David Gouveia*, Diogo Tomaz, Marco Bernardes, João Correia and Jorge Mendes
Department of Orthopedics and Traumatology of Unidade Local de Saude Tâmega e Sousa, Penafiel, Portugal
*Corresponding Author: David Gouveia, Department of Orthopedics and Traumatology of Unidade Local de Saude Tâmega e Sousa, Penafiel, Portugal.
Received: July 24, 2024; Published: August 20, 2024
Citation: David Gouveia., et al. “Liposclerosing Myxofibrous Tumor of Proximal Femur Treated with Intramedullary Nail Fixation a Case Report”. Acta Scientific Orthopaedics 7.9 (2024): 15-18.
Liposclerosing myxofibrous tumor is a rare benign bone tumor predominantly affecting the proximal femur. It typically presents in middle-aged adults and can be mistaken for various other bone lesions. Malignant transformation, though rare, has been reported.
We report the case of a 60-year-old female with a geographic lesion in the proximal femur. Biopsy confirmed the diagnosis of Liposclerosing myxofibrous tumor. Surgical intervention included curettage, artificial bone matrix implantation, and intramedullary nail fixation.
Liposclerosing myxofibrous tumor should be considered in the differential diagnosis of heterogeneous lytic lesions in the proximal femur. Comprehensive examinations and imaging studies are critical, and biopsy is essential for uncertain cases. Surgical intervention remains the primary treatment to mitigate risks of malignancy and fracture.
Keywords: Proximal femur; liposclerosing myxofibrous tumor; bone tumor; intramedullary nail.
Liposclerosing myxofibrous tumor (LSMFT) represents a relatively uncommon benign bone tumor with predilection for the proximal femur [1-5]. Typically, this condition manifests around 40 years old, without gender predilection [1-3,6]. Detection of the tumor commonly occurs incidentally on imaging studies or due to symptomatic pain, with pathological fractures being extremely rare [1]. This tumor can be mistaken for a numerous of lesions, including fibrous dysplasia, intraosseous lipoma, nonossifying fibroma, cartilaginous neoplasms, and osteoblastoma [1-4]. A small risk, less than 10% of malignant transformation has been reported [1-4].
In this singular case report, we meticulously document the clinical course of a female patient presenting with a geographic lesion in the proximal femur, diagnosed with LSMFT. Treatment included curettage, artificial bone matrix and nail fixation, leading to a satisfactory recovery. Complete clinical, radiological, and pathological findings, supplemented by retrospective discussion were presented.
A 60-year-old female patient sent to our orthopaedic department for a Magnetic Resonance Imaging (MRI) examination of her left hip, because a geographic lesion in the proximal femur was found by your physician.
She had a left hip pain while walking. The skin temperature of the left hip was normal and could move freely. There were no palpable masses during the physical examination.
Anteroposterior and lateral plain radiographs of the left hip showed a high-density shadow of the left proximal femur without fracture or bone destruction (Figure 1). MRI of the left hip showed a well-defined tumor in the proximal metaphysis of the left femur, with hypointense border on all sequences, with a matrix that is hypointense on T1. The cortical bone and others osteomuscular structures were not affected (Figure 2). Leading to the initial consideration of it being a benign tumor such as fibrous dysplasia, intraosseous lipoma or nonossifying fibroma. However, there was no clear diagnostic foundation. To alleviate her current symptoms and ascertain the nature of the lesion, we admitted her to the hospital and began preparing her for surgery.
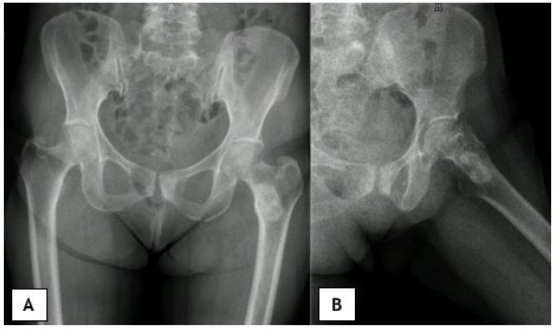
Figure 1: Preoperative X-ray view; A - Anteroposterior view; B - Lateral view.
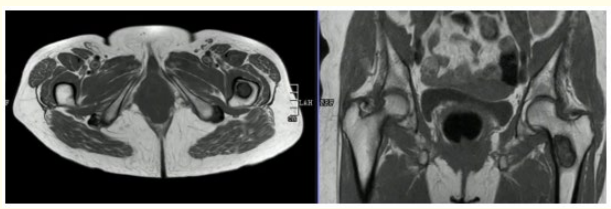
Figure 2: Preoperative magnetic resonance imaging, hypointense lesion on T1-weighted image.
Before the surgery, we carried out some examinations for her and found that all indicators of her haemoglobin, total white blood cell count and various specific indicators contained in white blood cell, platelets, coagulation function, calcium ions, potassium ions, antistreptolysin O, rheumatoid factor, hypersensitive c-reactive protein, fasting blood sugar, erythrocyte sedimentation rate, and renal function were normal. In addition, a higher alkaline phosphatase index (187.3U/L, normal range: 50-135U/L), other indicators of hepatic function were normal.
We performed a preoperative bone biopsy that suggested a Liposclerosing myxofibrous tumor.
After a comprehensive analysis of preoperative examinations, no contraindications were found.
An incision was performed on the lateral side of the left distal femur, and a bone block was removed at the location of the tumor. Additionally, the lesion in the medullary cavity was found to be fibrous-like and bone marrow-like in appearance. The lesion in the medullary cavity and the bone block was thoroughly curetted until the normal bone was visible and all specimens were sent for histopathological analysis. The bleeding was thoroughly stopped, then the incision was rinsed with distilled water and normal saline. The artificial bone matrix was filled in the defect and the removed bone block is put in place. We did not perform plate fixation, we prefer the use of an intramedullary nail with a femoral neck lag screw, because decreased the risk of postoperative fracture and the risk of thrombosis due to early failure of functional exercise.
On the microscopic examination a mixofibrous tissue and bone trabeculae like fibrous dysplasia were observed. Immunoreactivity with smooth muscle actin in the fusiform cells of stroma was observed. Considering these findings, the diagnosis of the lesion was reported as liposclerosing myxofibrous tumor (Figure 3).
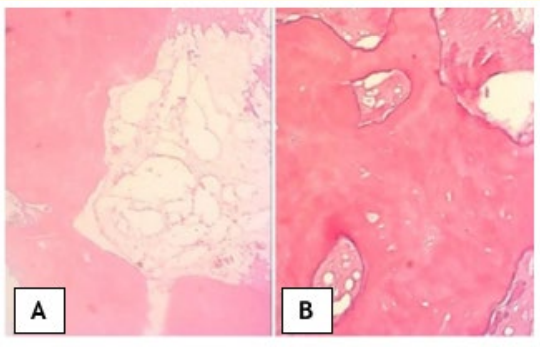
Figure 3: Microscopic images, myxoid degeneration, fat necrosis, calcified bone tissue, irregular calcification, collagen degeneration and cystic degeneration of fibrous tissue are seen (magnifications of ×4 in A and x10 in B).
We didn’t give her follow-up radiation and chemotherapy because it’s a benign lesion reported in the literature.
The patient recovered well after the surgery. The alkaline phosphatase index decreased on the 1st day after the surgery and remained normal after the 3rd postoperative day.
Anteroposterior and lateral radiographs of the left femur showed no aberrant signal at the left distal femur on the 3rd day after the surgery (Figure 4). On the fifth day after the operation, she was discharged from the hospital and returned home.

Figure 4: Postoperative X-ray view 3rd day after the surgery.
After six months, she returns to normal daily life with no symptoms of discomfort, anteroposterior and lateral radiographs showed good recovery of the left proximal femur (Figure 5).
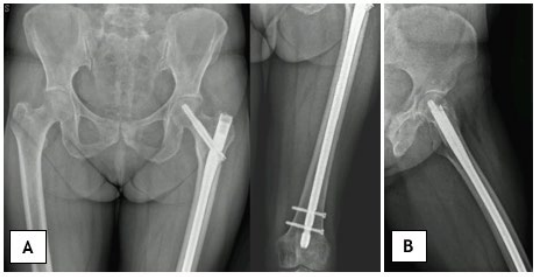
Figure 5: Postoperative X-ray view six months after surgery; A - Anteroposterior view; B -Lateral view.
During the twelve months of follow-up, the symptoms and images of her affected limb showed no signs of recurrence.
Liposclerosing myxofibrous tumor was first described by Ragsdale in 1986. [5-7] It has a complicated structure, which histopathologically includes myxoid areas, osteoclastic activity, bone trabeculae similar to fibrous dysplasia, fat necrosis, ischemic ossification and rarely cartilage components. [5-9] The average age of disease occurrence is 40 years. The frequency of males and females is equal. Although a large portion of the proximal femur is affected, other localizations have also been reported. [5].
Radiologically, it is a well-circumscribed lesion surrounded by sclerosis, which shows calcification occasionally. [3,4,9] Definitive treatment was planned when the biopsy confirmed the diagnosis.
Liposclerosing myxofibrous tumor has been reported to be associated with fibrous dysplasia because of its radiological and histopathological features. They are intramedullary well-limited lesions just as classic fibrous dysplasia. [7] Indeed, Matsuba., et al. [10] detected Gs alpha mutation at Arg201 codon in two cases of liposclerosing myxofibrous tumor. These mutations have also been identified in patients with McCune- Albright syndrome, and monostotic and polyostotic fibrous dysplasia [10-11].
Curettage, bone grafting and cementing by intralesional approach are sufficient for treatment due to its being a benign tumor. Yet, malignant transformation has also been reported, it’s rarely [5,6,8]. In our case, we applied curettage, artificial bone matrix and fixation with an intramedullary nail system with a femoral neck lag screw [11].
In the surgical treatment, aggressive curettage of the lesion and use of high-speed burr are important.
We used a intramedullary nail system with a femoral neck lag screw in order to prevent the risk of fracture at the load carrying area, where we opened a bone window, and enable immediate weight-bearing, thus reduce the risk of thromboembolism. Recurrence was not detected at the 12th month control.
Malignant transformations such as fibrosarcoma, malignant fibrous histiocytoma and telangiectatic osteosarcoma have been reported [5,6,8]. In the literature, a malignant transformation rate of 10% has been reported [4,7].
In summary, when evaluating heterogeneous, lytic lesions with surrounding sclerosis in the proximal femur, one should consider the possibility of a liposclerosing myxofibrous tumor. Comprehensive physical examinations and imaging studies are vital for all bone tumors. If there is any uncertainty in the diagnosis, performing a biopsy before proceeding with definitive treatment is of utmost importance. Given the potential risks of malignancy and fracture, surgical intervention is recommended as the primary treatment approach. Larger case series are necessary to better understand the relationship between these tumors and fibrous dysplasia lesions, as well as the overall disease progression.
Copyright: © 2024 David Gouveia., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.