Percentages of arterial hypertension, type 2 diabetes mellitus, and neurological diseases were 41%, 14%, and 16%, respectively.
The cause of indication for DM-THA was in 64% of cases due to femoral neck fracture, 24% due to degenerative pathology (primary or secondary osteoarthritis), 9% due to revision surgery and 3% others. Indications for revision included instability (N = 4), periprosthetic infection (N = 1), and aseptic loosening (N = 2).
Preferred approach was posterior (91%) followed by lateral (9%). We did not find any intraoperative complications related to acetabulum and those that did occur, were 3 type A femoral fractures (Vancouver classification), all of which were successfully managed. Regarding postoperative complications, 5 episodes of dislocation were recorded, which corresponds to 6.5% of the cases, 3 of which were conventional and 2 intraprosthetic (Table 1). Risk factors identified in this subgroup of patients were revision DMTHA, obesity, ASA 3 and history of stroke. There was only one case of infection.
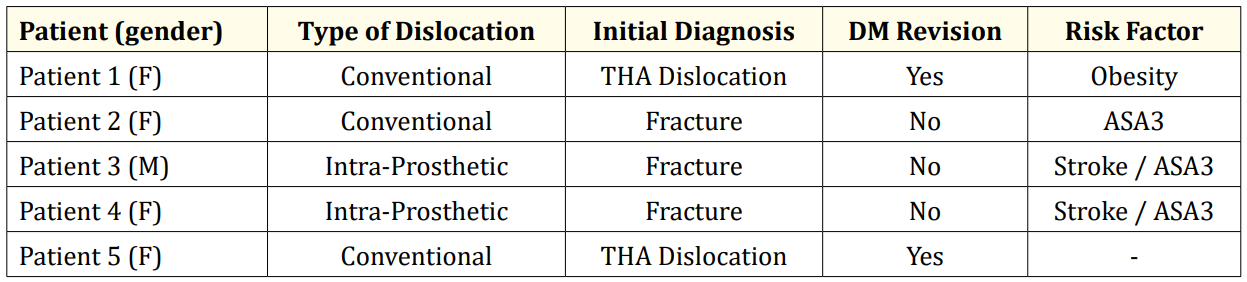
Table 1: Characterization and Identification of Risk Factors in Dislocated Patients in Our Series. F: female, M: male. THA: Total hip arthroplasty. The two cases of dislocation were due to instability of a primary THA.
Radiographic study showed average acetabular inclination of 39º in dislocated patients, average global offset of 4 mm less than the contralateral hip, and a discrepancy of 2.6 mm higher in operated limb (Table 2).
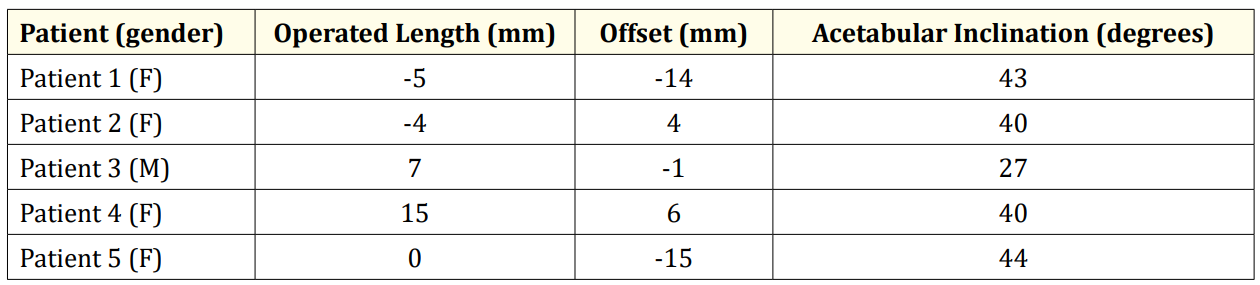
Table 2: Radiographic Analysis of Dislocated Dual Mobility Total Hip Arthroplasty. The reference for length and offset is in relation to the contralateral limb.
Statistical analysis obtained that age (p = 0.419), BMI (p = 0.411), head size (p = 0.317), head length (p = 0.217), gender (p = 0.979), alcohol consumption (p = 0.617), neurological disease (p = 0.761), spinal pathology (p = 0.466), ASA (p = 0.165), indication of DM-THA (p = 0.285), preoperative diagnosis (p = 0.632), number of previous surgeries (p = 0.975), type of approach (p = 0.934) and intraoperative complications (p = 0.610) were not related to dislocation episodes.
A logistic regression model was performed to evaluate the strength and direction of the associations between some of the variables studied. All associations were non-significant, with a 95% confidence interval (Table 3).
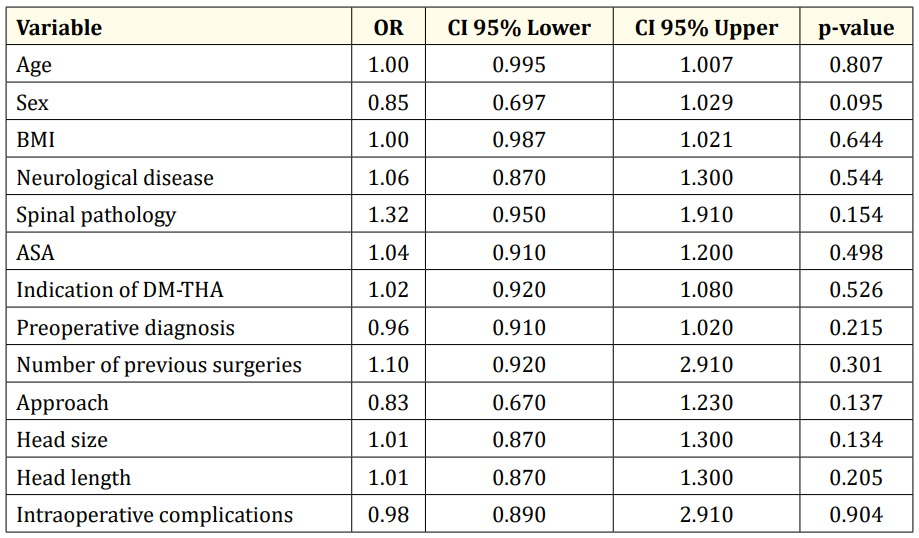
Table 3: Summary of odds ratios for selected Variables. This table summarizes the odds ratios (OR) with 95% confidence intervals (CI) and p-values for various variables analyzed in a logistic regression model, including age, sex, BMI, neurological disease, spinal pathology, ASA, THA-DM indication, preoperative diagnosis, number of previous surgeries, surgical approach, head size, head length, and intraoperative complications.
Overall survival of patients from surgery at 1 and 3 years was 91.76%, falling to 56.7% at 5 years.
Instability continues to be a problem in primary, fracture and revision arthroplasties. In response, DM components have emerged, designed to allow a greater range of motion and a greater head-to-neck ratio, reducing the probability of dislocation. Our study performed a descriptive analysis of the results of a sample of patients operated on with DM-THA in Chilean population
Average age of operated patients was 73 years, with a greater representation of the 70-79 and 80-89 age groups. We concentrated most of the indications in elderly patients, which is supported by the literature where it has been seen that DM cups reduce the risk of dislocation and revision, being a measure that improves the cost-effectiveness of the treatment [19,20]. In this age range, DM cups have even presented better functional results than hemiarthroplasties in fractures, with no disadvantages in mortality, loosening or dislocation rates [21]. On the other hand, our age dispersion was high and despite the average, we had 8 patients under 50 years of age. With the new DM models, wear is not always a priority concern, as some studies have shown excellent component survival with minimal corrosion and metal ion release in young, active patients [22]. Other studies have shown adverse results and, for example, Nam D., et al, found increased cobalt levels in 4 of 26 young patients followed after DM-THA [23]. It will be necessary to wait for more studies to support this indication in younger patients.
16% (N = 19) of our patients had some neurological disease. Of these, the majority had their indication for DM-THA due to fracture (N = 17). Diagnoses in this group were sequelae stroke (N = 8), Parkinson’s disease (N = 6), Alzheimer’s disease (N = 2), epilepsy (N = 2), and sequelae brain tumor (N = 1). In our center, based on the new evidence, we have been privileging the use of DM in this type of patient. Cnudde, P., et al. studied 9,638 patients with neurological diseases who underwent unilateral arthroplasty for femoral neck fracture and found that the rates of dislocations were similar between hemiarthroplasty and DM-THA, proposing DM as a safe and better option than conventional arthroplasty [24]. El-Deeb, M., et al. found that DM cups could prevent early dislocation in patients with neuromuscular diseases or cognitive dysfunction [25]. Liang,C., et al, concluded that DM system significantly improves quality of life in elderly patients with femoral neck fracture and severe lower limb dysfunction as a consequence of a stroke [26]. Lazennec, J., et al., on the other hand, studied 59 patients with Parkinson’s disease undergoing to DM-THA and described good to excellent results at 2 years of follow-up [27]. It is noteworthy that, like in our study, this last group presented intraprosthetic dislocation. This could be interesting to analyze in future studies, given the rarity of this condition.
There were 5 episodes of dislocation (6.5%). 2 of these cases were after revision surgery (2.5%) and 3 after primary arthroplasty (3.8%). This is higher than what has been found in the literature, where it has been shown that the percentage of primary dislocation is 0.6-0.9% and in the case of post-revision dislocation, 2.2-3.0% [28,29]. We did not find factors that could explain this result, so it would be interesting to analyze biomechanics of the implant in Chilean population, considering the great variability of the anatomy according to ethnicities. For example, femoral offset measured in United States is 42.2 mm (SD 5.1), while in India lower values have been observed, being 35.6 mm for men and 32.9 mm for women [30]. It is important to emphasize that DM prostheses should not be considered as compensation for poor surgical technique (poor acetabular orientation or inadequate restoration of soft tissue tension) and should always seek to achieve the objectives of surgical planning. Characterization of dislocated patients is shown in table 1, where we indicate the risk factors identified in the literature present in our patients [31].
Radiographic study (Table 2) showed an average acetabular inclination of 39º in dislocated hips, which would not explain the increased risk, except perhaps in the case with an inclination of 29º [32]. On the other hand, 2 cases were found that presented a much lower global offset compared to the contralateral (-14 and -15 mm). The literature reports that a decreased offset value of 5 mm or more is related to worse functional and quality of life outcomes [33]. Radiographic discrepancy was 2.6 mm in favor of the operated limb, which is within an acceptable surgical result and, on the contrary, is a protective factor against dislocation [34].
3 dislocated THAs were conventional (3.8%) and 2 were intraprosthetic (2.5%). Intraprosthetic dislocation is a rare and specific complication of prostheses with a DM component, its incidence reported in the literature is less than 0.3% [35]. Philippot, R., et al. classified them as Type 1: no arthrofibrosis and no cup loss; Type 2: secondary to liner blockage and Type 3: associated with cup loss [36]. In X-ray as seen in Figure 1, you can see the “bubble sign” that corresponds to the image of luxated polyethylene liner. One of the explanations for this type of dislocation is the “bottleopener effect”, where the polyethylene liner is trapped in the metal edge of the cup or in some bony prominence during the closed reduction maneuver [37]. However, in our series both cases were diagnosed without prior intervention, so we believe it is necessary to continue with similar studies that can clarify this result.
Overall survival of patients from surgery at 1 and 3 years was 91.76%, falling to 56.7% at 5 years, which could be discussed in future studies that evaluate differences with other types of implants.
In our sample of Chilean population, rate of dislocation of DM-THA is higher than that reported in the literature. Although all dislocated patients had at least one clinical or radiographic risk factor predictor of dislocation, we were unable to identify a significant association, so we believe it is necessary to formulate new studies to explain these results.
Copyright: © 2024 Héctor Foncea., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.