Mastewal Mulu1, Mebratu Kebede2*, Demise Asegu Fenta1, Kirubel Tinsae1, Fantahun Belay1 and Adanech Shiferaw1
1Department of Anesthesia, Hawasa University, Hawasa, Ethiopia
2School of Anesthesia, Wolaita Soddo University, Wolaita Soddo, Ethiopia
*Corresponding Author: Mebratu Kebede, School of Anesthesia, Wolaita Soddo University, Wolaita Soddo, Ethiopia.
Received:October 03, 2024;; Published: October 25, 2024
Citation: Mebratu Kebede. “Incidence and Predictors of Delirium among Patients Admitted to Intensive Care Unit in Selected Teaching Hospitals of Southern Ethiopia: Malti Center Prospective Observational Study". Acta Scientific Women's Health 6.11 (2024): 29-39.
Background: Delirium is an acute cognitive impairment or fluctuating concentration. It is a common organ dysfunction among critical patients in the intensive care unit that affects up to 87% of patients. It is strongly linked to increased mortality and morbidity. Objective: The objective of this study was to assess the incidence and predictors of delirium among patients admitted to intensive care units in selected teaching hospitals in southern Ethiopia, January 15-April 15, 2024.
Methods: A multicenter prospective observational study was conducted at selected Teaching hospitals in southern Ethiopia. The study enrolled 182 consecutive patients. The Confusion Assessment Method for the Intensive Care Unit to assess delirium and the Richmond Agitation Sedation Scale for assessment of the level of sedation and delirium subtypes were used. After the data was checked, cleared, and coded, the entry and analysis were employed using version 26 of SPSS software. Texts, tables, and graphs were used for data presentations. Binary logistic regression was used to see the association between each independent variable and the dependent variable. A variable with a p-value less than 0.25 in binary logistic regression was entered into multivariable logistic regression for adjustments. The adjusted odds ratio was used with a 95% CI to see the strength of the associations. Variables with a P-value less than 0.05 in multivariate logistic regression were considered statistically significant.
Result: the cumulative incidence of delirium is 30.8 % (95% CI 24.7–35.8%). On multivariate logistic regression, being single (AOR 5.560, CI: 1.844-16.765, p = 0.002), smoking (AOR 4.480, CI: 1.496-13.418, p = 0.007), alcohol use (AOR 4.850, CI: 1.780-13.217, p = 0.002), and sedation with propofol (AOR 3.776, CI: 1.265-11.275, p = 0.017) have a significant association with delirium.
Conclusion: cumulative incidence of delirium is 30.8% and Being single, smoking, alcohol usage, and propofol have significant association with delirium. It is crucial to assess and identify the incidence and risk factors of delirium for prevention and early management.
Keywords: Critical Patients; Delirium; Incidence; Risk Factor; Intensive Care Unit
AOR: Adjusted Odds Ratio; CAM: Confusion Assessment Methods; CAM-ICU: Confusion Assessment Methods for Intensive Care Unit; CI: Confidence Interval; COR: Crud Odds Ratio; HUSCH: Hawassa University Comprehensive Specialized Hospital; ICU: Intensive Care Unit; IQCODE: Informant Questionnaire on Cognitive Decline; LOS: Length of Stay; MSOFA: Modified Sequential Organ Failure Assessment score; NEMMCSH: Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital; RASS: Richmond Agitation Sedation Score; WSCH: Worabe Comprehensive and Specialized Hospitalital; WSSH: Wolyta Sodo Specialized Hospital
Delirium is a short-term disturbance in attention (the top mandatory feature) that is associated with cognitive functions [1]. It is also termed a transient condition of altered attention and consciousness [2]. It manifests as a sudden change in the patient's mental state, a lack of focus, disorientation when thinking, and cognitive failure [3]. It is a syndrome of several different etiologies and diseases with systemic involvement and is associated with a rapid decline in brain function [4].
The overall incidence is as high as 87% [5]. In Europe, the incidence ranges from 21.8% to 42% [6-8]. The incidence of ICU delirium in different Arabian countries ranges from 14.5%–33% [5,9-11]. In China and other Southeast Asian countries, it is about 22.2%–36.1% (4, 12, 13). ICU delirium is also relatively high in Ethiopia. As the study at St. Paul's Hospital Millennium Medical College showed, among delirious hospitalized patients, 36.4% were ICU patients [14].
Delirium in the ICU is caused by patient-related (predisposing) and precipitating or ICU environment-related risk factors. It commonly occurs due to the high degree of disease severity, age of the patients, mechanical ventilator use, sedative medication use, and other environmental factors like physical restraint use [15,16].
It has a strong correlation with several negative patient outcomes, such as increased rates of mortality and morbidity, longer periods of mechanical ventilation in the ICU, longer hospital stays, recurrent hospital admissions, both short- and long-term cognitive impairment, and increased medical expenses [13,17,18]. It is also a strong independent indicator of mortality [19].
Despite the different pharmacological and non-pharmacological interventions recommended previously, delirium in the ICU remains higher in developed countries. Since information is scarce, very little is known about the incidence of delirium, particularly in critically ill patients admitted to the ICU in Ethiopia. This study aimed to assess the incidence and associated factors of delirium among patients admitted to the intensive care units in teaching hospitals of southern Ethiopia.
This multicenter prospective observational study was carried out from January 15 to April 15, 2024, in four selected teaching hospitals of southern Ethiopia: Wolaita Sodo University Comprehensive Specialized Hospital, Worabe Comprehensive Specialized Hospital, Hawassa University Comprehensive and specialized Hospital, and Negist Elenni Mohammed Memorial Specialized Hospital. These medical facilities were selected with a lottery method from the region's nine teaching hospitals.
Hawassa University Comprehensive Specialized Hospital (HUCSH) is a tertiary referral academic medical center found in Hawassa town, one of the regional cities in Ethiopia (it is the capital city of the Sidama region), located about 276 km from Addis Ababa. The hospital offers one neonatal intensive care unit (NICU) and one general intensive care unit (ICU) with 11 beds that can accommodate critically ill patients from all specialties. It provides services to people in Ethiopia, including the Sidama region, southern nationalities, and peoples of neighboring zones and regions, including the Oromia region [20].
Wolaita Sodo University Comprehensive Specialized Hospital (WSUCH) is situated in the Southern Nation Nationality of People of the Region of Ethiopia, approximately 154 kilometers away from Hawassa, the regional center, and 327 kilometers away from Addis Ababa. In terms of research, education, and healthcare delivery, this facility is vital to the Wolaita Zone and beyond. The hospital can provide comprehensive care for all critically ill patients from all specialties thanks to its eight ICU beds [21].
Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital (NEMMCSH) is one of the governmental hospitals that is found in Hosanna town, an administrative city in the Hadiya zone. It is located at a distance of 230 km to the south of Addis Ababa. The hospital has 6 ICU beds for comprehensive care of all critically ill patients from all specialties [22].
Worabe Comprehensive Specialized Hospital (WCSH) is located in southern Ethiopia, 173 km away from Addis Ababa. The hospital provides inpatient treatment services for medical, surgical, OB/Gynecology, pediatric, and psychiatric patients. The hospital has five ICU beds for comprehensive care of all critically ill patients from all specialties [23].
All patients admitted to the intensive care units of selected teaching hospitals of southern Ethiopia.
All patients who were admitted to the intensive care units of selected teaching hospitals of southern Ethiopia during the study period.
All patients aged 18 years and older who are stayed for longer than 24 hours were included in the study.
The sample size was calculated by a single proportion formula using a p value of 50%, a 95% CI, and a margin of error of 5%.
Where n = number of sample sizes, Z, statistics for a 95% confidence interval (1.96), and p = 50%. q = 1 - p; p = 0.5; hence, q = 0.5, d = 0.05 level of precision at a 95% confidence interval. By incorporating into the formula: (1.96)2 (0.5) (0.5)/(0.0025) = 384. By applying a finite population correction formula, the final sample size was calculated: Nf = n / (1+n/N); where Nf = the final sample size, n = the minimum sample size; and the total number of patients admitted to the ICU of the four selected teaching hospitals as obtained from situational analysis of the past January, February, and March/2015, which is 292, Nf = 384/(1 + 384/292) = 166. With a 10% non-response rate, the final sample size is n = 182. Study participants were included to the study consecutively. From the HUCSH, NEMMCSH, WSCH, and WSSCH College of Medicine and Health Science, 292 patients were obtained from situational analysis in January, February, and March 2015. The numbers obtained were considered the sample size at each selected hospital. In each specific specialized public hospital, the total computed sample size was allocated to a three-month ICU admission rate. Hence, the sample sizes found from HUSH, WSSH, NEMMCSH, and WSH were 52, 52, 40, and 38, respectively (Figure 1).
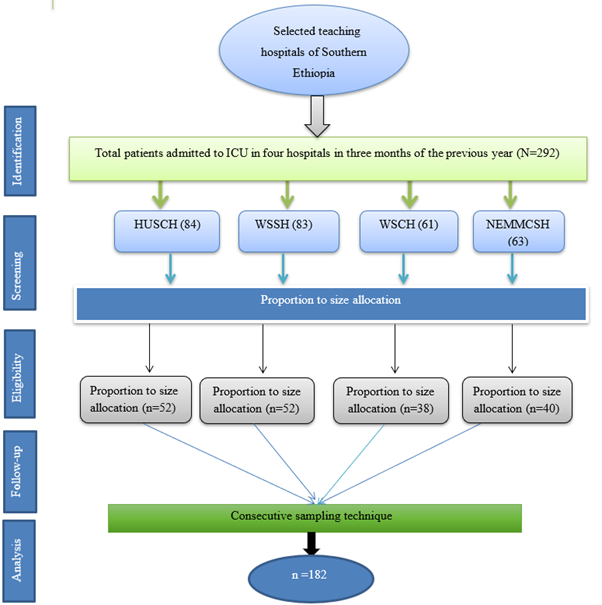
Figure 1: Strobe flow chart of sampling procedure among selected teaching hospitals in southern Ethiopia, January 15–April 15 (N = 182).
Dependent variable: Delirium (Yes/No)
A pre-tested questionnaire was used to collect the data. The principal investigator developed the questionnaire, which includes sociodemographic variables and patient and institutional-related variables, after a review of the literature reviews and similar studies [4,6,24].
Four data collectors and four supervisors were involved in the data collection. The principal investigator provided training in the administration of the CAM-ICU and RASS to data collectors and supervisors with a video-assisted, flowchart-guided, and patient-side demonstration. One emergency medicine and critical care physician, one intern, and two MSc-holding anesthetists were involved in the data collection. All participants participated in a training session and completed a 5 hour individualized training program. They also received comprehensive instruction manuals. The data was collected consecutively from each of the candidate patients after 24 hours of their admission, when consent was obtained from the caregivers. Patients were screened for delirium during the initial interview and 24 hours apart during the entire follow-up time. The data collection started every day at 3 a.m. local time. The follow-up was for 2 weeks until delirium occurred.
For the assessment of delirium, the confusion assessment method for the intensive care unit (CAM-ICU) was used, which is a validated tool for the intensive care unit. This tool has been mentioned to have a sensitivity of 0.82 (95% CI: 0.75-0.87) and a specificity of 0.95 (95% CI: 0.93-0.97) [25,26]. Diagnosis of delirium using CAM-ICU is suggested if features 1 and 2 plus either feature 3 or feature 4 are positive [27,28].
Feature 1: acute onset or fluctuating course of mental status (assessed by RAAS); Feature 2: inattention vigilance ‘A’ test or digit spans test if there are more than 2 errors taken as +ve for delirium, Feature 3: Altered level of consciousness (actual RAAS other than 0) and Feature 4: Disorganized thinking (yes or no questions for disorganized thinking) If there is more than one error, it is taken as delirium-positive [28].
The Richmond Agitation and Sedation Scale (RASS) was used to assess the level of sedation and agitation. It is a standardized 10-point sedation scale that goes from -5 to +4. RASS has 87.6% specificity and 84.0% sensitivity. A patient who has a score of 0 is considered to be conscious and calm. RASS was also used to identify subtypes of delirium [29].
The initial step is to determine the patient's level of awareness using the RASS scale. If the patient fulfills verbal commands (RASS score other than -4 and -5), the CAM-ICU will assess the patient for delirium. When a patient had a RASS of +1 to +3, it was considered hyperactive delirium. Those with negative scores between 0 and 3 were classified as having hypoactive delirium, while participants with a varying RASS score of positive and negative were classified as having mixed types of delirium [12].
The 16-item Informant Questionnaire on Cognitive Decline for the Elderly (IQCODE) was used for patients over 50 years of age before data collection was started to evaluate patients' cognitive function in the past 6 months by using inputs from caregivers [30]. Every IQCODE item is scored using an ordinal five-point Likert scale (ranging from 1 to 5), and the average score for all items is determined. Greater scores suggest cognitive deterioration; values greater than 3.44 were taken as indicating prior cognitive impairment [31].
After ethical approval was obtained, a pretest was conducted to assess the quality of the data collection tool. It was done at Bule Hora University Teaching Hospital two weeks before the actual data collection was started. The Cronbach’s alpha result for the pretest done on 5% of the sample size was 0.704.
Training was given to data collectors and supervisors. The supervisors checked for the completeness of the data daily. After data collection was completed, it was also checked for completeness and clarity by the principal investigator and the supervisors.
After the completion of data collection, SPSS version 26 was used to check code, enter, and analyze the data. The study characteristics of the participants were analyzed using descriptive statistics. The findings were presented as needed in text, tables, and graphs.
A linear regression was used for the multicollinearity test. Binary logistic regression was employed to assess the relationship between independent and dependent variables, as well as multivariable regression to identify the variables that showed independent associations with delirium. The degree of association and level of statistical significance were finally determined at a p-value of less than 0.05 using the adjusted odds ratio with a 95% confidence interval, respectively.
Ethical approval was obtained from the Hawasa University Comprehensive and Specialized Hospital School of Medicine, Ethical Review Committee (IRB/062/16). Further permission was obtained from Wachamo, Wolita Sodo, and Worabe Comprehensive Specialized Hospitals.
The caregivers provided their informed consent after the data collectors explained the benefits and objectives of the study to them. In addition, each study subject verbally gave his or her consent. The study gave disclosure of the subjects' complete right to discontinue participation at any moment to anyone unwilling to take part. Confidentiality and anonymity were ensured.
A total of 182 patients were enrolled in this study, resulting in a response rate of 100%. The majority of patients, 78.6% (n = 143), admitted to the ICU were within the age range of <60 years. Moreover, 52.2% (n = 95) of the patients were male, as shown on (Table 1).
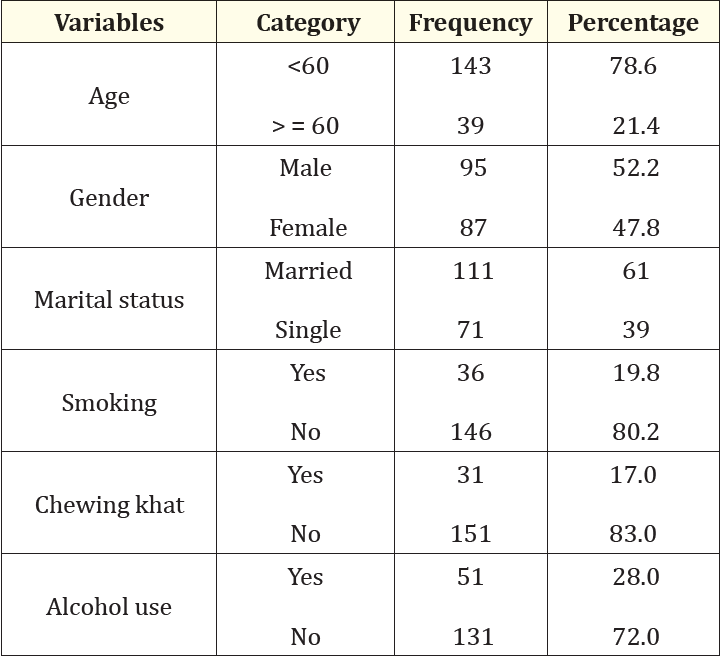
Table 1: Socio-demographic characteristics of patients admitted to the intensive care unit in selected teaching hospitals of southern Ethiopia, January 15-April 15, 2024 (n = 182).
The most of the patients, 40.1% (n = 73), were surgical, followed by trauma patients, 33.5 (n = 61). Only 18.1% (n = 33) of patients had previous head trauma. About 48.9% (n = 89) were exposed to sedation. A mechanical ventilator was used for 56.6% (n = 103) of patients. 20.3% (n = 33) of the patients stayed for more than 2 weeks. Physical restraint was applied to 73.6% of the patients, as shown in (Table 2).
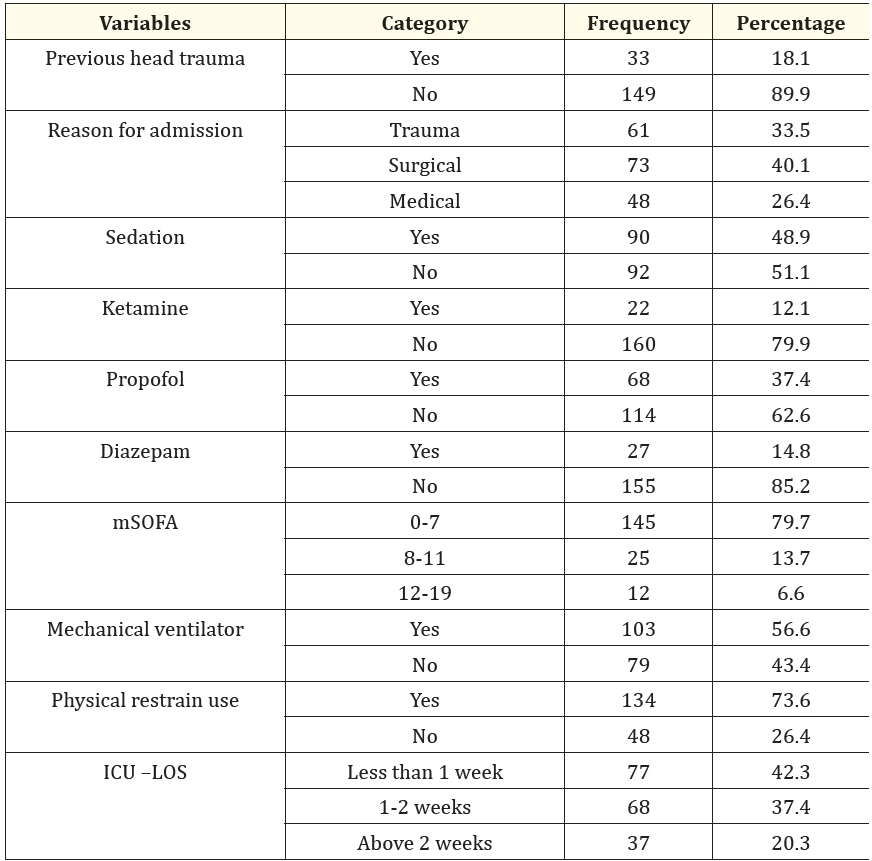
Table 2: Patient Characteristics and treatments employed in patients admitted to the intensive care unit in selected teaching hospitals of southern Ethiopia, January 15-April 15, 2024 (n = 182).
Key: mSOFA: Modified Sequential Organ Failure Assessment; ICU LO: Intensive Care Unit Length of Stay
In this study, the cumulative incidence of delirium is 30.8%. It has occurred in 56 patients among 182 admitted patients during their ICU stay. The subtype of delirium in most of the patients was hyperactive (53.6%; n = 30), followed by hypoactive (39.3%; n = 22) (Figure 2).
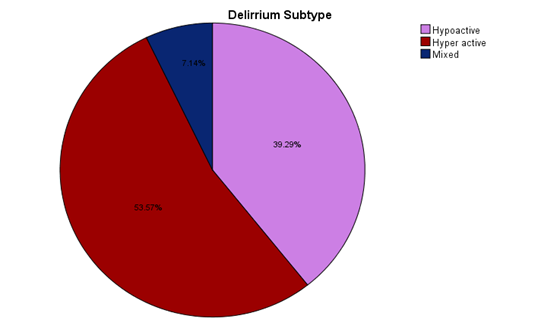
Figure 2: The incidence rate of subtypes of delirium in patients admitted to intensive care units in selected teaching hospitals of southern Ethiopia, January 15-April 15, 2024 (n = 182).
Our study results revealed that gender, marital status, smoking, sedation, alcohol use, chewing khat, high creatinine level, sedation, propofol, ketamine, feeding tube usage, and physical restraint use were significantly associated with ICU delirium.
In multivariate logistic regression analysis, we have found a significant correlation between marital status (being single) (5.560 (95% CI 1.844-16.765, p = 0.002), smoking (4.48 (95% CI 1.496-13.418), p = 0.007), alcohol use (4.85 (95% CI 1.780-13.217, p = 0.002), and propofol (3.776 (95% CI 1.265-11.275, p = 0.017) with ICU delirium (Table 3).
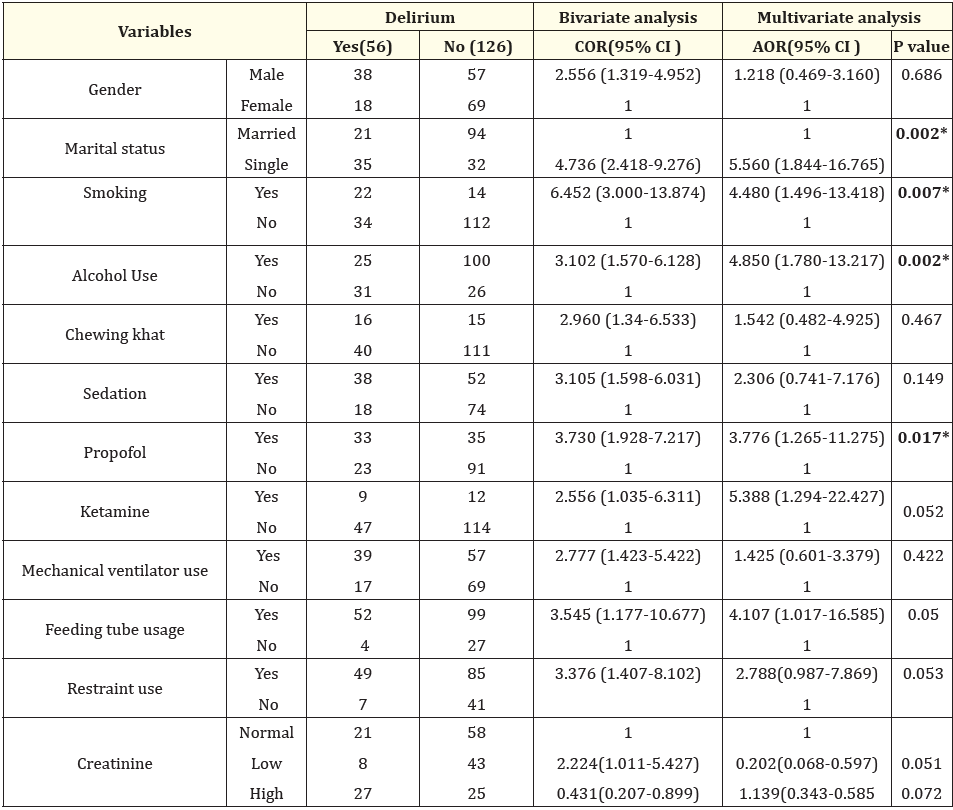
Table 3: Bivariate and multivariate binary logistic regression analysis result for risk factors associated with ICU delirium among patients in selected teaching hospitals of southern Ethiopia, January 15–April 15, 2023 (n = 182).
Key 1: Reference, COR crude odds ratio, AOR =adjusted odds ratio, CI confidence interval.
In our study, ICU delirium occurred in 30.8% (95% CI 24.7-35.8%) of the cases. This study result is in line with the studies conducted in China, India, Iran, Jordan, Oman, Turkey, and the Czech Republic [4,6,10,11,36-39].
Higher incidences, on the other hand, were found in other studies, which can be explained by variations in sample size, ICU settings, the severity of illness or patient characteristics, and diagnostic tools used. Our study showed a lower incidence compared with the studies conducted in China and Brazil [12,40], which revealed an incidence rate of 36.1% and 46.3%, respectively. This difference may result from the shorter study period in our study and the severity of the disease.
The result of our study revealed a higher incidence than reported results in previous studies conducted in Ireland [8], Saudi Arabia [9], and Korea 15.3% [41]. The discrepancy could be due to differences in the level of ICU care, accessibility of medical supplies, a multi-center study area in our study, and patient characteristics.
Patients with hyperactive delirium, which is characterized by restlessness, alertness, or aggressive behavior, were high in number. The incidence of hyperactive delirium was higher (53.6%), followed by the hypoactive type of delirium (39.5%), which was consistent with the claims of M. Kanova., et al. [6] Y. Pan., et al. [13]. and P. Limpawattana., et al. [13].
By contrast, patients with hypoactive delirium that are characterized by lethargy, drowsiness, and decreased reactivity are relatively low, and this result contradicts the previous study by A. K. Jayaswal., et al. and W. Ma., et al., respectively, which stated that the hypoactive type of delirium was the most commonly occurring subtype of delirium [36,37]. The reason behind this inconsistent result is likely that most of the patients in our study were <60 years old, while hypoactive delirium is common in patients above 65 years of age [1]. In addition to this, the delirious participants in this study had a history of smoking, and this hyperactive type of delirium can be due to nicotine withdrawal during their ICU stay [42]. In addition, it could be due to the assessment tool we used (CAM-ICU), which needs patient communication, that we might miss the hypoactive type of delirium.
It is observed in our study that delirium is significantly associated with marital status (being single), tobacco smoking, alcohol use, and propofol. Being single was 5.5 times (AOR = 5.560; 95% CI 1.844-16.765) more likely to experience delirium than those who are married. The possible reason for this could be that those who are single are more vulnerable to various physical conditions, mental health disorders, drug abuse, and other conditions that raise the risk of delirium. This study result was consistent with the study results in Iran [4].
The odds of participants with a history of smoking having delirium were 4.48 times (AOR = 4.480, 95% CI: 1.496-13.418) times the odds of participants who were not previously smoking. The most likely reason for this high incidence is smoking withdrawal during their hospital stay, which results in an imbalance in neurotransmitters [43]. Pathophysiologically, both delirium and nicotine withdrawal are linked with cholinergic deficiency [37]. This study finding was also supported by the previous study done in Iran [4].
Alcohol use is among the patient-related risk factors that independently affect delirium occurrence, as our study result showed. The participants who had a history of alcohol use had 4.85 times the odds of non-alcohol users (4.850) (1.780-13.217). This could be because alcohol use can cause a reduction in the functionality and number of GABA receptors and an enhancement of N-methyl-D-aspartate receptors [2]. This study's result was in line with the study done by M. Kanova., et al. in Central Europe [6].
According to this study result, propofol is also a potent independent predictor of ICU delirium. Those who were given propofol were 3.77 (AOR = 3.776, CI: 1.265-11.275) times more likely to develop delirium than those who had not been given it. This might be due to the active interaction of propofol with the muscarinic acetylcholine receptors [44]. This result was supported by evidence from previous studies in Nairobi and Brazil [8,40].
In previous studies, age was an independent risk factor for delirium, and the incidence was higher in older age groups. However, in our study, delirium was relatively high in patients with the age of <60 years (78.6%). This study finding was not in line with the studies in the Czech Republic, Ethiopia, and China, which revealed that patients aged >65 and 60 years, respectively, had a significant association with delirium [6,14,36]. This discrepancy could be due to variations in sample size and differences in patient distribution, as more than half of the participants in this study were in the age group of < 60 years.
While previous study results have focused on the higher incidence of delirium in patients with higher disease severity, organ dysfunction, mechanical ventilator use, the age of the patients, and ICU length of stay, this study result demonstrated that marital status, being single, tobacco smoking, alcohol use, and propofol are also independent risk factors for delirium occurrence [4,12,36,37]. Strength of the study is a multi-center and prospective study and the first in its kind in southern Ethiopia but we assessed delirium in the daytime only, we might have missed detecting the hypoactive type of delirium that is more common at night is limitation of the study.
Delirium is relatively low in critical patients admitted to the intensive care unit at Southern Ethiopia specialized hospitals. Single status, smoking, alcohol use, and propofol are risk factors that are independently associated with the incidence of delirium. It is necessary to identify delirium early and implement immediate management.
Ethical approval was obtained from the Hawasa University Comprehensive and Specialized Hospital School of Medicine, Ethical Review Committee (IRB/062/16). Further permission was obtained from Wachamo, Wolita Sodo, and Worabe Comprehensive Specialized Hospitals.
The caregivers provided their informed consent after the data collectors explained the benefits and objectives of the study to them. In addition, each study subject verbally gave his or her consent. The study gave disclosure of the subjects' complete right to discontinue participation at any moment to anyone unwilling to take part. Confidentiality and anonymity were ensured. All methods were carried out in accordance with declaration of Helsink.
The study was funded by Hawasa University.
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
The authors declare that there is no conflict of interest.
The author would like to thank Hawasa University for funding this project.
Not applicable
MM and KT were responsible for data collection, statistical analysis and interpretation, wrote the manuscript. MK, MM, AS and FB interpreted and supervised statistical analysis and edited the manuscript. All authors have read and approved the manuscript.
Copyright: © 2024 Mebratu Kebede. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.