Edir Soccol Junior1*, Mauro G Rodrigues2, Vinicius C Guarienti2, Neri Machado Jr3, Fabio A Cavali4, Fernando Soccol5 and Vanessa Marcolina6
1Department of Orthopedics and Traumatology, Department of Hip and Pelvic Surgery of the Pato Branco Polyclinical Institute, Paraná, Brazil
2Resident of Orthopedics and Traumatology, Department of Orthopedics and Traumatology of the Pato Branco Polyclinical Institute, Paraná, Brazil
3Director of the Department of Orthopedics and Traumatology of the Pato Branco Polyclinical Institute, Paraná, Brazil
4Chief of Residency of the Department of Orthopedics and Traumatology of the Pato Branco Polyclinical Institute, Paraná, Brazil
5Department of Orthopedics and Traumatology of the Pato Branco Polyclinical Institute, Paraná, Brazil
6Medicine Student from the University Center of Pato Branco, Pato Branco, Paraná, Brazil
*Corresponding Author: Edir Soccol Junior, Department of Orthopedics and Traumatology, Department of Hip and Pelvic Surgery of the Pato Branco Polyclinical Institute, Paraná, Brazil.
Received: February 05, 2021; Published: February 26, 2021
Objectives: to analyze the differences in the post-surgical result in the quality of fracture reduction in which the orthopedic traction table was used as a technique for intramedullary osteosynthesis.
Methods: The present study consists of a comparative quantitative study using secondary data from medical records of 79 patients who suffered a transtrochanteric fracture and underwent surgical treatment with and without the use of a traction table. Measurement data of the tip-apex distance (TAD) was collected on the immediate postoperative radiography, presence of the cut-out, analysis of loss of reduction, evaluation of possible failure in the synthesis material and analysis of fracture consolidation, and post-surgical complications. The Mann-Whitney U test and the Fisher Exact test were used to compare the traction table's use and non-use, adopting p < 0.05.
Results: There was a greater proportion of women with this type of fracture (75.9%). Complications related to surgery occurred in 7.9% of cases. No significant difference was found for TAD (p = 0.39), consolidation indicators (p = 0.52) and fracture-related post-surgical complications (p = 0.05) between the use and non-use of the traction table.
Conclusion: No significant difference was seen for TAD, consolidation, and the occurrence of post-surgical complications related to fracture between the use or not of a traction table to perform the surgical procedure.
Keywords: Femoral Fractures; Orthopedic Procedures; Orthopedic Traction Table; Hip Fractures
Transtrochanteric fractures consist of one of the types of hip fractures, with the proximal femur being the site affected in this lesion, more precisely the area between the greater and the lesser trochanter. Hip fractures affect mainly the elderly population, since bone density is decreased, and the presence of comorbidities is more common in these people [1,2].
The incidence of these fractures has been increasing in recent years, and it is likely to double in the next 20 years due to the worldwide increase in life expectancy. In Brazil, between 2008 and 2012 over 181 thousand cases of femur fracture were identified in the Hospital Information System of the Unified Health System, being more prevalent in women [2]. Such numbers highlight the great socioeconomic impact that the population suffers as consequence of this type of fracture [2,3].
The treatment of hip fractures aims to stabilize the fracture and allows patients to have a quick functional recovery of the limb and return to daily activities [4]. In view of this scenario, the treatment is carried out with the purpose of providing faster fracture stabilization possible to restore the function of the affected limb and to prevent future complications from arising.
Therefore, both conservative and surgical treatment are an option and the conservative treatment in transtrochanteric fractures is only assigned to patients with comorbidities that put them at risk if they undergo anesthesia and surgery. As for surgical treatment, the best method consists currently of internal fixation, which can be performed in several ways, such as: side plate with sliding screw, cephalomedullary nail, among others; and the indication for the use of each one depends on the fracture pattern, such as unstable and stable, the surgeon's preference and material availability [5].
The treatment of internal fixation by cephalomedullary nail has been shown to be very effective in this scenario, as it allows the patient to walk early, in addition to offering less surgical trauma due to its percutaneous insertion. The nail has the function of supporting the collapse and offering the medialization of the distal fracture fragment, being widely used mainly in transtrochanteric fractures of unstable femurs. For the insertion of this device, different techniques can be used according to the choice of orthopedists, such as the use or not use of the orthopedic traction table [5,6].
The traction orthopedic table is used in various hip and femur surgeries, mainly in cases of fractures and arthroscopies and generally requires a smaller team. This technique increases the quality of the reduction and allows circumferential access to the injured side, since it is performed with the patient in a supine position, traction on the affected limb and good support without the need for an assistant. The table arm facilitates the use of fluoroscopy, which can then be done in different positions, allowing anteroposterior, lateral and circumferential images to be obtained [7-10].
In view of the fact that transtrochanteric hip fractures are very prevalent today, especially in the elderly, and that surgical treatments are relatively expensive, so if done correctly they avoid other complications and surgical procedures. The present study aims to analyze whether there is a difference in the post-surgical result, in terms of the quality of reduction of patients in whom the orthopedic traction table was used as a technique for intramedullary osteosynthesis; in an attempt to offer the best type of treatment and thus, a better quality of life for patients. It is hypothesized that patients undergoing surgery using an orthopedic traction table have better results in the quality of the reduction and less complications resulting from the surgical procedure.
The present study consists of a comparative quantitative study using secondary data from medical records of patients who suffered hip fractures and underwent surgical treatment. The present study was approved by the Research Ethics Committee involving human beings of the University Center of Pato Branco under protocol 4,284,311.
Cohort and sampleThe cohort was composed of patients who suffered hip fractures with surgical treatment performed between the period of March 2018 to March 2020 at the Pato Branco Polyclinic Institute. These data were accessed through an electronic data storage base, where medical records were selected.
Assessment of post-surgical treatment resultsThrough the assessment of medical records and radiographs, data measuring the "tip-apex" distance (TAD) were collected on the immediate postoperative radiography [11,12] (Figure 1), assessment of the presence or not of the cut-out, analysis of the loss reduction or not, assessment of possible failure in the synthesis material and fracture consolidation analysis.
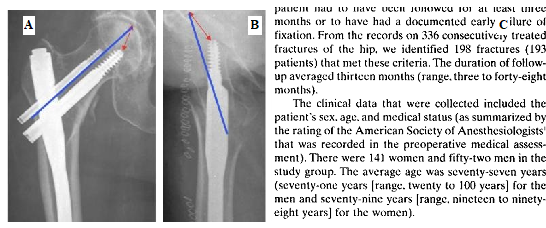
Figure 1: TAD Calculation. A: Anteropoterior View; B: Side View; C: TAD Calculation (Source: Baumgaertner., et al. [12]).
Data processing and statistical analysisCentral tendency and dispersion measures were used to describe continuous variables and relative and absolute frequency for categorical variables. The normality of the data was analyzed by the Shapiro-Wilk test and by the visual analysis of the histogram. Given the non-normal distribution of the data, they were represented by median and interquartile range. The comparison of TAD and consolidation between patients who underwent surgery with or without using the orthopedic traction table was performed using the Mann-Whitney U test. The effect size was obtained by calculating the probability of the superior outcome (PSO) [13]. Fisher's exact test was used to compare complications in the post-surgical period. For all analyzes, the significance level of p < 0.05 was adopted. All analyzes were performed using the STATA MP 14.1 software.
From March 2018 through March 2020, 196 patients undergoing care for fractures in the hip region were identified. Of these 196 patients, 79 (mean age 80.4 ± 10.4 years) had a transtrochanteric fracture and made up the sample of the present study.
Most participants were female (75.9%), underwent a surgical procedure without using an orthopedic traction table (53.1%), had surgery performed on the left side (57.0%). Regarding post-surgery complications, only 7.9% were related to fracture (cut-out, delayed consolidation or screw displacement) and the vast majority of patients did not suffer any complications after surgery (78.9%) (Table 1).
| n | % | |
|---|---|---|
| Sex | ||
Female |
60 |
75,9 |
Male |
19 |
24,1 |
Use of traction table |
||
No |
42 |
53,1 |
Yes |
37 |
46,9 |
Surgery Side |
||
Right |
34 |
43,0 |
Left |
45 |
57,0 |
Post-surgery Complications |
||
None |
60 |
78,9 |
Non-related to the fracture |
10 |
13,2 |
Cut-out, consolidation delay or screw displacement |
6 |
7,9 |
Table 1: Characteristics of the participants.
Table 2 shows median values and interquartile range of the TAD and consolidation, as well as the comparison of these values between patients who underwent surgical procedures with and without the use of the orthopedic traction table. There was no significant difference in TAD and consolidation between patients who were and were not submitted to the use of the orthopedic traction table.
| Use of orthopedic traction table | ||||||
|---|---|---|---|---|---|---|
Total Sample |
No |
Yes |
||||
| Median (IQR) | Median (IQR) | Median (IQR) | U | p | PSO (No use > Use of the traction table) | |
TAD |
1,92 (1,10) |
1,95 (1,37) |
1,92 (0,86) |
0,86 |
0,39 |
55,7% |
Consolidation* |
6,0 (0,0) |
6,0 (1,0) |
6,0 (0,0) |
0,64 |
0,52 |
54,0% |
Table 2: Median and interquartile (IIQ) for TAD and consolidation for the general sample and according to the use of the orthopedic traction table.
TAD: Tip-Apex Distance; IQR: Interquartile Range; PSO: Probability of Superior Outcome; U: Mann-Whitney U Test; *: n = 58.
Complications related to the fracture occurred only in patients not submitted to the use of the orthopedic traction table (n = 6, 15.0%), however, no significant difference was seen between patients who were and were not submitted to the use of the orthopedic traction table (Fisher's exact p-value = 0.05) (Figure 2).
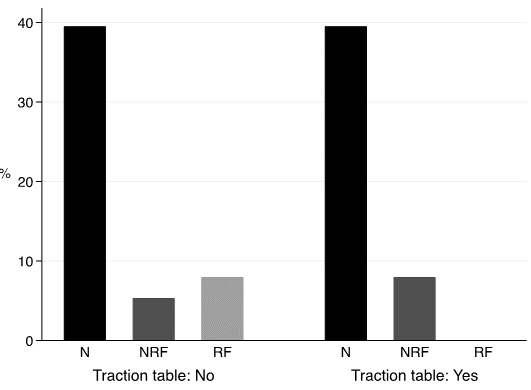
Figure 2: Postoperative complications according to the use of the orthopedic traction table. (de Fisher’s exact test p-value = 0,05). N = None; NRF: Non-Related to the Fracture; RF: Related to the Fracture.
The present study analyzed secondary data from 79 patients who underwent a surgical procedure for the treatment of transtrochanteric fractures. There was a greater proportion of women with this type of fracture compared to men (75.9%). It was also found that 7.9% of the cases suffered post-surgical complications related to the fracture. No significant difference was found for TAD and consolidation indicators between patients who underwent surgical procedure with or without the use of the orthopedic traction table. Complications related to the fracture occurred and only in patients who underwent surgery without the use of the traction table, however, such data should be viewed with caution given the absence of statistical significance in the comparisons.
The highest proportion of women affected by this type of fracture seen in the present study, is in line with that reported in epidemiological data from the Brazilian population [2]. Osteoporosis and its higher incidence in women represents the main reason for this higher occurrence of fractures in the female gender [14].
The orthopedic traction table is used in various surgical procedures performed on the hip and femur, such as fracture fixation, hip arthroscopy and less invasive arthroplasty [7]. Advantages of using the traction table include sustained longitudinal traction without the need for an assistant, and circumferential access to the injured extremity for manipulation, exposure and image [10]. Additionally, the use of the traction table reduces the number of assistants needed to perform the surgical procedure [8].
The present study did not find significant differences in TAD and consolidation among patients undergoing surgery with or without a traction table. Such results are corroborated by Sonmez., et al. [10] and Souza., et al. [9] who found no difference in TAD between patients who underwent surgery in lateral decubitus and patients who underwent surgery using the traction table.
Despite the occurrence of post-surgical complications related to the fracture being seen only in patients in the group without using a traction table, there was no statistical significance in the comparisons. Stephen., et al. [15] found no significant difference in post-surgical complications in patients undergoing surgery with or without the use of a traction table. More specifically, complications related to the increase or shortening of the femur as well as the functional state, did not differ between the techniques.
Despite the non-identification of differences in the TAD, consolidation and occurrence of complications with the use of the traction table, it is important to note that complications may be related to the use of this implement, such as misalignment of the affected limb, neurological and soft tissue injuries, and compartmental syndrome of the uninjured limb [7,10]. Therefore, surgeons must be aware of the advantages and disadvantages of using the traction table [7].
The present study is subject to limitations. The sample size may have limited comparisons of post-surgical complications between techniques. Complications occur in a minority of cases and this can limit these comparisons. Additionally, the data obtained from secondary sources are limited to the information provided in the medical records and medical examinations, thus limiting the inclusion of more variables that could assist in the contributions of the present study.
There was a greater occurrence of surgical procedures performed for the treatment of transtrochanteric fractures performed in women and post-surgical complications related to the fracture occurred in 7.9% of cases. No significant difference was seen for TAD, consolidation and the occurrence of post-surgical complications related to fracture between the use or not of a traction table to perform the surgical procedure.
Citation: Edir Soccol Junior., et al. “Comparative Study of the Results after Surgical Treatment of Transtrochanteric Hip Fractures Using a Cephalomedullary Device with and without the Use of the Orthopedic Traction Table".Acta Scientific Orthopaedics 4.3 (2021): 49-53.
Copyright: © 2021 Edir Soccol Junior., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.