Priya Ganeshkumar1, Bengia Chirchi2, Yam Narang2, Sharvari Ozalkar3, Shweta M Jangam3, Preeti Arora3*, Sanjay Gupte3,5 and Sarjan Shah4
1Medical Director, Sainiwas Healthcare, India
2Ram Krishna Mission Hospital Itanagar, Arunachal Pradesh
3Research Division of Accurate Diagnostics Private Limited, Pune, Maharashtra, India
4Greenarray Genomic Research and Solutions of ADPL, Pune, India
5Gupte Hospital, Pune, Maharashtra, India
*Corresponding Author: Preeti Arora, Research Division of Accurate Diagnostics Private Limited, Pune, Maharashtra, India.
Received:October 01, 2024;; Published: October 13, 2024
Citation: Preeti Arora., et al. “Population-Based Study on High-Risk Human Papilloma Virus Types in Itanagar: Prevalence and Implications". Acta Scientific Women's Health 6.11 (2024): 15-18.
Background: Cervical cancer is mainly attributed to infections caused by the Human Papillomavirus (HPV). In India, HPV infections are responsible for approximately 74,000 deaths annually, which represents nearly one-third of all cervical cancer fatalities. Data on HPV prevalence in a region is hence important because it helps us predict the risk of cervical cancer in that particular population. This study was done to know the prevalence among women of various age groups from Itanagar, Arunachal Pradesh. The study focuses on high-risk strains of HPV.
Methods: A total of 155 samples were collected from women of different age groups from Ram Krishna Mission Hospital, Itanagar. The samples were tested for the presence of high-risk HPV types using a PCR-based method, including but not limited to types 16 and 18. The prevalence of these infections was analyzed according to age groups, particularly focusing on the age group with the highest prevalence.
Results: Out of the 155 samples studied, 11 were found to be positive for various high-risk HPV types. The analysis revealed that, in addition to the commonly studied HPV types 16 and 18, other high-risk strains are also prevalent in the study population. Particularly, the prevalence was highest among women aged 30-40.
Conclusion: The findings suggest a significant presence of high-risk HPV infections in the studied cohort, with a maximum prevalence among women aged 30-40. This suggests the need for targeted HPV screening and vaccination programs in the region, starting the screening at an earlier age. The study highlights the importance of including a broader range of HPV types in epidemiological studies to better understand and address the risk factors associated with cervical cancer and other HPV-related diseases in this population.
Keywords: HPV; High-Risk HPV Types; Prevalence; Itanagar; Population-Based Study; Cervical Cancer; Screening; Age Groups
HPV: Human Papilloma Virus; PCR: Polymerase Chain Reaction; WHO: World Health Organization
Cervical cancer is one of the most common cancers affecting women globally. In 2020, it was reported that 604,000 new cases and overall 342,000 cases of cervical cancer were observed. Out of this 90% of all new instances of cervical cancer occur in developing nations, placing a heavy burden on these nations according to the World Health Organization (WHO) Factsheet, 2020 [1]. Compared to more urbanized areas of India, cervical cancer still affects 70% of the country's rural residents, indicating how common the disease is [2]. Majorly these cancers are caused by HPV infection. When HPV infection of the cervix is left untreated for a prolonged time, then these cases can develop 11 times higher risk of developing cervical cancer [3]. To understand the burden of HPV infection in the overall population and the prevalence of cervical cancer, it is necessary to study type-specific as well as co-infections [4,5]. Furthermore, evaluating the early effects of HPV vaccinations greatly impacts public health when examining the prevalence of the vaccine-targeted HPV strains in young women [6]. The prevalence of HPV also exhibits distinct age-related patterns of infection across various populations [7].
India being a lower middle-income country, cancer awareness and reach are limited to rural areas and many people are unaware of the disease [7]. This leads to a negative impact on the eradication of cervical cancer in India. Since the establishment of the earliest cancer registries in 2003, the incidence rates for all types of cancer have consistently been the highest in the northeastern states of India [8]. Despite the widespread of this infection across the nation there is no national screening program available currently [9]. This shows that there is an urgent need to screen and investigate this region's specific cancer patterns, as well as establish suitable screening programs to detect and bridge the study gaps.
This study was piloted to thoroughly investigate and document the prevalence of high-risk HPV types within the Itanagar area. By focusing on the distribution and frequency of these specific HPV strains, the study offers a detailed insight into the overall burden of HPV infections in this region. This information is crucial for understanding the potential public health impact, guiding future screening and vaccination strategies, and informing healthcare policy to better address the risk of HPV-related diseases, such as cervical cancer, within this population. The findings aim to contribute valuable data that can enhance the region's epidemiological profile and aid in the development of targeted interventions.
Ram Krishna Missionn Hospital of Itanagar was the collection center for this study and enrolling of the subjects. This study was conducted from March to July 2024. The inclusion criteria for the study considered symptoms like abnormal vaginal discharge, painful menstruation, or lower abdominal pain. Additionally, married women aged 20 to 50 years who appeared healthy were included in the screening process. Exclusion criteria were applied for women who were unmarried, pregnant, or undergoing treatment. Samples were collected using a cytobrush and kept in a standardized viral transport medium. The swabs were further stored at 4° C until further processing.
The DNA from the swabs was isolated using Mylab extraction kit- Maverick Spin Column-Based Isolation kit as per the manufacturer’s instructions. For establishing the adequateness of isolated DNA, the amplification of the human beta-globin gene was examined. PCR amplification and HPV genotyping were performed as per our previous publication [2].
A total of 155 samples were included in our study for screening of HPV infection. The age group varied from 23 years of age to 49 years of age women. The screening procedure took place during the months of March to July 2024. Out of these 155 subjects a total of 11 HPV high-risk positive infections were observed. This contributes to 7.09% prevalence as shown in 1. part of Table 1.
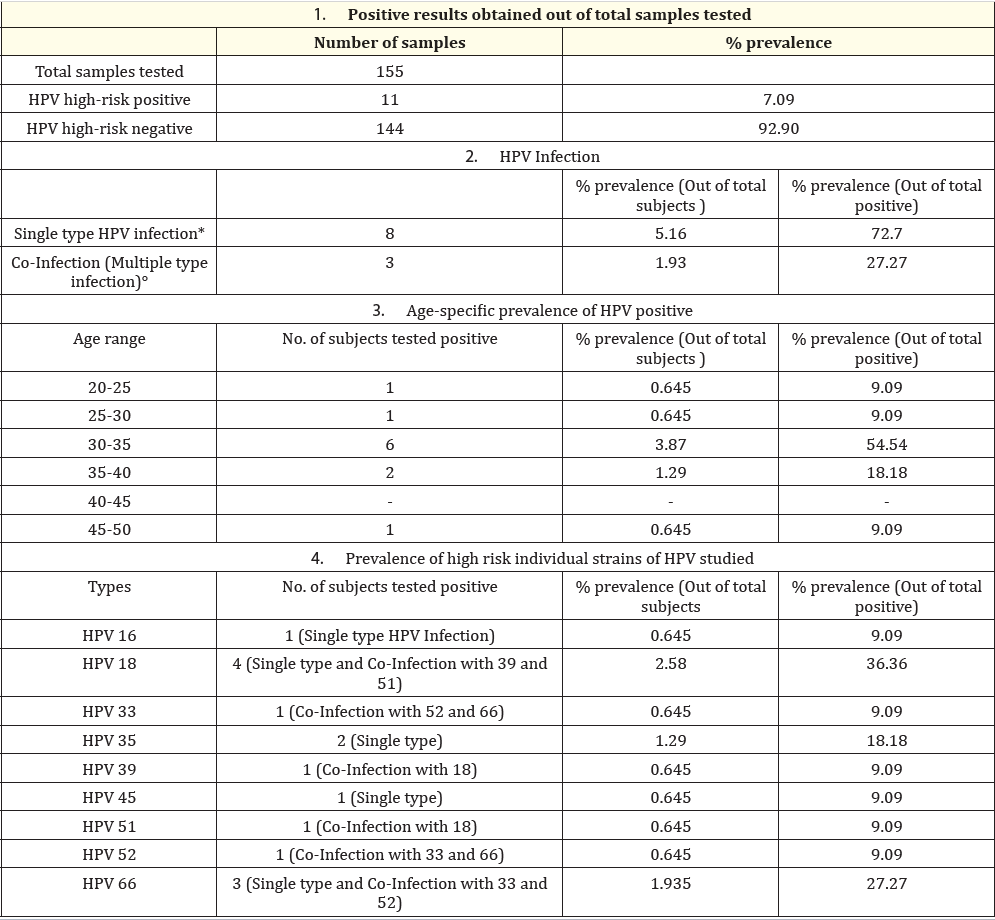
Table 1: Prevalence of high-risk HPV types among study population.
*Single-type HPV infection is the infection that has occurred a single time in the positive population
°Co-infections indicate that more than one type of strain is present.
As shown in the part 2 of the table, single infections of high-risk HPV types were observed in 72.7% of total positive samples. Co-infections also were 27.27% prevalent indicating that not only the common type but also other types of HPV high risk should be screened in the population and similarly vaccination for these HPV types should be developed and implemented based on population studies [10].
Out of the total 155 subjects studied we found that either single or HPV co-infection was highest (3.87% prevalence out of total subjects and 54.54% prevalence out of total positive) in the age group of 30-35 years. This was followed by the subjects in the age group 35-40 years (1.29% prevalence out of total subjects and 18.18% prevalence out of total positive). The lowest was observed in the age group of < 30 years and > 40 years.
HPV high-risk type 18 was the most prevalent high-risk type observed in the study group contributing to 36.3% of positive samples and this was followed by HPV high-risk type 66 which contributed to 27.27%. HPV 33 high risk was also seen as prevalent contributing to 18.18%. Multiple HPV high-risk infections were also observed in the studied population. Among multiple infection cases, 1 subject was infected with 3 types of HPV (52,33,66), and two subjects were infected with 2 types (18, 39; 18, 51).
HPV 18 was found to be highly prevalent in single and co-infection types of the positive population.
Cervical cancer has a significant global impact, ranking fourth in both new cases and deaths. However, the situation in India is particularly concerning, where it is the second most prevalent female cancer, constituting 10% of all diagnosed female cancers. This high prevalence is associated with lower socioeconomic status and a widespread presence of the human papillomavirus (HPV), particularly types 16 and 18, which are responsible for approximately 80% of cervical cancer cases reported in India [11]. Prolonged HR-HPV infection leads to the development of abnormal changes in the cervical epithelium, which can progress to a precancerous state and ultimately cancer [12]. As the quadrivalent HPV vaccine (Gardasil, Merck Sharp and Dohme) only prevents infection by high-risk genotypes 16 and 18, Observational research evaluating the incidence of other high-risk genotypes may help us develop new vaccines targeting the most prevalent genotypes by region, enhancing coverage against non-16/18 genotypes [10]. This study provided additional information on the relative distribution of HR-HPV genotypes other than HPV-16 and -18 in the North East population. The overall prevalence of HR-HPV infection in women screened from first-level health center in Itanagar was 7.09%. The most prevalent HR-HPV genotypes in women attending the Ram Krishna Hospital in March-July 2024 were HPV-18, HPV-66, and HPV-35. Our results showed that HPV 66 infection had a significant prevalence (27.27% of all the positive subjects) than HPV-16 (9.09%) in the studied population. The genotype distribution pattern showed a higher prevalence of single-type infection than co-infection. Senapati., et al. [13] reported that had a 2.9-fold increased risk of invasive cervical carcinoma concerning other genotypes; thus, multiple HR-HPV infections could increase the risk of cervical cancer.
The distribution of HR-HPV genotypes showed that the most prevalent genotype HPV-18 predominated in patients in the age group of 30-35 years. The main strength of this study is to determine the prevalence of non-16/18 HPV infections in first-level health center in Itanagar. The main limitation of our study is the small sample size. Additionally, the studied population is not representative of other regions of the nation or the world, so these results are not generalizable to other populations. In conclusion, the prevalence of single and multiple HR-HPV infections revealed a significant predominance of non-16/18 multiple HR-HPV infections. Finally, HPV-18 was the most prevalent genotype in the studied population. We emphasize the importance of promoting awareness, early detection, and improving the healthcare system.
We would like to thank Ram Krishna Mission Hospital for helping in sample collection.
There is no financial interest or any conflict of interest.
Copyright: © 2024 Preeti Arora., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.