Kulvinder Kochar Kaur*
Scientific Director, Dr Kulvinder Kaur Centre for Human Reproduction, Jalandhar, Punjab, India
*Corresponding Author: Kulvinder Kochar Kaur, Scientific Director, Dr Kulvinder Kaur Centre for Human Reproduction, Jalandhar, Punjab, India.
Received:September 19, 2024; Published: October 25, 2024
Citation: Kulvinder Kochar Kaur. “Reemphasizing the Significance of Fertility Preservation in Cancer Patients Needing Chemotherapy and/or Radiotherapy - A Case Report". Acta Scientific Women's Health 6.11 (2024): 70-74.
With the greater advancements in field of cancer treatment, the survival rates have escalated remarkably, thus the need arising for the fertility preservation in the survivors with regards to oocyte/embryo/ovarian tissue/Cortical tissue/testicular tissue transplantation/sperm cryopreservation has assumed great importance particularly for those receiving chemotherapy that too with alkylating agents. Earlier we have extensively detailed however still we come across akin patients who never received any counselling keeping longterm fertility in mind. The case report we present here highlights this issue. Here we present a case report of how a couple presented With a previous child having diagnosis of type II Arnold Chiari malformations. Later husband gave history of certain axillary mass which was surgically removed in addition to got chemotherapyx 6 cycles and radiotherapy for4 cycles although the nature of chemotherapy was not known he later told diagnosis was non Hodgkin’s lymphoma. Despite his semen parameters were normal 10 years subsequent to chemotherapy and radiotherapy couple was not willing to go for Intracytoplasmic sperm injection (ICSI) with blastocyst transfer subsequent to preimplantation embryo genetic testing (PGT) for aneuploidy (PGT-A), and particular congenital abnormalities. Thereby here we re emphasize the role of counselling for sperm cryopreservationor testicular tissue preservation as per age prior to administration of chemotherapy and radiotherapy for cancer treatment.
Keywords: Cancer Treatment; Counselling; Fertility Preservation
With the greater advancements in field of cancer treatment, the survival rates have escalated remarkably, thus the need arising for fertility preservation in the survivors with regards to cryopreservation of oocyte/embryo/ovarian tissue/Cortical tissue/testicular tissue transplantation/sperm cryopreservation has assumed great importance particularly for those receiving chemotherapy specifically with alkylating agents. Furthermore, the need further is enhanced in younger adults along with adolescents diagnosed as cancer and need chemotherapy and are yet to attain puberty where cryopreservation of oocytes might not be feasible. However even in adult cases how it has become substantially significant for all clinical practitioners tackling cancer patients to emphasize the significance of counselling both male and female patients prior to initiation of chemotherapy/radiotherapy to get either cryopreservation of sperm/oocyte before initiating chemotherapy/radiotherapy. We have made numerous publications regarding this issue, however still we come across akin patients who never received any counselling keeping longterm fertility in mind. The case report we present here highlights this issue. now was
A couple came to our centre on 11/2/2023 with the history of being married for 9 yrs and previously having a pregnancy antenatally with a diagnosis of type II Arnold Chiari malformations, which resulted in performance of a MTP. Currently age of wife is 40 yrs; with that of husband being 37 yrs. On in depth probing we got the history of husband obtaining treatment for certain axillary mass which was surgically removed in addition to received 6 cycles of chemotherapy and4 cycles of radiotherapy although the nature of chemotherapy was not known he later divulged diagnosis was non Hodgkin’s lymphoma. This had been done 10yrs previously. Now they had come for counselling for subsequent pregnancy in addition to chances for a normal child (without any congenital abnormalities). His RSA displayed a semen count of 70m/ml, with apparently normal morphology in 70%. Taking into account there being a history of both chemotherapy along with radiotherapy receipt we counselled her for Intracytoplasmic sperm injection (ICSI) in addition to preimplantation genetic testing (PGT) for aneuploidy (PGT-A) prior to embryo transfer (ET) once normal PGT report was attained however the couple were not willing to attribute this problem to chemotherapy along with radiotherapy and normal RSA they wanted simpler approach. Earlier we had reported innumerable reviews on fertility preservation in both male and female cancer therapy with chemotherapy particular alkylating agents along with considerable research getting performed even in young children in addition to adolescents who have not attained puberty along with any treating physician needs to refer these cases for counselling for fertility preservation as per age either gametes/testicular/ovarian cortical tissue/testicular tissue transplantation [1-5] later was.
Gonadotoxic actione and the duration taken for sperm recovery subsequent to radiotherapy based apart from initial semen quality, but further on gonadal dosage and the administration methodology subsequent to after chemotherapy, regimens kinds and dosages and on the spermatogenesis phase that each drug affects. Combination treatment with radiotherapy and chemotherapy will induce more gonadotoxicity than either modality alone. Although efforts to prevent gonadal toxicity in cancer treatment are routinely applied, sperm cryopreservation remains the gold standard to maintain male fertility after cancer survival [6].
Despite sperm banking prior to initiation of cancer treatment is recommended, conditions might be there that prevent the successful cryopreservation of sperm in personalized patients. The restoration of spermatogenesis subsequent to chemotherapy or radiotherapy is acknowledged to be unanticipable as well as studies of spermatogenesis in long-term cancer survivors have illustrated corroboration of continuation of azoospermia or robust oligospermia in approximately 24% of cases. However, the ultimate resumption of sperm generation in plethora of posttherapy cancer patients incites the query of posttreatment safety of sperm utilized in natural or assisted reproductive technologies (ART) on contemplating conception. Choy., et al. [7], assessed this problem of reproductive safety and the risks of utilizing sperm from cancer patients.
In reference to these both erations over reproductive safety are basically based in the plausible existence of DNA injury stimulated by the germ line chemotherapy or radiotherapy. Chemotherapeutic agents, specifically the alkylating agents which get commonly utilized, might stimulate genetic injury by cross-linking DNA along with introducing single-strand DNA breaks; the akin mutagenic actions of radiation originating from DNA fragmentation evoked within cells [2,7]. The estimation of genetic safety depends largely on the spermatogenic stage at which a mutation is attained. In view of down-regulation of DNA repair mechanistic modes which take place in late spermatogenesis, spermatogenic cells further along the differentiation pathway canonically do not possess the capacity of repair DNA injury, nor do they possess the capacity generally of going via total apoptosis [8]. Thereby the ejaculated spermatozoa might foster substantial genomic injury which theoretically might get transmitted to a resultant embryo subsequent to fertilization. Fortunately, mutations that stimulate sole stages of spermatogenesis would provide a risk period for the generation of genetically endangered sperm that is restricted to approximately 3 months/the time taken for a full spermatogenic cycle to finish [8]. Conversely, mutations suffered by the spermatogonial stem cells possess the capacity of plausibly healed by inherent DNA repair mechanistic modes or entirely eliminated by the cell's apoptotic machinery. Nevertheless, since these spermatogonial cells which portray the progenitors from which all future germ lines get obtained, any sustenance of mutations in these cells dodge repair or depletion will persistently get transmitted, resulting in the plausible generation of mutation-carrying sperm for the full time period of a man's lifetime [8].
There is a scarcity of peer-reviewed literature in reference to reproductive results in the acute, posttreatment duration of time. These studies are clearly restricted in view of ethical along with the practical botherations. Existing studies implicating humans are usually largely removed from the acute, posttreatment time frame, and they previously canonically typically conclude that the frequency of congenital anomalies in the children of men earlier having exposure to chemotherapeutic agents is not more compared to that observed among the general population [7]. Nevertheless, case studies of men who have managed to conceive subsequent to cancer therapy continue to corroborate the plausibility of an association between cancer therapy as well as congenital anomalies in humans, since instances of resultant syndactyly, tetralogy of Fallot, in addition to anencephaly have been revealed [9].
Further Meistrich ML. [10] reviewed the actions of chemotherapy as well as radiotherapy on spermatogenesis in humans.
They described the i)Course of how sperm decrease takes place (Figure 1) see ref no 10 for details.
![Figure 1: Courtesy reference no-10-Sequence, kinetics, and survival after irradiation of spermatogenic cells in the human male. Drawings cells courtesy of Dr. Y Clermont. Arrows indicate time required for cells to mature from one state to another. Numbers in parentheses are based on histological counts of the surviving fraction of cells at 2 weeks after 1 Gy of irradiation, reflecting the direct killing of cells by irradiation and 2 weeks of maturation depletion [3].](https://actascientific.com/ASWH/images/ASWH-06-0634_figure1.png)
Figure 1: Courtesy reference no-10-Sequence, kinetics, and survival after irradiation of spermatogenic cells in the human male. Drawings cells courtesy of Dr. Y Clermont. Arrows indicate time required for cells to mature from one state to another. Numbers in parentheses are based on histological counts of the surviving fraction of cells at 2 weeks after 1 Gy of irradiation, reflecting the direct killing of cells by irradiation and 2 weeks of maturation depletion [3].
Furthermore how does sperm recovery occurs subsequent to chemotherapy or radiotherapy (Figure 2)- displays different chemotherapies used and their effect for instance in Hodgkin’s lymphoma use of vincristine/vinblastine as well as prednisolone -their impact on sperm recovery against mitoxantrone
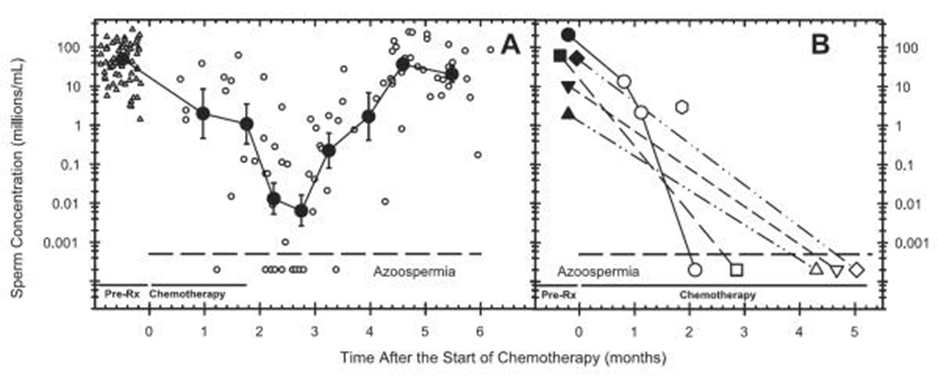
Figure 2: Courtesy reference no-109-Declines in sperm counts in patients treated with two different chemotherapy regimens. (A) NOVP (9) chemotherapy consisting of Novantrone (mitoxantrone), Oncovin (vincristine), vinblastine, and prednisone for Hodgkin's disease. Small open circles are individual sperm counts. Large filled circles are averages of counts grouped into time ranges. (Reprinted with permission from Meistrich et al., Journal of Clinical Oncology 15: 3488, 1997) The subsequent recovery of sperm counts to normal levels is also shown. (B) CY (V) ADIC (8) chemotherapy consisting of cyclophosphamide, Adriamycin (doxorubicin), DIC (DTIC, dacarbazine), with or without vincristine for Ewing and soft-tissue sarcoma. Pretreatment counts are indicated by solid symbols. Dashed lines connect longitudinal counts for individual patients. (Reprinted with permission from Meistrich., et al. Cancer 70: 2703, 1992.
Then actions of radiotherapy (see Figure 3).
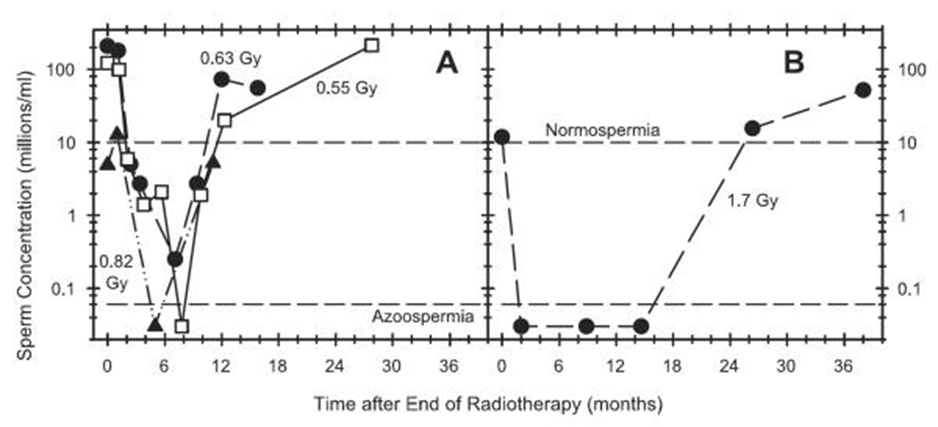
Figure 3: Courtesy reference no-9-Recovery of sperm counts in individual patients treated with (A) hemi-pelvic radiotherapy for seminoma (22, 23), or (B) pelvic radiotherapy for Hodgkin's disease (24). Gonadal doses are indicated next to each plot.
Further delayed recovery might occur with actions of variable cytotoxic agents. The article describes in detail why azoospermia occurs/how if stem cells injured how it impacts see reference 6 for details of a variety of cytotoxic agents and radiotherapy

Figure 4: Courtesy reference no-10- (A) Examples of delayed recovery of sperm count occurring after 2 to 5 years of azoospermia in 5 patients treated with chemotherapy agents that are toxic to stem spermatogonia. (◯, ●) CVPP-ABDIC consisting of cyclophosphamide, vincristine, procarbazine, prednisone, Adriamycin, bleomycin, dacarbazine, and lomustine (CCNU) (26) treatment for Hodgkin's disease patients; (▲) CHOP-Bleo which consists of cyclophosphamide, Adriamycin (hydroxydaunorubicin), Oncovin, prednisone, and bleomycin (27) treatment for a non-Hodgkin's lymphoma. (B) Kaplan-Meier actuarial estimation of sperm count recovery to 10 million/ml showing the overall rates and extents of recovery in sarcoma patients were treated with the CY (V) ADIC regimen, but receiving different total doses of cyclophosphamide (8) (Reprinted with permission from Meistrich., et al. Cancer 70: 2703, 1992).
Thereby our patient received the usual drugs for non Hodgkin’s lymphoma probably in addition to radiotherapy as well as although normal RSA as explained by Choy JT, Brannigan RE their child suffered from type II Arnold Chiari malformations which adds to the list of congenital anomalies earlier documented in the aftermath of receiving chemotherapy and radiotherapy, thereby emphasizing on cryopreservation prior to any chemotherapy and radiotherapy to avoid such effects on the gametes and documentation of these congenital anomalies is significant for convincing the patients in addition to treating clinical practitioners. This further highlights how much normal general physicians (GP’s), any family physicians/clinical practitioners/oncologists need to be hammered that counselling for cryopreservation is significant before any chemotherapy and radiotherapy is planned both from point of view of future fertility, [11-14] so much so that while writing one of the articles on fertility preservation in men the reviewer asked so much knowledge exists what is the point of more and my answer was still all cases we encounter yet have not received counselling or no tissue cryopreserved, thus it has become empirical to use tv ads to even make public more aware and themselves start asking as so much failure by practitioners in implementation.
Copyright: © 2024 Kulvinder Kochar Kaur. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.