Binal Dave*
Women’s Health Department, Saveetha Medical University, India
*Corresponding Author: Binal Dave, Women’s Health Department, Saveetha Medical University, India.
Received:October 09, 2024;; Published: October 21, 2024
Citation: Binal Dave. “Physiotherapy Assessment and Management of Overactive Bladder Syndrome: A Case Report". Acta Scientific Women's Health 6.11 (2024): 19-25.
Introduction: Treatment options for Overactive Bladder Syndrome (OAB) include electrostimulation, medication, pelvic floor muscle training, and surgery. Pelvic floor muscle training is a component of physical therapy, which is one nonpharmacological treatment option.
Case Description: The patient, a 35-year-old female, came to the urogynecological physiotherapy consultation room because she was experiencing frequent pressure in her bladder. The physiotherapist employed both manual inspection to evaluate the pelvic and abdominal structures' functionality. The patient complained of pain when several abdominal and pelvic floor muscles were examined. It was determined that the patient qualified for urogynecological physical therapy. Manual therapy was applied to the musculus piriformis, the superficial back line myofascial meridian, the lateral line myofascial meridian, the lumbopelvic hip complex, and the pervaginum. In the last session, the patient reported that the symptoms had improved, most notably the absence of frequent bladder pressure.
Conclusion: Often, treating OAB requires a multi-phase approach involving the use of various therapies by a multidisciplinary team. The conservative management of OAB for this patient included physiotherapy assessment and intervention.
Keywords: Overactive Bladder; Physiotherapy Techniques; Urologic Diseases; Soft Tissue Therapy; Pelvic Floor Therapy
Increased frequency of urination and nocturia accompanied by an abrupt sensation of bladder pressure is known as overactive bladder syndrome (OAB) (White and Iglesia, Citation 2016) [1]. Urinary leakage (OAB wet) or none at all may accompany these symptoms (OAB dry). In addition, other pathologies of the urinary system such as UTIs are not included (Bø., et al. White and Iglesia, Citation (2016); Robinson and Cardozo, Citation 2019) [2]. There are numerous reasons for overactive bladder syndrome, including neurological (i.e. e. disorders of the bladder innervation), myogenic (i.e. e. hypersensitivity to stimuli or dysfunction of the bladder detrusor muscle), or idiopathic (Jankiewicz, Kulik-. 2012; Rechberger, Nowakowski, and Rechberger; 2007; White and Iglesia, Citation (2016)) [3]. According to other guidelines, pelvic organ prolapse (POP) should not be the cause of OAB symptoms before an OAB diagnosis is made. Yet, a number of experts feel that symptomatic POP shouldn’t have an impact on the OAB diagnosis and treatment procedure (Grzybowska., et al. Reference 2021) [4]. According to Eapen and Radomski (Citation 2016a), OAB symptoms are more common in women (12.8%) than in men (10.8%) in the general population. Anatomical and physiological factors could be to blame for this.OAB is a nuisance that significantly lowers patients’ quality of life and well-being, which leads to social, professional, and personal life limitations and frequently exclusion (Gormley, Lightner, Faraday, and Vasavada, Citation 2015; Jankiewicz, Kulik-Rechberger, Nowakowski, and Rechberger, Citation 2012; White and Iglesia, Citation 2016) [5]. There are various treatment tiers for OAB management. Physical exercise, dietary modifications, training of the pelvic floor muscles, training of the bladder with biofeedback, regulation of fluid intake, or electrostimulation are all part of the first tier (Gormley, Lightner, Faraday, and Vasavada, Citation 2015) [6]. Przydacz along with others. Citation 2020). OAB is a nuisance that significantly lowers patients’ quality of life and well-being, which leads to social, professional, and personal life limitations and frequently exclusion (Gormley, Lightner, Faraday, and Vasavada, Citation 2015; Jankiewicz, Kulik-Rechberger, Nowakowski, and Rechberger, Citation 2012; White and Iglesia, Citation 2016) [7]. There are various treatment tiers for OAB management. The first tier includes exercise, dietary modifications, training of the pelvic floor muscles, training of the bladder with biofeedback, management of fluid intake, orelectrostimulation (Grzybowska., et al. 2015; Gormley, Lightner, Faraday, and Vasavada, Citation 2015) [6]. Citations: White and Iglesia (2016), Robinson and Cardozo (2019), and Citation 2021 [7]. The second stage of treating OAB is pharmacotherapy, which involves the use of anticholinergic medications like mirabegron and solifenacin (Gormley, Lightner, Faraday, and Vasavada, Citation2015; Grzybowska., et al. Citations: Grzybowska (2015), Robinson and Cardozo (2019), Citation 2021 [8]. Injections of botulinum toxin (BTX), percutaneous tibial nerve stimulation (PTNS), or sacral nerve stimulation (SNS) are used in the third tier of treatment (Gormley, Lightner, Faraday, and Vasavada, Citation2015; Grzybowska., et al. [9] Citations 2021 and 2019 by Robinson and Cardozo [8]. The alternative course of treatment, sometimes known as the fourth tier, involves surgery (i.e.(Jankiewicz, Kulik-Rechberger, Nowakowski, and Rechberger, Citation 2012; Rechberger, Citation 2007; White and Iglesia, Citation 2016) [7] augmentation cystoplasty or bladder drainage. This case study shows how a patient with OAB was able to experience symptom relief through tailored physical therapy and appropriate functional diagnostics.
Case description: The patient, a 35-year-old woman, came to the urigynaecological department because she was experiencing frequent pressure in her bladder and frequent nocturia. The patient saw a urologist prior to the visit, who diagnosed Overactive Bladder Syndrome (ICD10: N31.8). About two or three years ago, the first symptoms appeared with no apparent reason. Although there had not been any bladder or urethral infection episodes i the previous 12 months, the patient disclosed the existence of past episodes. She did not disclose any past history of childbirth, injuries, or spine or pelvic surgery. Although the patient was sexually active, having sex was uncomfortable for her and she occasionally felt pressure in her bladder as well as nocturia. The patient saw a urologist prior to the visit, who diagnosed Overactive Bladder Syndrome (ICD10: N31.8). About two or three years ago, the first symptoms appeared with no apparent reason. Although there had not been any bladder or urethral infection episodes in the previous 12 months, the patient disclosed the existence of past episodes. She did not disclose any past history of childbirth, injuries, or spine or pelvic surgery. The patient gave written informed consent for the case to be published, and the ethics committee waived the requirement for approval. The patient was sexually active, but had painful sex and occasionally felt pressure in her bladder. The patient provided written informed consent for the case to be published, and the ethics committee waived the need for approval.
In the initial visit, the pelvic floor muscles were assessed structurally and functionally using manual inspection and biofeedback imaging (i.e. E. per vaginum palpation). Additionally, an assessment was conducted on the muscles of the lateral line myofascial meridian, the gluteal muscles, and the superficial back line myofascial meridian (Myers, Citation 2020) [9]. Throughout the examination, the patient was asked to rate their subjective sensation of bladder pressure on a scale of 0 to 10. A score of 0 indicated no bladder pressure, while a score of 10 indicated extreme urgency for micturition. She gave it a 9 out of 10, indicating that there may be problems with how the bladder is perceived to be full and that the sensation of the bladder filling is not accurate. Next, the pelvic floor's myofascial structures were examined for any abnormalities or diseases. There were no pathologies or damage found in the pelvic floor. These results, along with other testing procedures, ruled out pelvic organ prolapse as the cause of the symptoms of pain and frequent urge during sex. The assessment of the pelvic floor muscles’ voluntary phasic and tonic contraction came next. First, phasic activity was evaluated. Without any prior guidance, the patient was instructed to rapidly contract their pelvic floor muscles. The physiotherapist evaluated the patient's contraction dynamics, direction, and intensity. e. elevated, lowered, or unchanged), as well as the potential for peripheral stabilization manifested as heightened lower extremity, abdominal, and gluteal muscle tension (Arokoski, Valta, Airaksinen, and Kankaanpaa, Citation 2001) [10]. The patient showed correct phasic contraction of the pelvic floor muscles with elevation with no apparent peripheral stabilization. The patient was asked to contract their pelvic floor muscles and hold that position for eight seconds in order to measure their tonic activity.
The evaluation was based on the same criteria as for phasic contraction: contraction dynamics, direction, peripheral stabilization presence, and ability to sustain contraction. Without obvious peripheral stabilization, the patient showed proper tonic contraction of the pelvic floor muscles while elevated. Therefore, it was determined that the frequent urge and painful sex were not caused by improper pelvic floor muscle functioning. The patient was then placed in the same position for a per vaginum examination by the physiotherapist. The physiotherapist started the examination by looking at the perineal area, noting the skin's color, the vaginal opening's appearance, and searching for scar tissue. Neither the vaginal opening nor the perineal region showed any obvious pathological changes. The bulbocavernosus reflex was then tested by applying pressure to the clitoral glans (Previnaire, Citation 2018) [6]. A proper reflex response was noted, indicating appropriate innervation from the S2-S4 level. The physiotherapist also used palpation to measure the central tendon of the perineum's flexibility and pain prevalence. Additionally, when coughing, the central tendon of the perineum’s dynamic function was assessed. After asking the patient to cough, the physiotherapist noted that the central tendon moved upward and then downward in a proper reflex response. After ruling out any potential external pathologies, the perineal behavior was visually evaluated. The pelvic floor muscles per vaginum were palpated as the next step in the examination to see if any pain was present. Using a Numerical Rating Scale (NRS) with 0 representing no pain and 10 representing the worst possible pain, the patient was asked to report any pain during palpation and to describe its intensity. Both sides’ muscles were tested, and Table 1 shows the results.
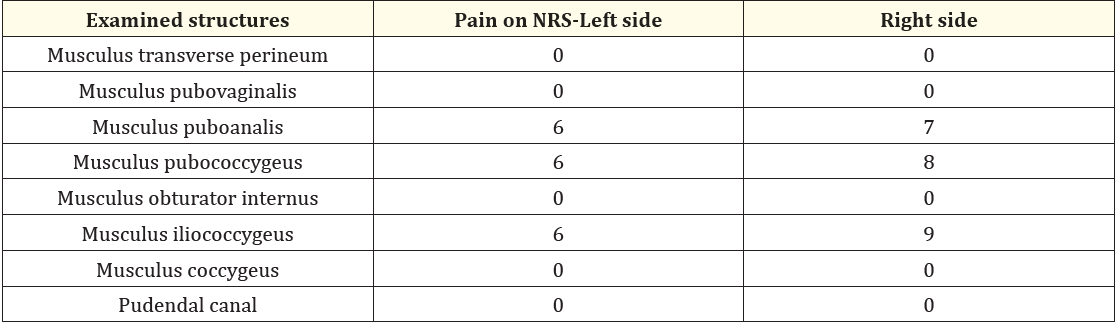
Table 1
The evaluation of the phasic and tonic contraction of specific pelvic floor muscles was then done by palpation. The patient was instructed to rapidly contract the pelvic floor muscles by the physiotherapist, who put the index finger in the musculus pubovaginalis area. e. phasic contraction), wherein the measurable parameters of contraction strength, dynamic contraction, and ability to contract were evaluated. The patient was then instructed to execute a second pelvic floor contraction and hold it for eight seconds (a tonic contraction) by the physiotherapist as she moved on to the musculus puboanalis. Next, the musculus pubovaginalis and musculus bulbospongiosis phasic activity. The patient was instructed to contract the pelvic floor muscles after the physiotherapist used the index and middle fingers to widen the vaginal orifice. The patient showed accurate responses in each test, and there was no sign of peripheral stabilization. With the patient on her back and her lower limbs fully extended, an assessment examination of the lumbopelvic hip complex was then performed. Using both hands, the physiotherapist assessed the anterolateral abdominal wall via palpation. Pain and tension in the muscles were assessed. The patient used the NRS to describe any pain they felt during palpation and to indicate how intense it was. The musculus rectus was the first area the physiotherapist evaluated, with the results shown in parenthesis. 1) The left side (7/10) and right side (7/10) have musculus rectus abdominis at the level of the umbilicus; 2) The left side (0/10) and right side (5/10) have musculus psoas major; 3) The left side (0/10) and right side (8/10) have musculus transversus abdominis in the middle of the line connecting the anterior superior iliac spine and public symphysis; and 4) Abdominal palpation revealed abnormalities in the tension of the muscles generating intra-abdominal pressure, which may result in symptoms of urgency. The Lasèque Test was used in the same position. The leg that has been straightened is slowly raised until pain starts during this test. The physiotherapist focused especially on the angle between the leg and the rest surface at the point of pain and the pelvic position during the test due to potential compensation. The observed angle was more than 60 degrees, so the test was negative on both sides. During the test, the patient did not report any lower extremity or lumbosacral pain (Buckup) [8]. After that, in a supine position, the tension in the lateral line myofascial meridian and the superficial back line myofascial meridian was measured. The patient’s leg was raised and the ankle was simultaneously dorsiflexed by the physiotherapist in order to assess the superficial back line myofascial meridian. The leg was raised until resistance was felt, which the patient reported as a pulling sensation along the superficial back line myofascia or as apparent compensation manifested as knee flexion (Myers, Citation 2020) [9]. The patient was also asked to describe any pain and its level on the NRS and Buckup, Citation 2016) [5]. These results ruled out compression of the sciatic nerves and irritation of the nerve roots as the patient's reported disorders' causes.
After that, in a supine position, the tension in the lateral line myofascial meridian and the superficial back line myofascial meridian was measured. The patient's leg was raised and the ankle was simultaneously dorsiflexed by the physiotherapist in order to assess the superficial back line myofascial meridian. The leg was raised until resistance was felt, which the patient reported as a pulling sensation along the superficial back line myofascia or as apparent compensation manifested as knee flexion (Myers, Citation 2020) [10]. The patient was also asked to describe any pain and its level on the NRS. The patient reported pain on the left side at a score of 6/10 and the right side at an 8/10 along the superficial back line myofascia. In the same posture, the lateral line myofascial meridian was examined. The patient's leg was raised by the physiotherapist while the hip and ankle joints were simultaneously abducted. The leg was abducted until resistance was felt, which the patient reported as a pulling sensation along the lateral line myofascial meridian or as apparent compensation manifested as knee flexion (Myers, Citation 2020) [10]. The patient experienced pain on the left side at 7/10 and the right side at 9/10 along the lateral line myofascial meridian. The superficial back and lateral line myofascial meridians’ functional shortening was observed during examination; this has an Impact on the pelvic floor muscles as well as the position and function of the abdominal wall. The musculus piriformis was assessed as the last phase of the physiotherapy evaluation process. The patient was once more in the same posture as before. The physiotherapist measured muscle tension and pain by palpating the musculus piriformis along the muscle’s length with both hands. The patient was instructed to use the NRS to report any pain and to indicate how severe it was. During the examination, the patient indicated a pain level of 9 out of 10 on the left side and 4 out of 10 on the right side. This assessment revealed heightened tension in the piriformis muscle, which could also influence the increased tone of the pelvic floor muscles.
The physiotherapy assessment revealed an excessive sensation of bladder fullness even with a filling of 260 ml, along with increased tension in the pelvic floor muscles, abdominal wall, piriformis muscle, superficial back muscles, and lateral line myofascial pathways. Due to the complexities and nature of overactive bladder (OAB) syndrome, predicting a return to a symptom-free state proved to be quite challenging. Research indicates that substantial morphological improvements and symptom relief in patients with urinary incontinence were noted after engaging in pelvic floor muscle training consistently for a minimum of three months (Braekken, Majida, Engh, and Bo; Citation 2010; Lightner, Gomelsky, Souter, and Vasavada, Citation 2019) [5]. Based on the physiotherapeutic assessment, the patient was deemed suitable for urogynecological physiotherapy. The treatments involved manual therapy targeting the lumbopelvic hip complex, vaginal manual therapy, manipulation of the piriformis muscle, and therapy for the superficial back line and lateral line myofascial meridians. Intervention Following the physiotherapeutic assessment, the patient was deemed suitable for urogynecological physiotherapy. Treatment included manual therapy targeting the lumbopelvic hip complex, vaginal manual therapy, piriformis muscle therapy, as well as treatment for the superficial back line and lateral line myofascial meridians. The physiotherapy regimen comprised ten sessions lasting 40 minutes each, scheduled over a period of six weeks (refer to Table 2).
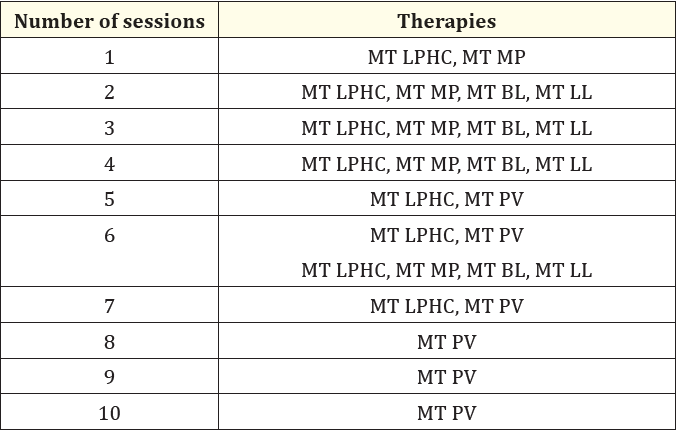
Table 2
The manual therapy for the lumbopelvic hip complex involved techniques such as trigger point therapy, friction massage (including stroking, rubbing, and kneading), and manual diaphragm release. These methods were applied while the patient was positioned on her back, with her arms resting along her sides and her legs supported on a couch, aiming to relax the abdominal wall. Additionally, manual therapy through the vaginal approach utilized trigger point therapy, friction massage, and post-isometric relaxation. This was carried out with the patient in a supine posture, her lower limbs bent at both the hip and knee joints and her feet flat on the couch, with the goal of relaxing the pelvic floor muscles.
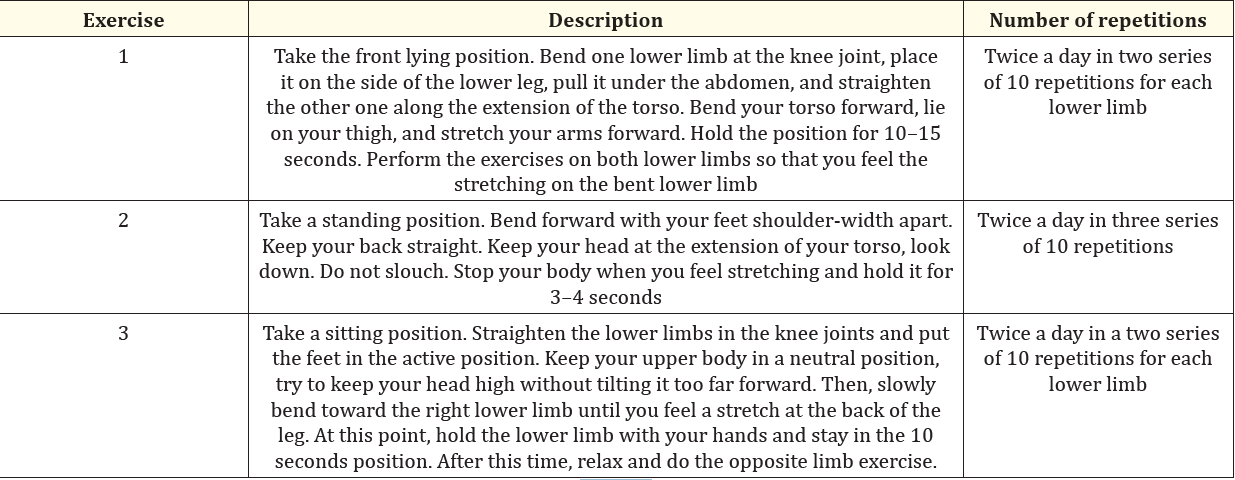
Table 3
Treatment for the superficial back line and lateral line myofascial meridians involved post-isometric relaxation and mobilization methods. These techniques were applied while the patient lay on their back, with one leg elevated, flexed at the hip, and extended at the knee. To stretch the posterior line, dorsiflexion of the foot was utilized, while adduction of the lower limb was implemented to target the lateral line myofascial meridian. Additionally, hip flexion was enhanced. Transverse massage and post-isometric relaxation of the lower limb muscles were also employed to boost treatment efficacy. Therapy for the piriformis muscle included trigger point therapy and friction massage, performed with the patient in a prone position. In the last session, the patient indicated that their symptoms had improved, particularly noting a reduction in the frequent sensation of bladder pressure. As a result, trips to the restroom during both the day and night were less necessary. The patient also mentioned experiencing neither pain nor urgency during sexual activity. Before the follow-up appointment, they were provided with a customized program of exercises to complete, which included stretching routines targeting the superficial back line and lateral line myofascial meridians, as well as the piriformis muscle (see Table 3).
Four weeks following the final treatment session, the patient returned for a follow-up appointment where she noted progress in her urinary symptoms, specifically a reduction in the frequent feeling of bladder pressure and nighttime urination. Furthermore, the physiotherapist conducted a complete evaluation again, similar to the initial visit.
During the cough stress test, the urethra responded appropriately, and the musculus pubovaginalis and musculus puboanalis were active, with no leakage of urine or compression of the lesser pelvic organs noted. Upon per vaginum examination, the patient encountered no discomfort during palpation and exhibited normal phasic and tonic activity in the pelvic floor muscles. When examining the anterolateral abdominal wall, the patient did not experience pain in the structures on the left side; however, pain on the right side had diminished to 2/10 on the Numeric Rating Scale (NRS). Both sides of the superficial back line myofascial meridian were still painful, but the patient indicated a lower pain intensity, rating it as 5/10 on the left and 4/10 on the right. The patient also noted pain relief and progress observed during the lateral line evaluation: the pain intensity on both the left and right sides reduced to 5 out of 10 on the NRS. Pressing on the piriformis muscle did not produce any pain responses. Given these findings, the physiotherapist suggested continuing with the tailored exercise program and scheduling a follow-up appointment in approximately three months.
The final follow-up visit took place five months after the initial visit and three months following the last follow-up visit. The patient reported almost complete relief of the symptoms, which she had originally presented at the center. Once again, the physiotherapist performed the whole examination as described above. The bladder volume was estimated at 270 ml, and the patient’s subjective feeling of bladder pressure was identified as 6. Such a result suggests the improvement and normalization of the sensation of the bladder. Before the therapy, the patient assessed the urgency to urinate on a scale of 0–10 out of 9 with 260 ml bladder filling, after therapy 9 with 380 ml filling and 6 with 270 ml filling. The pelvic floor muscles exhibited both correct phasic and tonic activity alongside proper elevation. There was no evidence of urine retention following urination. During the cough stress test, a suitable response from the urethra, as well as activity from the pubovaginalis and puboanalis muscles, was noted. The patient did not report any pain during the vaginal examination and showed appropriate phasic and tonic activity of the pelvic floor muscles. Additionally, there were no signs of urine leakage or depression of the lesser pelvic organs throughout the cough stress test. While palpating the anterolateral abdominal wall, the patient indicated experiencing pain in only one of the areas evaluated, specifically located away from the umbilicus. The patient rated the pain intensity as 1/10 on the Numeric Rating Scale (NRS) on both sides. No painful symptoms were reported during the examination of the back line. The assessment of the lateral line showed pain on the left side, with an intensity rated at 3/10 on the NRS. There were no pain symptoms detected in the musculus piriformis. After the interview and physiotherapeutic evaluation, both the patient and the physiotherapist agreed to end the physiotherapy process and determined that a referral to a urologist for a follow-up examination was necessary.
The consultation with the urologist showed no abnormalities. The patient was advised to persist with the prescribed exercises and keep an eye on her health status.
Overactive Bladder Syndrome (OAB) is a challenging condition that significantly affects individuals’ quality of life and overall well-being, potentially resulting in social isolation (Bø., et al; Citation 2020; Gormley, Lightner, Faraday, and Vasavada, Citation2015; White and Iglesia, Citation2016) [7]. Managing OAB requires a multi-faceted approach, incorporating various therapies and strategies. Consequently, the selection of a specific treatment for overactive bladder (OAB) should stem from evaluating risks and benefits, taking into account patients' expectations (Olivera., et al. 2016) [6]. Typically, medication is the primary treatment option. Nevertheless, pharmacotherapy is frequently halted due to less than satisfactory outcomes, such as insufficient symptom relief and/or the presence of side effects (Olivera., et al.; 2016, White and Iglesia, 2016) [7]. Some research indicates that the anticholinergic medications used to treat OAB may negatively impact the central nervous system, potentially resulting in long-term cognitive decline and dementia (Robinson and Cardozo, 2019) [8].
On the other hand, botulinum toxin therapy is related to a higher risk of urine retention and incidence of urinary tract infection. In addition, this therapy requires self-catheterization by patients and long-term observation shows that the healing effect passes in about 9–12 months, after which therapy must be repeated. A similar situation exists in the case of application of PTNS therapy because the symptoms of OAB tend to intensify 6–12 weeks after therapy (Olivera., et al. Citation 2016; Robinson and Cardozo, Citation 2019) [8]. The application of SNS therapy necessitates surgical intervention (in order to implant electrodes), which results in the exclusion of some patients due to their general health status (Robinson and Cardozo, Citation 2019) [8]. The most commonly used treatments for overactive bladder (OAB) may provide some symptom relief, but they do not fully eliminate the condition. This limitation could stem from their focus on alleviating symptoms rather than addressing the underlying causes. Therefore, it's crucial to conduct a thorough diagnostic process that considers the pathophysiology and risk factors associated with OAB (Kasman, Stave, and Elliott, Citation 2019) [8].
Gormley, Lightner, Faraday, and Vasavada (Citation 2015) [4] found that individuals with OAB frequently receive treatment from the second and third tiers, while behavioral therapy and other conservative approaches are seldom utilized. This likely stems from a lack of awareness regarding these conservative options, highlighting the necessity for broader educational initiatives on the subject. Similarly, Kasman, Stave, and Elliott (Citation 2019) [6] noted that conservative treatments are often underutilized and misunderstood among healthcare providers. Physiotherapeutic interventions are increasingly recognized as a vital aspect of urological care and serve as a potential conservative treatment alternative. Earlier research has examined the physiotherapeutic treatment of overactive bladder (OAB) primarily through the lens of pelvic floor muscle training (Bø., et al. 2020; Olivera., et al. 2016; White and Iglesia, 2016) [7]. The rationale behind the effectiveness of pelvic floor muscle training lies in the premise that increased muscle tension raises pressure in the urethra, which subsequently lowers the tension in the detrusor muscle, thereby suppressing the micturition reflex. This mechanism provides patients with additional time to reach restrooms and reduces the likelihood of urine leakage. Additionally, pelvic floor muscle training can induce lasting alterations in pelvic structure morphology, potentially stabilizing neural activity and pressure within the urethra.
Alongside pelvic floor muscle exercises, physiotherapy provides additional therapeutic methods for managing overactive bladder (OAB), as illustrated by the current case report. So far, there is limited research assessing the effectiveness of physiotherapy for OAB or contrasting various physiotherapeutic approaches. The absence of a standardized physiotherapeutic protocol for OAB treatment complicates the ability to endorse specific physiotherapy techniques for certain situations. Consequently, there is a significant need for more research in this field.
The results from this case report indicate that for the patient experiencing OAB syndrome, conservative treatment methods that emphasize proper pelvic floor muscle contractions, manual therapy for the pelvic floor and lumbopelvic hip area, along with personalized exercises, effectively alleviated the patient’s OAB symptoms.
We sincerely thank our client for her help during the process of research.
No potential conflict of interest was reported by the author(s).
The author(s) reported that there is no funding associated with the work featured in this article.
Copyright: © 2024 Preeti Arora., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.