José Luis Mosso Vázquez1,2* and Enrique Jesús Rodriguez3
1School of Medicine, Universidad Panamericana, México
2Regional and General Hospital No. 25 IMSS, Mexico
3Medical Center la Raza, IMSS, UMAE, Mexico City, Mexico
*Corresponding Author: José Luis Mosso Vázquez, School of Medicine, Universidad Panamericana and Regional and General Hospital No. 25 IMSS, Mexico.
Received: February 19, 2021; Published: March 11, 2021
Objective: Demonstrate the utility of Mobile phones for Telemedicine in emergency surgery. Surgeon shared patient´s medical record, pictures and videos with anesthesiologist, scrub nurses to prepare on time operating room and surgical tools before emergence surgery.
Methodology: In the preoperative, surgeon made medical text and images with a mobile phone of each patient in emergence service and send this information to anesthesiologists and scrub nurses. In the intraoperative an assistant made pictures of surgical field. In the postoperative surgeon made pictures of organs or tissues removed and share all information with physicians of emergence service also. 77 cases were recorded with this technique.
Results: Anesthesiologists evaluated 77 cases in the preoperative where images from the patient´s mouth, teeth, neck size and anatomical surgical regions were enough to be evaluated. With aware patient state, endotracheal tube size and preparation of medication for general or regional anesthesia were evaluated also thanks of medical pictures and data. Surgeon sent anesthesiologist a summary of medical record of each patient by messages, pictures and videos. Pictures resolution was enough to evaluate airways of each patient to select the correct endotracheal tube size.
Conclusion: Pictures resolutions were enough to prepare adequate surgical and anesthesiologist tools in the preoperative to avoid lost time in the intraoperative. The first significant conclusion is for the quality of surgical attention for patients because we can reduce intraoperative complications such as bleedings and losing time for intubations. Otherwise, with smart phones we improve traditional medical relationship between surgeons, anesthesiologist, scrub nurse, interns, residents, undergraduate students, and emergence team. The cost benefit of this project is the reduction of surgical complications as bleeding and short surgical time. In this technique, we add technology with smart phones inside traditional communications between physicians, sending us medical data of patients in the preoperative 7 years later, mobile phones generations have been improving emergence in surgery communications and in Telemedicine with high resolutions of medical images and videos. Up today, early 2021, smartphones demonstrate the potential into SARS II, Covid-19 Global Pandemic. Videoconference, social media are the powerful technology in the humankind hands.
Keywords: Smartphones; Telemedicine; Emergency Surgery
Mobile phones in medicine have become a potential medical tool for communication, telemedicine, medical education, surgical training and surgical tool. Up today, medical students, interns, residents and medicine professionals have communication with a mobile phone in the worldwide. Medical and surgical second opinion is the must application using text messages, pictures, and patient´s videos (Telemedicine, education) [1-4]. Mobile phones are being used as surgical simulators for laparoscopic trainers (Surgical education). Mobile phones have been used as scope (Laparoscope) to perform laparoscopic surgeries (surgical tool). Microscopes, dermatoscopes, colposcopes, ophthalmoscopes, microscopes and other devices are using mobile phones as medical tools to perform diagnosis in many medical areas. Mobile phones are being using as virtual anesthesia in Cibertherapy to reduce pain and anxiety during medical and surgical procedures (https://www.youtube.com/watch?v=V4wDEXF1_ec) [5-7]. In this project, mobile phones generations in 2011 have been used just to share text message, patient´s pictures and videos between emergence physicians, surgeon [8], residents and anesthesiologists.
In Emergency Surgery, surgeons have contact with two groups of physicians to organize an operating room, they are Medical Emergencies Physicians (MEP) and anesthesiologists. MEP request patient´s surgeon evaluation with all patient´s laboratory results, X rays, ultrasounds, CT Scanners. Traditionally, Surgeons arrive Emergency service to perform surgical assessments. Then, He goes to operating room to present patients to anesthesiologist giving a paper request with general data and consent informed of each patient and relatives. Traditionally, surgeon also explains the clinical condition of patients to anesthesiologists, who evaluate patients with the data in the request paper and furthermore evaluates the patient directly on the bed in emergence service. Under these conditions, anesthesiologists prepare medications for general or regional anesthesia, endotracheal tube, monitors, etc. Scrub nurses prepare operating room with surgical instruments for thorax, neck, or abdomen regions. This entire scenario is prepared under surgeon explanation and the medical file contains a summary of general conditions of each patient (Name, age, register number, diagnosis, surgical procedure, laboratories count as: Hemoglobin, hematocrit, time coagulation, glucose and signatures with written consent informed). By other hand MEP leaves patients when they go to operating rooms, they don´t know about surgical results except if surgeon casually met MEP to comment the case by oral explanation or if the MEP is interested in a particular case that search surgeon to ask about surgical results in the postoperative or many days after surgery.
The purpose of this traditionally method is to present patients with smartphones sending text message, pictures and videos to surgical team in the preoperative, intraoperative and postoperative. This method will short time to prepare anesthesiologist equipment, operating room and surgical tools for emergence surgery.
This low cost with mobile phones for Telemedicine, is easy to use, easy to carry and provide the following advantages. Anesthesiologists evaluate patients in critical conditions and prepare with high security all material they need for anesthesia; scrub nurse prepare their appropriate surgical tools. Patients have an adequate surgical treatment without lost time avoiding surgical complications and better recovery in the postoperative. MEP has the opportunity to know the evolution of each patient they treated since their admission in emergence service.
Telemedicine in the last decade is in progress because Smart phones evolutions permit us a better communication such as: Social networks, chats, Internet and all applications we know. There are many publications where iPhones and other smart phones have been used with similar purpose [9-19].
Surgical team and material. The project was developed on weekends since 2011 to 2018 in the Departments of Surgery, emergence and anesthesia at the Regional Hospital Number 25 of the IMSS (Instituto Mexicano del Seguro Social “Social Security Mexican Institute”) in Mexico City. The team participants are one surgeon, 4 anesthesiologists, 8 Medical Emergence Physicians, 5 residents of surgery, and 2 scrub nurses. In early 2011 surgeon´s smart phone starts this project with an I Phone G3s with 32 Megapixels and Internet service. An Illuminated loup (Led light) is used with 30 X-25MM, Model MG21011 LED 6-shaped jewelry magnifier Magnification 40 X Lens diameter 25 mm, it uses 3 LR927 batteries. Anesthesiologist´s smart phones equipments are, I Phone G4, Samsung with 3.2 megapixels, Samsung tocco stylish touch, with Wi Fi and 5 Megapixels and Internet. MEP smart phones are different (See table 1) and additionally they use a computer of emergence service with Intranet of the Institute (IMSS) where they opened an email account to review all data and pictures emailed from surgeon. In 2018 surgeon´s mobile phone was G6.
Methodology: Criteria for selected patients are patients insured or not to the IMSS and with written informed consent. This project began in March 2011. We selected 77 patients with critical or acute diseases and trauma. 18 to 95 of age, 38 males and 39 females, all in critical care conditions, 8 cases with acute infectious diseases in soft tissues, 7 cases with trauma, 7 cases with complicated abdominal and inguinal hernias, 55 cases with acute abdomen pain and two with respiratory failure.
Criteria for no selected patients. Patients who died in the emergences service, and not been interested to participate in the project.
PreoperativeSurgeon arrives to Emergence Service on Saturday and Sunday morning and in the course of the weekend. He evaluates patients in critical care together with MEP and residents who present him a summary or background of each patient. Surgeon evaluate patients aware or not on their emergence´s bed to explore them. With previous explanation and purpose of the project and permission of each patient to make pictures of their noses, open mouths, and necks of all patients and in abdomen and thorax region. If patient can´t talk, surgeon can get information through paramedics, relatives, parents, friends or anyone. Once, He gets Medical information exploration He reviews labs counts results and X ray images. He sends the following information in text message to the anesthesiologist by mobile phone (iPhone G3), patient name, age, weight, a medical background and general condition of the patient (Blood pressure, hearth and breath rate, and temperature) with their labs results such as: White cell blood, blood coagulation time, hemoglobin, creatinine, platelets and pictures including x ray, ultrasound, scanner, and electrocardiogram, Anesthesiologist share all data and images with scrub nurses and residents of anesthesia. To avoid the reflection of X ray pictures, we cover of dark around the pictures to get better images without shadows or reflections. When the surgical diagnosis is integrated, surgeon request surgery with a format paper into operating room with the anesthesiologist who already knows the patient´s presumptive diagnosis, and surgical planning, in addition of the consent informed signed by patient, relatives and surgeon.
IntraoperativeWhen patient is at the operating room, anesthesiologist gets additional information reading the complete file of the patient. Surgeon makes pictures of the region to operate. Once the patient is ready (Washed and dressed), surgeon begin his procedure traditionally and when He consider necessary someone not involved in the surgery and anesthesia directly make pictures or videos focused to specifically organs or tissues to be shared with MEP.
PostoperativeIn 2011 surgeon makes pictures of the removed organs before placing in formalin. In the case of gallbladders, cysts, tumors, appendix, and others organs removed, surgeon open organs to measure and describe colors, size, before to send the samples to pathology service. When surgeon gives information about surgical findings to relatives of the patient, He doesn´t show them any picture. In the first opportunity, surgeon send messages to an email account created by MEP, in the first one describes surgical findings, and in the second one, the preoperative, intraoperative and postoperative pictures of the patient and his or her medical images. Surgeon sends all Medical information by Internet on Saturday or Sunday night. 6 years later, on 2018 exist social media used to share medical information easily by WhatsApp, Facebook, etc.
Anesthesiologists evaluated 77 cases in the preoperative where images from the mouth, neck, and anatomical surgical regions were enough to be evaluated. Patients participated and underwent emergence surgeries at the Regional Hospital, since February 2011 to October 2011 on weekends. 39 Females and 38 Males, 21 to 92 of age, 43 surgeries in abdomen, 7 surgeries in soft tissues on arms, hands and legs, 6 surgeries in abdominal and inguinal wall, 7 trauma surgeries in the neck, thorax rectum. 2 patients died in the intraoperative and 5 in the postoperative. The relationship between surgeons, anesthesiologists and Emergence Physicians was so close thanks for using smart phones to know the clinical condition and to permit prepare all anesthesiology and surgical equipment at time.
PreoperativeThe most important pictures for anesthesiologists to use general anesthesia were from the nose, open mouth, and neck of each patients because they could appreciate the airway and determine the size of the endotracheal tube, if the pictures include x ray or scanner images of the neck, they could consider the grade of difficulty to introduce the tube around disorders of anatomy of trachea, larynx, or cervical spine. The most important pictures to use regional anesthesia were from the back of the patient and x ray pictures to evaluate the thoracic and lumbar spine. The videos of each patient are so important for anesthesiologist because they can appreciate the general condition of each patient, first they can see if they are aware or not, second, the airway, with the presence or not of endotracheal tube, and third, they can know the degree of injury or the region of the acute disease. This information will permit anesthesiologists determine what kind and better anesthesia they can use and all alternatives to prepare medications at time. The most important pictures for scrub nurse are from the arms (to appreciate peripheral, central venous catheters or urinary catheters) of the patients and the affected region with a disease or injuries because they will prepare the surgical instruments for the neck, chest, abdomen, or vascular tools. Videos also permit them to know if patients have gastric, urinary, or central catheter because they most have permeable line veins to introduce medications. The time to prepare patient is shorter because all team in operating room prepare all surgical tools at time, and if they don´t have the necessary equipment they can search them at time. Only videos couldn´t sent by internet because are heavy and it was necessary to present directly with the phone for all team. The only delay to begin a surgery we have, was, haven’t at time the complete file in emergence department. Mandatory requirement must be changed to avoid lost time in emergences surgeries.
IntraoperativeThe surgical time is shorter because surgeon don´t lost time for all equipment ready before surgery and all surgical team develop as well with an excellent relationship. Surgeon, anesthesiologist and scrub nurses work together, knowing completely the patient. Pictures or videos made in the intraoperative take few seconds for residents or nurses. Two patients died in the intraoperative for acute disease related with sigmoid volvulus and sepsis by violin spider bite.
PostoperativeThe day after surgery, surgeon send all images made in the intraoperative by email to all MEP involved in the case to share all surgical findings and corroborate the previous or preoperative diagnosis with the surgical or intraoperative results. Excellent reasons to be evaluate their clinical experience themselves. Furthermore, the complete cases can be prepared to present in conference or to be published.
| Physician | Sex | Smart phone | Internet | Video | |
|---|---|---|---|---|---|
1 |
Surgeon |
M |
iPhone G3 A1324 |
No |
Yes |
2 |
Resident I of surgery |
F |
iPhone G4 (GSM)/(GSM, A) A1332 |
Yes |
Yes |
3 |
Resident I of surgery |
M |
iPhone G3 A1324 |
Yes |
Yes |
4 |
Resident I of surgery |
M |
Black Berry 8520 8530 |
Yes |
Yes |
5 |
Resident I of surgery |
M |
Nokia N70 |
Yes |
Yes |
6 |
Resident I of surgery |
M |
Nokia N71 |
No |
No |
7 |
Anesthesiologist |
M |
iPhone G3 A1324 |
Yes |
Yes |
8 |
Anesthesiologist |
F |
Black Berry 8520 8530 |
Yes |
Yes |
9 |
Anesthesiologist |
F |
Nokia E63 |
Yes |
Yes |
10 |
Anesthesiologist |
F |
Nokia N71 |
Yes |
Yes |
11 |
Scrub nurse |
F |
Samsung S |
No |
Yes |
12 |
Scrub nurse |
F |
Samsung S |
Si |
Si |
13 |
Emergence physician |
M |
LG Optimus Me P350 |
No |
No |
14 |
Emergence physician |
F |
LG Optimus Me P350 |
No |
Yes |
15 |
Emergence physician |
F |
Motorola Atrix |
Yes |
Yes |
16 |
Emergence physician |
M |
Sony Ericsson Arc |
Yes |
Yes |
17 |
Emergence physician |
F |
Nokia N72 |
Yes |
Yes |
18 |
Emergence physician |
F |
I Phone G4 |
Yes |
Yes |
19 |
Emergence physician |
M |
Nokia N70 |
Yes |
Yes |
20 |
Emergence physician |
F |
Samsung S |
No |
No |
21 |
Resident I Emergence physician |
F |
LG Optimus Me P350 |
No |
No |
Table 1: Smart phones and physicians on 2011.
| Physician | Sex | Smart phone | Internet | Video | |
|---|---|---|---|---|---|
1 |
Surgeon |
M |
iPhone 6s |
Yes |
Yes |
2 |
Resident I of surgery |
F |
iPhone 8 Plus |
Yes |
Yes |
3 |
Resident I of surgery |
M |
Samsung Galaxy S6 |
Yes |
Yes |
4 |
Resident I of surgery |
M |
iPhone 8 Plus |
Yes |
Yes |
5 |
Resident I of surgery |
M |
iPhone 6 |
Yes |
Yes |
6 |
Resident I of surgery |
M |
iPhone 8 Plus |
No |
Yes |
7 |
Anesthesiologist |
M |
iPhone X |
Yes |
Yes |
8 |
Anesthesiologist |
F |
Samsung S8 Edge |
Yes |
Yes |
9 |
Anesthesiologist |
F |
Samsung S8 Edge |
Yes |
Yes |
10 |
Anesthesiologist |
F |
Samsung S8 Edge |
Yes |
Yes |
11 |
Scrub nurse |
F |
Samsung S7 Edge |
Yes |
Yes |
12 |
Scrub nurse |
F |
iPhone 6s |
Yes |
Yes |
13 |
Emergence physician |
M |
Sony E5 |
Yes |
Yes |
14 |
Emergence physician |
F |
Samsung S7 Edge |
Yes |
Yes |
15 |
Emergence physician |
F |
Galaxy Note 8 |
Yes |
Yes |
16 |
Emergence physician |
M |
iPhone XR |
Yes |
Yes |
17 |
Emergence physician |
F |
Galaxy S7 Edge |
Yes |
Yes |
18 |
Emergence physician |
F |
iPhone XR |
Yes |
Yes |
19 |
Emergence physician |
M |
iPhone XR |
Yes |
Yes |
20 |
Emergence physician |
F |
iPhone XR |
Yes |
Yes |
21 |
Resident I Emergence physician |
F |
iPhone 7 |
Yes |
Yes |
Table 2: Smart phones and physicians in 2018.
| Case | Sex | Diagnosis | Surgical treatment | Region |
|---|---|---|---|---|
1 |
M |
Hidrocholecyst |
Laparoscopic cholecystectomy |
Abdomen |
2 |
M |
Piocholecyst |
Laparoscopic cholecystectomy |
Abdomen |
3 |
F |
Acute cholecystitis |
Laparoscopic cholecystectomy |
Abdomen |
4 |
F |
Mesenteric Thrombosis |
Intestinal resection and anastomosis, ileostomy. |
Abdomen |
5 |
F |
Renal failure |
Installation of Tenckhoff catheter |
Abdomen |
6 |
M |
Appendicitis stage IV |
Laparoscopic appendectomy |
Abdomen |
7 |
F |
Acute abdomen |
Laparotomy |
Abdomen |
8 |
F |
Appendicitis stage III |
Appendectomy |
Abdomen |
9 |
F |
Appendicitis stage IV |
Laparoscopic appendectomy |
Abdomen |
10 |
F |
Appendicitis stage III |
Appendectomy |
Abdomen |
11 |
M |
Appendicitis stage IV |
Appendectomy |
Abdomen |
12 |
F |
Appendicitis stage II |
Appendectomy |
Abdomen |
13 |
F |
Appendicitis stage IV |
Appendectomy |
Abdomen |
14 |
F |
Perforated sigmoid |
Sigmoidectomy and colostomy |
Abdomen |
15 |
F |
Perforated sigmoid |
Sigmoidectomy and colostomy |
Abdomen |
16 |
M |
Perforated sigmoid |
Sigmoidectomy and colostomy |
Abdomen |
17 |
M |
Perforated sigmoid volvulus |
Sigmoidectomy and colostomy |
Abdomen |
18 |
M |
Giant abdominal cyst |
Cyst resection, laparotomy |
Abdomen |
19 |
F |
Giant ovarian cyst |
Ovarian cyst resection |
Pelvis |
20 |
F |
Small bowel necrosis |
Resection and intestinal anastomosis. Lysis of adherents. |
Abdomen |
21 |
F |
Ectopic pregnancy, hypovolemic shock |
Laparotomy drainage of 3 liters of blood, left salping oophorectomy |
Pelvis |
22 |
M |
Bladder perforation |
Laparotomy and Cistorraphy |
Abdomen, Urinary tract. |
23 |
F |
Left ovarian cyst ruptured |
Resection of left ovarian cyst |
Pelvis |
24 |
F |
Incarcerated umbilical hernia |
Omentectomy and umbilical hernia repair. |
Abdomen |
25 |
F |
Incarcerated bowel |
Intestinal resection and anastomosis and umbilical hernia repair. |
Abdomen |
26 |
F |
Incarcerated umbilical hernia. |
Umbilical hernia repair and mesh placement. |
Abdominal wall |
27 |
F |
Incarcerated umbilical hernia. |
Umbilical hernia repair |
Abdominal wall |
28 |
F |
Incarcerated crura hernia |
Crura hernia repair with mesh placement. |
Abdominal wall |
29 |
M |
Bleeding in left inguinal radiated zone. |
Inguinal zone exploration and laparotomy. |
Abdomen and Abdominal wall |
30 |
M |
Fasciitis in right leg |
Fasciotomy and necrosectomy |
Soft tissue |
31 |
M |
Fournier´s syndrome |
Fasciotomy and necrosectomy |
Perineum |
32 |
M |
Abscess in the neck |
Abscess drainage and surgical cleaning |
Neck |
33 |
M |
Fasciitis for violin spider sting |
Fasciotomy and necrosectomy |
Neck |
34 |
M |
All right arm with necrosis for violin spider sting. |
Fasciotomy and necrosectomy. |
Arms |
35 |
F |
Necrosis of right hand for violin spider sting. |
Fasciotomy and necrosectomy |
Arms |
36 |
M |
Spleen bleeding for abdominal trauma |
Splenectomy |
Abdominal trauma |
37 |
F |
Vein cava injury for gun shot |
Cava vein repair |
Thoracic trauma |
38 |
M |
Neck injury for glass |
Neck exploration |
Neck trauma |
39 |
M |
Hemothorax for gun shot. |
Thorax drainage. |
Thoracic trauma |
40 |
F |
Acute Cholecystitis |
Laparoscopic cholecystectomy |
Abdomen |
41 |
M |
Acute Cholecystitis |
Laparoscopic cholecistectomy |
Abdomen |
42 |
F |
Postsurgical adhesions |
Adherensiolisis, laparotomy |
Abdomen |
43 |
M |
Gastric necrosis for hiatal hernia strangulated. |
Partial gastrectomy with gastric sleeve and diaphragmatic pillars repair. |
Abdomen |
44 |
F |
Appendicitis stage IV |
Appendectomy |
Abdomen |
45 |
M |
Giant left inguinal hernia. |
Mac Bay hernia repair, laparotomy, bowel resection and ileostomy. |
Abdomen |
46 |
M |
Failure respiratory, adenocarcinoma in gastric cardia and metastasis in liver and trachea. Aortic aneurysm. |
Tracheostomy and gastrostomy tube installation. |
Neck and abdomen |
47 |
F |
Ectopic pregnancy, hypovolemic shock |
Left Salpingectomy |
Pelvis |
48 |
F |
Appendicitis stage III |
Appendectomy |
Abdomen |
49 |
F |
Appendicitis stage IV |
Appendectomy |
Abdomen |
50 |
F |
Appendicitis stage I |
Appendectomy |
Abdomen |
51 |
M |
Trauma in pelvis, rectum and coccyx. |
Fragment removing of coccyx, rectum exploration, washing, drainage, colostomy, and pelvis external fixation. |
Rectum |
52 |
F |
Abdominal sepsis. 9 days in the postoperative for Perforated duodenal ulcer. |
Duodenostomy and jejunostomy |
Abdomen |
53 |
F |
Ischemic colitis |
Left hemicolectomy, colostomy |
Abdomen |
54 |
M |
Duodenal perforated ulcer |
Primary closure of the duodenum, omental patch. |
Abdomen |
55 |
F |
Hidrocolecisto |
Laparoscopic cholecystectomy |
Abdomen |
56 |
M |
Sigmoid volvulus |
Sigmoidectomy, colostomy |
Abdomen |
57 |
M |
Pleural effusion |
Catheter placement |
Thorax |
58 |
M |
Abdominal sepsis, appendicitis. |
Laparotomy, abscess drainage |
Abdomen |
59 |
M |
Pyocolecystits, gallbladder perforated, thrombocytopenia, bleeding. |
Open cholecystectomy, abdominal packing. |
Abdomen |
60 |
F |
Intestinal occlusion |
Release of internal abdominal hernia |
Abdomen |
61 |
M |
Dysfunctional Tenckoff catheter |
Catheter removal |
Abdomen |
62 |
M |
Abdominal wall abscess |
Abscess drainage, new Tenckhoff catheter placement |
Abdominal wall |
63 |
M |
Metabolic acidosis, Renal failure |
Tenckhoff catheter placement |
Abdomen |
64 |
M |
Prolonged intubation, hyperosmolar state, urinary retention. |
Tracheostomy, cystostomy |
Neck, urinary tract |
65 |
F |
Acute abdominal pain |
Laparotomy, lyses of adherents, prophylactic appendectomy, inflammatory pelvic disease. |
Abdomen |
66 |
F |
Hypovolemic shock |
Laparotomy, broken pelvic pregnant. |
Abdomen |
67 |
M |
Acute abdominal pain |
Laparoscopic appendectomy phase IV |
Abdomen |
68 |
M |
Skin ulcers on the back |
Surgical cleaning |
Soft tissue |
69 |
F |
Acute abdominal pain |
Laparoscopic appendectomy phase I, Inflammatory Pelvic disease. |
Abdomen |
70 |
F |
Dysfunctional Tenkoff catheter |
Tenckhoff Catheter removing |
Abdomen |
71 |
M |
Acute cholecystitis |
Laparoscopic endoscopic cholecistectomy |
Abdomen |
72 |
M |
Knife penetrating abdominal injury |
Endoscopic suture of gastric wall. |
Abdomen Trauma |
73 |
M |
Abdominal acute pain |
Endoscopic appendectomy, phase IV |
Abdomen |
74 |
M |
Abdominal acute pain |
Endoscopic appendectomy phase IV |
Abdomen |
75 |
M |
Hypovolemic shock |
Laparotomy, suture of gastric ulcer |
Abdomen |
76 |
F |
Acute Cholecystitis |
Laparoscopic cholecystectomy |
Abdomen |
77 |
F |
Appendicitis |
Laparoscopic appendectomy |
Abdomen |
Table 3: 77 cases with preoperative diagnosis and intraoperative findings.
7 years later of this project, mobile phones are one of the meanly tools for surgeons as the rest of physicians in the world. Mobile phones resolutions and many Apps give the surgeon a potential and remarkable surgical tool to improve communication in surgery. Telemedicine with Smartphone for emergences surgery is not an invasive procedure that helps all surgical team involved to avoid lost time in the preparation of surgical but meanly anesthesiologist equipment organization. In the present project we demonstrate with 77 cases that smart phones reduce time in organization anesthesiologist and surgical instruments in the preoperative. Telemedicine with smart phones are a complementary tool in the communication between surgical team, easy to use and carry, lighter, and fast to send medical data and pictures. The meanly advantages with mobile phones is for prepare at time medications, tools for anesthesia and surgical instruments thereby improving the quality of service. This application could be better in 2011 if we can get access in Wi Fi in our service in the hospital to send via internet all information avoiding delay in sending messages in traffic time. Videos are heavy and difficult information to send by phone service and internet, in that year (2011) the only smart phone that has this service was expensive and didn´t permit us our proposal. There was another way where society shares information, such as; social networking services, face book, twitter, etc. I don´t suggest social networking for Telemedicine applications in our society for the following reasons, image of patients, file numbers, personal data are private information for exclusive use for Medicine only and could be the possibility to be used by other different interests as criminals from organized crime rising every day in Mexico. Telemedicine in 2017 with mobile phones for emergence service currently is because is so fast to send information and we can prepare on time patients for operating rooms. Up today patients can communicate with relatives in the recovery with video skype. Videoconferences App in real time in smart phones are the future for Telemedicine. In future works, we´ll need analyze the surgical time in each patient and the kind of surgery to demonstrate if arranging surgical team is possible to reduce the time of emergence surgery sending medical data and images by mobile phones. 7 years later, smartphones have demonstrated that is more than a phone, more than a computer and has transformed a powerful medical tool for the pocket for surgeons for Telemedicine. Up today 2021 we are living global pandemic by SARS II, Covid.19. Smartphones is the meanly tool for medical communications among relatives and with physicians. Videonference as Zoom applications is the must use too. 10 years ago, smartphones began to demonstrate the potential today they have in medicine. Brain computer interphase in the following years will change much more the culture of humankind communication because brain implants could be placed in the cortex or midbrain for no wiring global communication using just brain Internet.
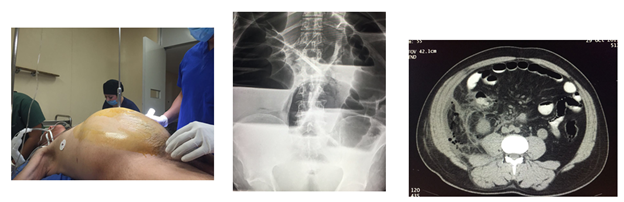
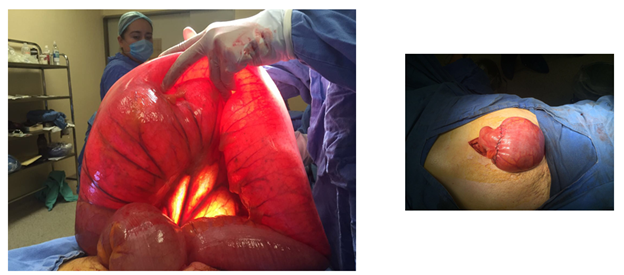
Case 17 (iPhone G3 A1324). July 2011. Text message: Male, 54 age, 21 days of evolution with abdominal distention, vomiting, diarrhea, and intense thirst for dehydration. Laboratory: leukocytes 1000, hemoglobin 10.2, glucose 60, creatinine 5. See picture 1, patient abdomen distended, abdomen X Rays and scanner CT. Picture 2: Intraoperative findings.
Picture 1: Preoperative. Patient´s abdomen and X Rays with iPhone G3 A1324.

Picture 2: Intraoperative. Sigmoid volvulus with iPhone G3 A1324.
October 28, 2017. Text message: Male of 70 of age, 15 days of evolution with abdominal distention and pain, and thirst for dehydration. Laboratory: leukocytes 13400, hemoglobin 16.5, glucose 142. Creatinine 0.8 (Picture 3 and 4 made with iPhone 6s).
Picture 3: Preoperative. Patient´s abdomen, abdomen X Rays and scanner CT with iPhone 6s.
Picture 4: Intraoperative. Sigmoid volvulus and end to end colo-colo anastomosis. Picture made with iPhone 6s.
Citation: José Luis Mosso Vázquez and Enrique Jesús Rodriguez. "Smartphones in 2011 for Telemedicine in Emergency Surgery and 7 Years Later". Acta Scientific Gastrointestinal Disorders 4.4 (2021): 03-11.
Copyright: © 2021 José Luis Mosso Vázquez and Enrique Jesús Rodriguez. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.