Shikha Khare1*, Karthikeya Patil2 and Mahima VG3
1Masters in Dental Surgery, PG Student, Department of Oral Medicine and
Radiology, JSS Dental College and Hospital, JSS Academy of Higher Education and
Research, Karnataka, India
2Masters in Dental Surgery, Professor and HOD, Department of Oral Medicine and
Radiology, JSS Dental College and Hospital, JSS Academy of Higher Education and
Research, Karnataka, India
3Masters in Dental Surgery, Professor, Department of Oral Medicine and Radiology,
JSS Dental College and Hospital, JSS Academy of Higher Education and Research,
Karnataka, India
*Corresponding Author: Shikha Khare, Masters in Dental Surgery, PG Student, Department of Oral Medicine and Radiology, JSS Dental College and Hospital, JSS Academy of Higher Education and Research, Karnataka, India.
Received: January 12, 2021; Published: February 16, 2021
Purpose: Craniofacial asymmetry is rarely appreciable and is often unnoticed, but it is often a cause of major diagnostic difficulties in orthodontics. Currently, no clear universally accepted method exists for the evaluation of craniofacial asymmetries therefore different methods are utilised to determine midline and evaluate asymmetry. This study was conducted to compare the reliability and validity of two different methods for cranial midline localization through cephalometric analysis of mandibular condylar asymmetries.
Materials and Methods: Craniostat ear rods and foramen spinosum were considered as initial landmarks in tracing 1 and tracing 2 respectively. Quantification of Condylar Asymmetry was performed by calculating bilateral condylar width, condylar angle, intracondylar hemidistance and extracondylar hemidistance on each tracing. Descriptive analysis and paired t-test for independent samples were performed with SPSS software for windows.
Results: No significant difference was found on comparative analyses of difference in symmetry ratios between the two methods for the determination of craniofacial asymmetry.
Conclusion: Craniostat ear rods, as well as foramen spinosum, are both suitable markers for tracing the reference cranial midline for assessment of condylar asymmetry with neither being more reliable or suitable than the other in the representative adult population.
Keywords: Orthognathic Surgery; Mandibular Condyle; Facial Asymmetry; Skull Base
A small degree of craniofacial asymmetry is always present in all subjects with normal biometric parameters [1]. Although, unlike major facial deformities typically associated with various syndromes, this asymmetry is rarely appreciable and is often unnoticed, but it frequently renders major diagnostic difficulties in orthodontics. Diagnosis and localization of asymmetry could be vital for treatment planning and act as an indicator of prognosis for orthognathodontics [2]. Furthermore, prior to combined orthodontic/orthognathic surgery, skull radiographs are recommended to evaluate pre-existing temporomandibular pathologies in the patients for diagnosis and prevention of joint disorders that could heavily influence the postsurgical function. Anatomically, altered condylar position and bone degeneration (osteoarthrosis) are often associated with jaw discrepancies/malocclusion which should be detected and quantified to optimize the pre-treatment diagnosis and post-treatment follow-up [3]. The submentovertex (SMV) radiograph gives an immediate localization and quantification of condylar asymmetries and the visualization of other facial and mandibular structures that could be involved in the craniofacial asymmetry [4].
The key to evaluating asymmetries is defining the criteria to determine the cranial midline. Currently, there is no clear, universally accepted method for the evaluation of craniofacial asymmetries and therefore different procedures are used to identify the ideal midline.
In context to the above preamble, this study was undertaken to compare the reliability and validity of two different methods of cranial midline localization through cephalometric analysis of mandibular condylar asymmetries. The objective of this study was to aid in planning treatment and evaluating the results of orthognathodontics or maxillofacial surgery.
The study group comprised of 20 subjects who reported to the Department of Oral Medicine and Radiology, JSS Dental College and Hospital as out-patients. Purposive sampling included the patients which required submentovertex radiograph for their orthognathic surgery or minor oral surgery. This sampling method ensured that the patients are not additionally exposed to radiation for the purpose of this study. Radiographs were obtained with SMV projection by a single operator to reduce interoperator bias during the positioning of the patient.
Inclusion criteria
Exclusion criteria
Two different cephalometric analyses were chosen to trace the basicranium midline for the localisation of midline. In tracing 1 craniostat ear rods were considered as initial landmarks. The straight line connecting the tip of the left and right ear rods passes through the left and right midpoint of the external acoustic meatus forming transporionic axis (TPA). The cranial midline/median sagittal plane (MSP) was established by tracing a perpendicular line crossing the midpoint of the TPA as shown in figure 1. In tracing 2 foramina spinosum (FS) were used as main landmarks to identify the axis of symmetry. The outlines of the FS were identified on the radiographs, and the straight line passing through the centre of the left and right FS was traced to obtain trans-spinosum axis (TSA). A second line that passes through the midpoint of the TSA was considered to be the MSP as shown in figure 2. All radiographic tracings and measurements were done digitally using Romexis software.
The medial and lateral poles for bilateral mandibular condyles were identified and quantification of the asymmetry was performed using eight parameters each for tracing 1 and 2 on a digital submentovertex radiograph. The parameters quantified for assessment include:

Figure 1: Radiograph showing measurement of the condylar width as the distance between the medial and lateral pole on tracing 1 taking transporionic axis (TPA) as reference. A- Right condylar width; B- Left condylar width.

Figure 2: In tracing 2 the straight line passing through the centre of the left and right Foramina Spinosum was traced to obtain trans-spinosum axis (TSA). A second line that passes through the midpoint of the TSA was considered to be the midsagittal plane.

Figure 3: Radiograph showing measurement of condylar angle on tracing 1 taking transporionic axis as reference. Condylar angle is formed by the straight line passing through the condylar poles and the straight line perpendicular to the midline. A- right condylar angle; B- left condylar angle.
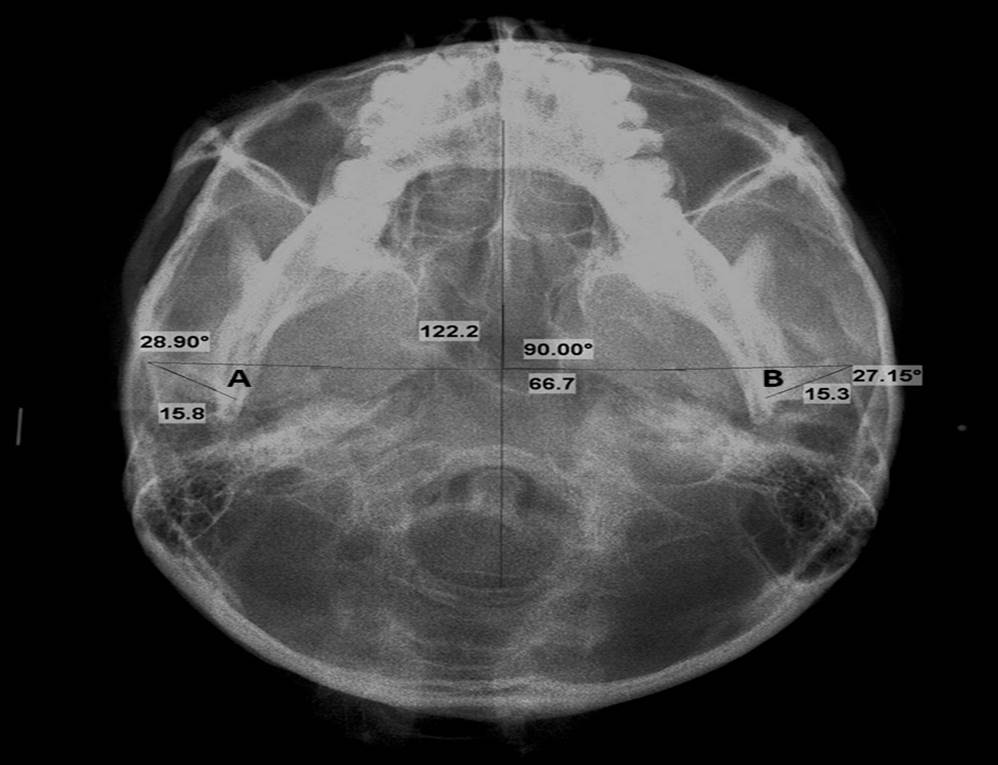
Figure 4: Radiograph showing measurement of condylar angle on tracing 2 taking trans-spinosum axis as reference. Condylar angle is formed by the straight line passing through the condylar poles and the straight line perpendicular to the midline. A- right condylar angle; B- left condylar angle.

Figure 5: Radiograph showing measurement of bilateral intracondylar and extracondylar hemidistance on tracing 1 taking transporionic axis as reference. A- Intracondylar hemidistance; B-Extracondylar hemidistance.

Figure 6: Radiograph showing measurement of bilateral intracondylar and extracondylar hemidistance on tracing 2 taking trans-spinosum axis as reference. A- Intracondylar hemidistance; B-Extracondylar hemidistance.
The symmetry ratio (SR) was calculated for Tracing 1 (Table 1) and Tracing 2 (Table 2) individually using the left side measurement as a reference by the formula: SR = Left parameter/Right parameter. An SR value of more than 1 indicates that the left side is larger than the right side, an SR value of less than 1 suggests that the right side is greater than the left and an SR value equals to 1 indicates perfect symmetry.
| Mean | Standard deviation | Symmetry Ratio | |
|---|---|---|---|
Left condylar width |
14.3 |
1.02 |
1.0 ± 0.02 |
Right condylar width |
14.25 |
0.91 |
|
Left condylar angle |
26.48 |
3.15 |
0.96 ± 0.16 |
Right condylar angle |
28.16 |
5.05 |
|
Left intracondylar hemidistance |
42.51 |
5.62 |
0.97 ± 0.09 |
Right intracondylar hemidistance |
43.90 |
6.58 |
|
Left extracondylar hemidistance |
53.75 |
6.41 |
0.99 ± 0.08 |
Right extracondylar hemidistance |
54.67 |
7.31 |
Table 1: Statistical analysis of all parameters on tracing 1 (using ear rods as reference).
| Parameters | Mean | Standard deviation | Symmetry Ratio |
|---|---|---|---|
Left condylar width |
14.3 |
1.02 |
1.0 ± 0.02 |
Right condylar width |
14.25 |
0.91 |
|
Left condylar angle |
26.94 |
3.08 |
0.98 ± 0.14 |
Right condylar angle |
27.93 |
4.69 |
|
Left intracondylar hemidistance |
43.17 |
5.84 |
1.0 ± 0.09 |
Right intracondylar hemidistance |
43.05 |
6.11 |
|
Left extracondylar hemidistance |
53.70 |
6.42 |
1.0 ± 0.01 |
Right extracondylar hemidistance |
53.72 |
6.60 |
Table 2: Statistical analysis of all parameters on tracing 2 (using foramen spinosum as reference).
Statistical analyses were performed to compare each quantifying parameter on tracing 1 to the same on tracing 2. (Table 3, Figure 7) Statistical significance was also calculated for difference in the symmetry ratio between tracing 1 and 2 for the condylar angle, intracondylar hemidistance and extracondylar hemidistance individually. Descriptive analysis of the entire sample and paired t-test for independent samples were performed with the SPSS software for windows.
| Parameters | Mean | Std. Deviation | p-value |
Left condylar angle |
-.46400 |
2.02041 |
0.317 |
Right condylar angle |
.22650 |
2.93051 |
0.733 |
Left intracondylar hemidistance |
-.65850 |
1.81754 |
0.122 |
Right intracondylar hemidistance |
.84950 |
1.93055 |
0.064 |
Left extracondylar hemidistance |
.05200 |
2.85709 |
0.936 |
Right extracondylar hemidistance |
.95100 |
2.44046 |
0.098 |
Table 3: Comparision of each parameter from tracing 1 and tracing 2.

Figure 7: Bar diagram showing comparision of each parameter from tracing 1 and tracing 2.
The total sample consisted of 65% males (13) and 35% females (7) with an overall mean age of 32.65 years. There was no significant correlation of data with age or gender.
None of the 8 parameters as discussed earlier showed a significant difference in quantification by tracing 1 or tracing 2. Symmetry ratio of condylar angle, intracondylar hemidistance and extracondylar hemidistance as analysed on tracing 1 (considering craniostat ear rods as a landmark) was less than 1, indicating a greater dimension of the right cranial base than its left counterpart. On the other hand, tracing 2 (considering foramen spinosum as the landmark) depicted a symmetry ratio of 1 for intra and extra condylar hemidistance indicating perfect symmetry. The symmetry ratio of condylar angle in tracing 2 was less than 1, similar to tracing 1. However, the comparative analyses of difference in symmetry ratios as calculated using tracing 1 and 2 was not statistically significant and depicted similar findings (Table 4).
| Symmetry ratio | Mean | Std. Deviation | p-value |
Condylar angle |
-.02027 |
.05309 |
.104 |
Intracondylar hemidistance |
-.03296 |
.07631 |
.068 |
Extracondylar hemidistance |
-.01465 |
.06701 |
.340 |
Table 4: Comparing the symmetry ratios obtained from tracing 1 and tracing 2.
The submentovertex radiograph represents a useful method to examine the cranial base for the quantification of asymmetry of the anatomic structures. Visualisation of the axial plane at the cranial base is more useful than other skull radiographs to determine the midsagittal axis [5].
However, SMV is two-dimensional imaging modality and the advent of three-dimensional radiographic techniques like cone-beam computed tomography have changed the potential in pre-surgical diagnosis and pre-treatment planning. Nevertheless, the digital two-dimensional skull radiograph remains the modality of choice for the major diagnostic challenges in clinical practice due to its ease of execution, low radiation exposure dose, and the good spatial resolution [6].
The central area of the external cranial base including Foramina Spinosum reaches its maximum dimension at the age of 4-5 years and thereafter preserves its morphology throughout life [7]. The masticatory function, facial trauma, and orthognathodontic therapy will influence the development of temporal bones but not the position of the neurovascular foramina [4]. It should also be underlined that the possibility of head rotation during the positioning of the patient and a subsequent image distortion with misinterpretation of the results cannot be ruled out [8]. It highlights the inaccuracy of ear rods as reference points for the determination of midline asymmetry, whereas the bony landmark remains unaltered. Furthermore, the positioning of the ear rods in the acoustic external meatus could be influenced by the operator’s skill and precision.
Therefore, the foramina spinosum represent the most reliable tracing point in basilar view as it is a fixed bony landmark which makes it reproducible and free of positioning errors. However, in this study, no significant difference was found between two methods for determination of asymmetry.
Michele Maglione and Fulvia Costantinides in a similar study found that the difference between the SRs obtained with the two different tracings was statistically insignificant for the adult population but if the analysis of condylar asymmetries is performed in growing subjects, utilization of anatomic references such as the foramina spinosum seems to guarantee a lower error compared to non-fixed references such as ear rods [4].
Another relevant study by Ashutosh Kumar Singh., et al. [9] also failed to validate the hypothesis indicating that the midline traced with spinosum foramina as reference landmark approximates the ideal midsagittal more closely than craniostat ear rods. Statistical analysis of the results showed substantial equivalence and reliability of both tracing methods used.
In the current study, statistical analysis revealed the substantial equivalence and reliability of both the tracing methods which results from the fact that the left/right discrepancy for Tracing 1 and 2 is not statistically significant. Therefore, it can be concluded that both craniostat ear rods, as well as foramen spinosum, are suitable markers for tracing the reference cranial midline for assessment of condylar asymmetry with neither being more reliable or suitable than the other in the representative adult population. However, another study on adult, as well as a growing population, should be conducted with a bigger sample size before rejecting or accepting this hypothesis.
Citation: Shikha Khare., et al.“Localization of Basicranium Midline by Submentovertex Projection for the Evaluation of Condylar Asymmetry Using Craniostat Ear Rods and Foramen Spinosum as Reference".Acta Scientific Dental Sciences 5.3 (2021): 64-70.
Copyright: © 2021 Shikha Khare., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.