Alain P Bourcier1*, Gilbert Naccache2 and Laurent Mamy3
1Pelvic Floor Rehabilitation Unit - Centre Médical Victor Hugo, Paris, France
2Urodanamics Unit - Centre Médical Victor Hugo, Paris, France
3Perineum Healthcare - Saint-Maur des Fossés, France
*Corresponding Author: Alain P Bourcier, Pelvic Floor Rehabilitation Unit - Centre Médical Victor Hugo, Paris, France.
Received: August 04, 2023; Published: September 24, 2024
Citation: Alain P Bourcier., et al. “Pelvic Floor Disorders and Body Changes After Childbirth: Postpartum Rehabilitation". Acta Acta Scientific Women's Health 6.10 (2024): 33-48.
Carrying and giving birth to a child can affect the pelvic floor in different ways and cause various undesirable symptoms. Fortunately, there are treatments for pelvic floor issues that can arise after childbirth. Mothers are affected differently by childbirth and the most frequent complications include: urinary incontinence, pressure in the pelvic area, pelvic organ prolapse, trouble passing stools, fecal incontinence. pelvic pain, modifications of the musculoskeletal system as well as body changes.
Keywords: Obstetric Injuries; Pelvic Floor Disorders; Body Changes
Pelvic floor disorders (PFDs) are common health problems and are mainly related to vaginal delivery, pelvic surgery, chronic straining and ageing. Vaginal childbirth is the most common mode of delivery and it has been associated with increased incidence of PFDs later in life. This usually arises from trauma to levator ani muscle (LAM), endopelvic fascia and pudendal nerve (Figure 1). However, not all women who deliver vaginally develop lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) or faecal incontinence (FI); some are more likely to be at risk than others. If such “at risk” group can be identified, then prevention might be possible. Apart from the PFDs there are also other dysfunctions that must be taken into consideration. Among these the most frequent are genito-pelvic pain, lumbopelvic pain and musculoskeletal disorders (MSDs). Changes in maternal hormones, both during and after pregnancy, can result in tissue changes that cause excessive joint motion as well as postural changes. Physical therapy plays an important role in the postnatal period through a combination of specific treatments such pelvic floor physical therapy/physiotherapy and physical therapy/physiotherapy techniques for MSDs, both therapies can improve health outcomes for new mothers in the postnatal period.
Although the pathophysiology of PFDs is multifactorial, two of the main associated factors are the gestational period and the delivery route. The pregnancy period demands several modifications. During pregnancy, the physiological, anatomical, and hormonal changes must occur to the female body as well as a lot of stress on the LAM. The increase in body weight and uterine size leads to a high abdominal pressure that overloads pelvic floor structures. A possible cause of the long-term effect of pregnancy on pelvic floor function is the influence of pregnancy hormones on connective tissues. The hormone relaxing has a putative role in connective tissue remodeling. This occurs in the uterine body, cervix, pelvic joints and perineal tissues in late pregnancy and parturition. Pregnancy triggers a wide range of changes in a woman’s body leading to various MSDs. Most commonly reported musculoskeletal discomforts by pregnant women as well as childbearing women (CW) are low back pain and symphysis pubis pain. The risk factors for PFDs are vaginal childbirth and parity which appear to be important risk factors for the development of PFDs, such as SUI and POP. Obstetrical exposures, such as operative vaginal delivery, prolonged second stage of labor, fetal macrosomia and perineal lacerations, often coexist. Trauma to the pelvic support system, denervation injury, ischemia, combined neurovascular injury and defective soft-tissue remodeling are some of the mechanisms that may explain the association between vaginal delivery and PFDs. Injury to the LAM is attributed to vaginal delivery resulting in reduced pelvic floor muscles (PFM) strength, enlargement of the vaginal hiatus, stress urinary incontinence (SUI), pelvic organ prolapse (POP) and anal sphincter defects. Most damage of the pelvic floor obviously occurs during first delivery and objective findings have demonstrated pudendal nerve damage mostly found after forceps delivery.
Increased duration of second stage of labor, third degree perineal tear, high birth weight, trauma to the pudendal nerve through stretch injury have been well documented. Vaginal delivery results in significant pelvic floor tissue stretching and pudendal nerve damage and there is a direct link to the PFM being impacted. Blomquist and coll [1] describe the incidence of PFDs after childbirth and identify maternal and obstetrical characteristics associated with patterns of incidence 1 to 2 decades after delivery. Recruitment was based on mode of delivery. They concluded that compared with spontaneous vaginal delivery, cesarean delivery was associated with significantly lower hazard for USI, overactive bladder (OAB), and POP, while operative vaginal delivery was associated with significantly higher hazard of FI and POP. A larger genital hiatus was associated with increased risk of POP independent of delivery mode. Environmental etiology can only explain part of patient cases with SUI, but it is impossible to explain the occurrence of SUI in women who are not pregnant and have not given birth, while most of the multiparous women show no symptoms of SUI. Epidemiological studies suggest that SUI has a familial hereditary tendency. The etiology and pathogenesis of SUI are complex and to be involved with environmental factors, genetic factors and cross-cutting factors between the two.
Pregnancy can affect the lower genitourinary tract through physiologic changes, besides neurologic and vascular compression and compromise, and muscle strain are inevitable during childbirth. Hormones during pregnancy also contribute to the loosening of ligaments and muscles. It has been demonstrated that pregnancy itself, through mechanical changes of the pelvis and hormones, can be a significant risk factor for PFDs. Groutz and colleagues concluded that labor itself, not just delivery, may play an important role in the development of postpartum urinary incontinence, performed a prospective cohort study of 363 primiparous Israeli women [2]. The prevalence of SUI was similar in women who had vaginal deliveries and women who underwent cesarean section for obstructed labor (10.3% and 12%, respectively), besides they found that only 3.4% of women who underwent planned cesarean section complained of SUI during that postpartum year performed. Until recently, women were expected to deliver their babies vaginally if their pregnancy was considered to be low risk. But many women get concerned about the issues of UI or PFDs before giving birth and tend to deliver by C-section. Yared., et al. reported a retrospective observational cohort study including forty primiparous women undergoing cesarean delivery were involved, divided into 2 groups: elective cesarean and cesarean delivery for arrested second stage of labor [3]. Cesarean delivery cannot be proposed to women who fear to suffer from SUI post-partum. However, it should be done if the cervix fully dilated for > 2hours in order to decrease the risk of SUI. Nevertheless, there are other opinions who state that an elective cesarean section (eCS) without labor is thought to protect against pelvic floor dysfunction. Although short-term occurrence of any degree of postpartum SUI is reduced with cesarean section, severe symptoms are equivalent by mode of birth. Cesarean section is associated with a reduction in the risk for PFDs, although the routine performance of this procedure does not eliminate the risk for dysfunctions because the pathophysiology is multifactorial. C-section is associated with a reduction in the risk for PFDs, although the routine performance of this procedure does not eliminate the risk for dysfunctions because the pathophysiology is multifactorial. Cesarean delivery is associated with a higher rate of injury to abdominal organs (bladder, bowel, blood vessels), infections (wound, uterus, urinary tract), and thromboembolic (blood clotting) complications than vaginal delivery. Women with complaints of decreased strength of pelvic floor muscles had avulsion of the LAM, found after evaluation by means of translabial ultrasound. In addition, 1/3 of women with a LAM injury have decreased muscle strength. Although these PFM damage were first described using magnetic resonance imaging (MRI), three-dimensionl transperineal and endovaginal ultrasound has emerged as a more readily available and economic alternative to identify LAM morphology. The study of Li and coll. [4] aimed to evaluate the contributions of LAM injury, vesical neck movement, and urethral sphincter dysfunction observed on MRI towards SUI after vaginal delivery on fifty primiparous women after 6 months of delivery (15 with SUI and 35 without) and 35 nulliparous.
The MRI findings revealed that de novo SUI was associated with major LAM injury, vesical neck downward movement as well as urethral sphincter dysfunction. Vesical neck funneling on sagittal images can be treated as a valuable predictor for SUI. Constitutionally/genetically weak connective tissue and collagen might represent another risk factor. SUI is present in a significant number of nulliparous and pregnancy may adversely affect connective tissue biomechanics. The genetic and environmental factors contribute to the occurrence of SUI and POP. Lince., et al. found, In the systematic review, a substantially greater likelihood of SUI in family members with women with POP compared with women without POP, indicating that genetic predisposition plays an important role in the development of POP [6]. With the advent of modern imaging techniques, trauma to the PFM has gained a lot of interest and there is evidence that women with POP have an underlying LAM avulsion (Figure 1). LAM avulsion injury occurs occultly during childbirth, most commonly during operative vaginal deliveries and have long term sequelae for pelvic floor health (Figure 2). This avulsion occurs mainly during the first vaginal delivery by stretching and tearing of the muscles. Diagnosis of LAM avulsion should be suspected after operative vaginal delivery, obstetric anal sphincter injury (OASI) and at prolapse assessment. There is varying evidence for antepartum risk factors associated with LAM avulsion: increased maternal age, lower BMI, bladder neck descent for prediction of LAM avulsion. Clinically, palpation of the LAM insertion is done using the index finger of the clinician's dominant hand and the two modalities used in the diagnosis of LAM avulsion are ultrasound scan and imaging MRI. Chan and coll. evaluated the morphological outcome of LAM avulsion 3-5 years after a first delivery and to assess the effect of a second delivery on this condition [5]. They concluded that the risk of developing new LAM avulsion after a second vaginal delivery is low (0.9%). Vaginal laxity, a symptom frequently encountered in parous women and vaginal looseness is a subjective and self-reported sexual health concern. Evidence suggests that having multiple vaginal deliveries can increase the risk of vaginal fatigue and incomplete recovery of pre-pregnancy vaginal tightness. Vaginal laxity is a condition that is distinct from POP, but can sometimes be confused with it and with vaginal looseness the tissue becomes relaxed and stretched with feelings of reduced tightness. Auditory passage of vaginal air (embarrassing vaginal wind) is also a symptom reported in women with PFDs. Millheiser., et al. hypothesized that introital laxity leads to loss of physical sensation and the development of sexual dissatisfaction during vaginal intercourse among 50 parous women ages 25-55 years of age who had experienced at least one vaginal delivery [6]. They candidly described body image changes following childbirth and the complexity of physical and emotional consequences due to vaginal laxity (e.g., reduced vaginal sensation, difficulty reaching orgasm). Among the respondents who represented a 30-year age range from 25 to 55, approximately half expressed some degree of concern for “looseness” of the vaginal introitus. Gaping vaginal opening and stretched out internal tube of vaginal space that typically occurs after vaginal birth with obstetric risks factors, altered genital sensation during sexual intercourse, and reduced sexual satisfaction. Dominoni., et al. investigated the relationship between delivery and genital appearance in order to determine whether the mode of delivery changes the genital perception of the woman and, in doing so, influences their acceptance [7]. They enrolled 365 women for evaluation, divided into three groups: spontaneous vaginal delivery (80.82%), operative vaginal delivery (9.86%) and cesarean section (9.31%). They concluded that the mode of delivery may influence the genital perception and appearance of genitalia without a decrease of sexual life and daily activity in childbirth. As a component of PFDs, POP which is a common health problem affecting about 30% of the women between 20-59 years of age and more than half of the women over 50 years of age attending to the clinics is the most common surgical indication following hysterectomy. There are multiple factors: racial differences (more in the white race); connective tissue damage (Marfan syndrome, Ehlers-Danlos); ligamentous hyperlaxity (perineal relaxation syndrome in young nulliparous women); pregnancy (muscle relaxin effect); childbirth (tear of the perineum, forceps, high weight of the newborn, damage to the pudendal nerve); overweight and obesity (BMI> 30). POP in pregnancy is a rare condition with decreasing incidence and improved management and outcome world-wide recently. Little has been known about the changes that occur in the pelvic floor during pregnancy. Due to the impact of these changes either on the present pregnancy, or in future pregnancies, the need to document and to ascertain specific alterations from the normal becomes very apparent. The growing number has amplified the interest in determining their pathophysiology in relation to pregnancy. The need to evaluate all CW during prenatal examination for the presence of a prolapse cannot be overemphasized. The impact of the prolapse and its implications to a pregnancy should be studied further for formulation of better treatment modalities, and in the future, prevention. About half of women who had anal sphincter laceration and repair at delivery will experience some changes related to their bowel control. Even women who did not have direct anal sphincter damage at delivery may notice some bowel changes. These changes can include bowel urgency or FI. Bowel urgency means that there is very little time (five minutes or less) between the first urge to have a bowel movement and the need to pass stool. FI includes involuntary leakage or loss of control of gas, liquid stool, mucous, or solid stool. Bowel urgency and incontinence to gas are particularly common in the first few months after vaginal delivery. Urinary urgency and incontinence are also very common during this time. Incontinence of stool and flatus are frequent complications of childbirth and are more common than was previously believed. FI is associated with forceps delivery and anal sphincter laceration. Anal sphincter laceration is strongly predicted by first vaginal birth, median episiotomy, and forceps or vacuum delivery but not by birth weight or length of the second stage of labor. Mac Arthur and colleagues investigated persistent FI after birth and association with delivery mode history and quality of life in a twelve-year longitudinal study [8]. Prevalence of persistent FI was 6.0%; 43% of 12-year responders who reported FI at 3 months also reported it at 12 years. This large longitudinal study has demonstrated the persistence of FI and flatus incontinence many years after birth.
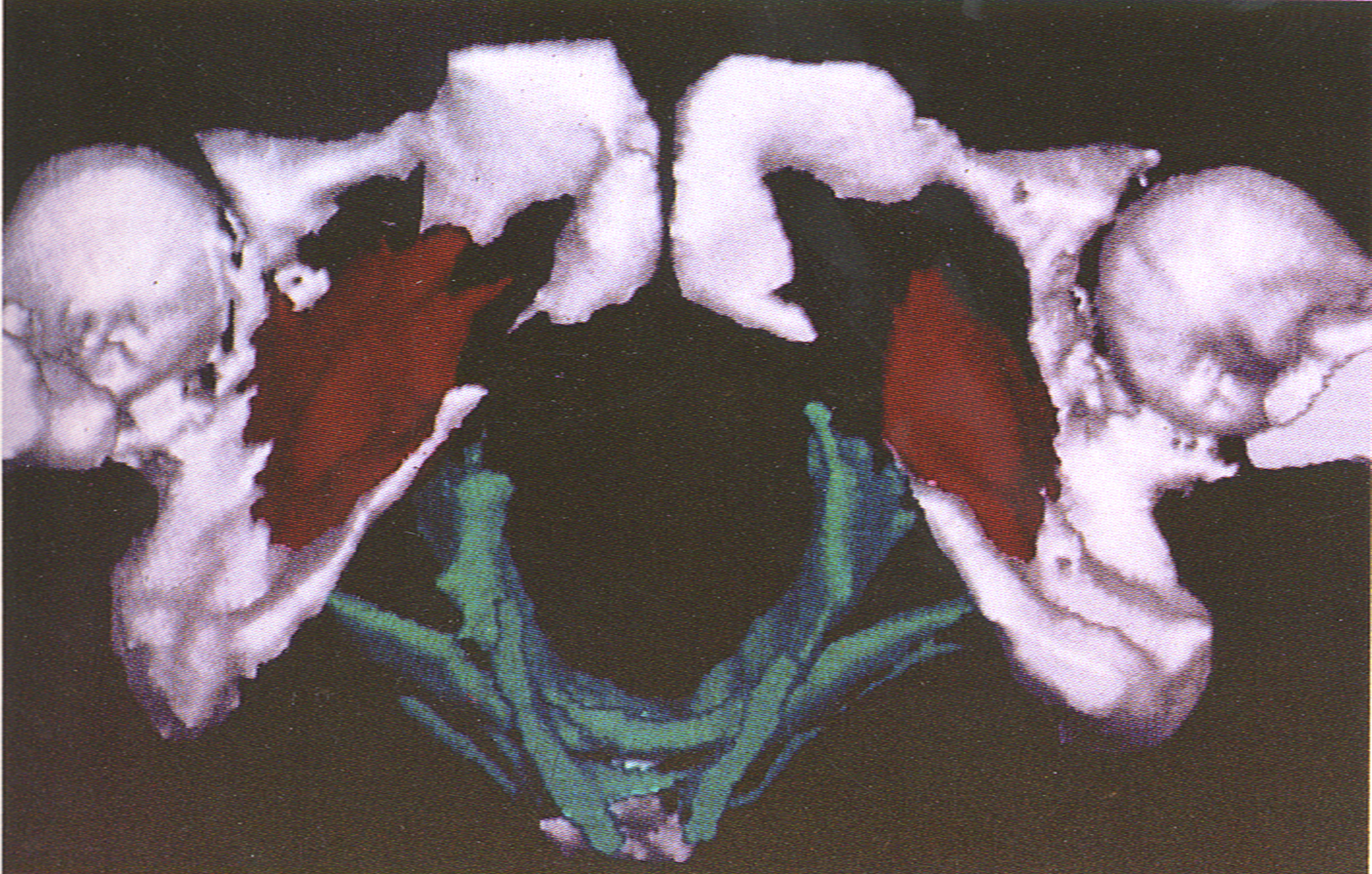
Figure 1: The 3-dimensional models determine LAM volume, shape and hiatus width, distance between symphysis and levator sling muscle; The obturator internus muscles are bilaterally connected to bony pelvis.

Figure 2: Levator avulsion can be diagnosed reliably by MRI evaluation and have shown an association between LAM avulsion and the development of pelvic floor prolapse in later life. Women have a higher incidence of LAM avulsion and show a wider urogenital hiatus and levator hiatus.

Figure 3: From top left to bottom right. (a)- The diastasis rectus abdominis or a separation of the abdominal muscle bellies is frequent, due to expanding abdomen and hormonal changes that cause tissue laxity. (b)- Stretch marks in pregnancy are one of the most common cosmetic concerns among child-bearing women. They are narrow, streak-like lines that can develop on the surface of the skin. They can be pink, red, purple or brown, depending on the skin color. (c)- C-sections can cause scarring and in some women, these scars become thick, raised, and red. A keloid scar occurs when scar tissue extends beyond the original wound boundaries, typically due to an overproduction of collagen during the healing process. (d)- Varicose veins aren't exclusive to pregnancy, but pregnancy can signal their arrival or make them worse. Varicose veins of the legs are a more severe form of venous insufficiency. (e)- The most common musculoskeletal complaints in pregnancy and after childbirth are low back pain and/or pelvic girdle pain. These conditions often happen due to problems with how the muscles and joints of the back and the pelvis are working.

Figure 4: From top left to bottom right. (a)- Manual therapy involves the PT using hands-on pressure and massage, either externally or internally, on the muscles of the pelvis. It is useful for improving blood flow to the affected muscles, as well as helping those muscles to stretch and relax. There are three techniques that can be applied to the pelvic floor, i.e. flat, deep and pincer palpation. (b)- The PFM form the base of the group of muscles commonly called the 'core'. These muscles work with the deep abdominal (tummy), back muscles and the diaphragm (breathing muscle). While these exercises are pelvic floor, it is important to consider the number of repetitions, intensity, number of sets, length of rest and activation of the PFM. (c)- Biofeedback technique involves placing small devices or surface electrodes in addition of abdominal internal or external control. These devices provide visual and auditory stimuli, providing the patient with feedback as to how well contracting their PFM. (d)- Extracorporeal magnetic stimulation is a non-invasive (neither vaginal nor anal probe). The impulse elicit activity in the pelvic floor muscles, which consequently contract and relax in response to each impulse. The technology aids in the rebuilding of strength and endurance. (e)- A magnetic biofeedback trainer scans and records the activities of the pelvic muscles through a special sensor integrated in the seat. Muscles activities are measured by the sensor and visualized on the screen.
The findings of this study have some implications for practice. Women who deliver exclusively by caesarean section have no lesser likelihood of persistent FI than those who deliver vaginally. That just one forceps delivery increases the likelihood of persistent FI might be justification to favor vacuum extraction. The aim of the study of Shei B., et al. was to explore whether women who had delivered only vaginally were at greater risk of anal incontinence than nulliparous women and women who had undergone cesarean sections only [9]. Age, educational level, diarrhea, constipation, birthweight, and OASIS increased the risk of anal incontinence in all women. The authors concluded that women with vaginal deliveries complicated by OASIS are at increased risk of anal incontinence. However, no increased risk of anal incontinence was found in nulliparous women or women who had cesarean sections only or vaginal deliveries not complicated by OASIS.
In nulliparous women, the most common risk factors for PFDs are obesity, childhood enuresis and practice of sports with high-impact exercise [10]. With a prevalence of 18– 75%, SUI is the most common type of PDFs during pregnancy and is highest in the third trimester. The factors behind UI in pregnancy are not fully understood, but anatomical changes in the pelvic floor, the weight of the pregnant uterus and hormonal issues have been suggested. This most likely related to hormonal and physical changes to the pelvic floor during pregnancy and vaginal delivery. Urinary incontinence before and during pregnancy was significantly associated with urinary incontinence three months after childbirth. SUI was also more common in the women with urinary incontinence three months postpartum. Vaginal childbirth is probably the most important factor in the aetiology of PFDs and results in the combination of some or all of the following conditions: UI, POP and FI. The identification of such women at risk should be achievable by appropriate history. A recent prospective cohort study was conducted by Rajavuori., et al. to investigate the incidence of UI during pregnancy and three months postpartum and determine the risk factors underlying UI. [11] 47 volunteer women were recruited from the maternity clinic of a tertiary hospital. The prevalence of UI during pregnancy was 39.5% and three months after childbirth 16.1%. The authors concluded that women with UI before or during pregnancy and who are primiparous are at increased risk for postpartum UI. Wilson and coll. propose a scoring system (UR-CHOICE) to predict the risk of future PFD based on several major risk factors: UI before pregnancy, ethnicity, age at birth of first child, body mass index, family history (mother and sister) of PFDs and baby’s weight and maternal height (baby >4kg <160cm) have been identified for subsequent PFDs risk [12]. This scoring system will help with counselling for women regarding PFDs prevention. New evidence exists for the presence of risk groups for obstetric pelvic floor trauma including anal sphincter injury (OASIS), urinary incontinence and pelvic organ prolapse and this highlights the need for identification as part of routine antenatal care. Even though the evidence was divided into non-obstetric and obstetric risk factors the committee [12] noted that in clinical practice they would be divided into modifiable and non- modifiable factors so that risk management can be planned and agreed with the woman. There are 2 types of risk factors:
Preventative measures can then be put into practice. The presence of risk groups highlights the need for identification as part of routine antenatal care: taking an history for pre-pregnancy and antenatal incontinence; referring such women for supervised PFMT antenatally; midwives might be the ideal group to offer this to all women in pregnancy after being trained; identified as high-risk factors could be referred for PFMT with a physiotherapist or continence advisor postnatally.
It was in 1978 that Bourcier organized the basics of perineal rehabilitation program which was instituted in France in 1985 and paid for by the “Sécurité Sociale”. Women are prescribed 10 sessions of “Rééducation périnéale post-natale”, in the form of pelvic floor muscle exercises (PFME) by manual internal techniques, biofeedback (BF) and electrical stimulation (ES) with a probe free of charge. French obs/gyn doctors prescribe postpartum sessions and it is covered as part of the country’s government health care plan.
Routine postpartum PFR in France has long been the envy of many physiotherapists in other countries but had received some funny comments from some female journalists who delivered in France [13]. Among the best known are: in The Guardian "We will teach you to make love again", in The Telegraph "The French Government wants to tone my vagina". Bonnie Rochman comments "Why France pays for postpartum women to re-educate their vagina. "Have you heard about the French and their vaginas ", Emily Mazo-Rizzi, an American who has lived in Paris for nearly 20 years, happily took advantage of this government-funded rehabilitation when her first baby was born in 2012. "Why French Women Don’t Pee Their Pants ", in France, any woman who has delivered a baby gets a ‘prescription’ for 10 free physiotherapy/rehabilitation sessions to “re-educate” their pelvic floor that supports your pelvic organs, helps you have enjoyable sex and stops you from peeing in your pants (and lots of other things too!). Lyndey Graham from The Mummy Mot said in 2018 that we don’t have such a thing on our NHS here, some NHS trusts offer a bit of a Physiotherapy service to look after women, most however are lucky to get a quick check up from their GP/Midwife at 6 weeks. It is true that these services are routinely provided by “kinésithérapeutes or sages-femmes”, after 6 weeks postpartum, regardless of symptoms. France seems to be one of the only countries that supports such a program. We wonder if this is a true reality and wanted more data on this assertion. This was the reason of the first study of Bourcier and coll. based on the situation in other countries with regard to the approach of postnatal management [14]. In 2017, 56 international experts from 28 countries selected according to their interest in this field and have already published articles, filled out a questionnaire which included 21 items on 5 main topics. The main questions were: Do you recommend pelvic floor rehabilitation (PFR) after delivery ? When do the childbearing women (CW) start PFR in the early postpartum? Number of sessions for each individual? What type of pelvic floor muscle training (PFMT) is used? Do you propose ES) and/or BFB in office therapy or home care? Is the treatment covered by your national social security agency? The main responses were: PFR is provided in 71% for vaginal birth, but only for symptomatic CW; The PFR starts 6 weeks in 85% or 8 weeks in 34%; Number of visits is 1 to 6 sessions in 66%; At the first visit, they have a pelvic floor muscles assessment in 100%; The PFMT is undertaken by a skilled PT including individualized PFMT with a home exercise program 75%; ES and BF might be included as a second-line intervention; The reimbursement by private health insurance (partly covered only) is in 75% and CW often had to contribute to the cost of their therapy. Brook, as President of the International Organization of Physical Therapists in Women’s Health (IOPTWH), was invited to present at the 7èmes Journées Francophones de Kinésithérapie in Montpellier, France, in 2019. She was asked to speak about the current “state of play” in postpartum physiotherapy [15].
25 countries were members of IOPTWH and delegates were invited to answer the following questions: Is postnatal/postpartum physiotherapy standardized across the country? 48% of the responders stated that there is no standardized national approach; If there is standardized care, what does it include? Some responders mentioned group sessions for women postpartum, while others saw women on a one-to-one basis one or more times before they were discharged from hospital; Who pays for the treatment? Free postpartum physiotherapy was available in 44% of the countries surveyed. Women could access private treatment in most or all countries; this was either covered by insurance, subsidized by the state (24%) or self- funded. Both the present IOPTWH international survey and that of Bourcier., et al. suggested that this is already current practice in many countries [14]. Brook declared that physiotherapy interventions (e.g. diastasis recti abdominis, posture and a return to fitness activities) are worthy of further consideration.
The reimbursement for the PFR after childbirth is rarely covered and one should send a bill of fees for rehabilitation services. Certainly but interestingly, in many countries, there is an interest in postpartum body changes. These transformations are not systematic and can be isolated or associated with perineal pathology. In summary: PFR is proposed 6 weeks after vaginal delivery; the number of sessions is limited to 6, on weekly basis and between 30 to 45 minutes, under a control of a trained physiotherapist (physical therapist); the therapy is mostly PFMT and Kegel unsupervised exercises as home care; BF and ES are not first line treatments; health insurance covers rarely these services and the amount to pay for this therapy depends on the coverage from national health insurance and private health insurance. Currently, there are no clear guidelines for new mothers on prevention and avoidance of PFDs after childbirth. Therefore, a multidisciplinary strategy to make women aware during and after their first pregnancy of the importance of PFMT as a normal part of healthy lifestyle and general wellbeing may be necessary. It seems important to propose adequate recovery/rehabilitation guidance in order to get a consensus about the management of postpartum care.
Pelvic pain refers to pain in the lowest part of the torso, in the area below the abdomen and between the hip bones. The pain may be sharp or crampy and may come and go. It may be sudden and excruciating, dull and constant, or some combination. It can occur normally as the bones and ligaments shift and stretch to accommodate the fetus. Pelvic pain differs from abdominal pain, which occurs higher in the torso, in the area of the stomach and intestine. However, sometimes women have trouble discerning whether pain is mainly in the abdomen or pelvis. Causes of abdominal pain during pregnancy are usually not related to the pregnancy. During early pregnancy, pelvic pain may result from disorders that are related to the digestive tract and urinary tract, which are common causes of pelvic pain. These disorders include the following: infection of the digestive tract, irritable bowel syndrome, and urinary tract infections. The pain during pregnancy is sometimes called pregnancy- related symphysis pubis dysfunction (SPD) but health professionals now call it Pelvic Girdle Pain (PGP) because it affects all the joints of the pelvis not just the one called the symphysis pubis. The incidence of diagnosed GPD is about 1 in 300 pregnancies, though some experts think that up to 25 percent of all pregnant women will experience SPD (though not all have it diagnosed). PGP is a collection of uncomfortable symptoms caused by a stiffness of the pelvic joints or the joints moving unevenly at either the back or front of your pelvis. For some women in pregnancy the pelvic joints become stiff or less stable and affects up to 1 in 5 women. The pain can range from a dull ache to severe pain. Most sufferers are in the mild to moderate category. Women with PGP may feel pain: over the pubic bone at the front in the center, roughly level with hips; across 1 or both sides of the lower back; in the area of perineum. The pain can be worse when walking, going up or down stairs, turning over in bed and moving the legs apart.
They are potential causes of PGP. Wang., et al. studied the association between relaxing and peripartum pubic symphysis separation and evaluate other factors that might affect this association [16]. 54 women were enrolled with 15 exhibiting (observational group) and 39 not exhibiting (control group) peripartum pubic symphysis separation. They concluded that serum relaxing levels and neonatal weight were associated with the occurrence, but not the severity, of peripartum pubic symphysis separation. As the fetus grows during pregnancy, the center of gravity shifts forward and remains forward in the post-partum period. This typically results in a forward rotation of the pelvic bones, leading to increased load and decreased functional stability and increased wear and tear of the SI joints. Traumatic cause may be due to direct injury of the pelvic floor muscle or injury to the nerves that innervate the pelvic floor muscles during pregnancy and/or delivery. Pelvic pain during the postpartum period is common and may persist for months or years postpartum. It can also be intermittent, made worse by certain positions or activities, like coughing, lifting something heavy, or certain sex positions. The pain can worsen when walking and doing weight-bearing activities, particularly those that involve lifting one leg like climbing stairs, getting dressed, getting in and out of a car, or even turning over in bed. Weight gain of a pregnant woman and a shift in the center of gravity forwards causes mechanical changes mainly in the pelvic girdle and lower limb joints.
There is a tendency for deepening of lordosis in the lumbar spine, forward inclination of the pelvis, and formation of flexion contractures in the hip joints. Under hormonal stimulation during pregnancy, there is widening of the symphysis pubis and the sacroiliac joints. It is usually noticed after delivery but can be observed up to six months postpartum. Pain is often located in the anterior pelvis and can radiate down the anterior thigh, hip, abdomen, and lower back. Patients will often exhibit tenderness to palpation of the pubic symphysis and symptoms will be exacerbated with specific movements such as the transition from lying down to sitting and standing, climbing stairs, or lifting heavy loads. Low back pain and sciatica is one of the most common complaints during pregnancy is back pain. In fact, it's estimated that more than half of all women experience some degree of back discomfort. Most back pain is related to the physical changes that happen during pregnancy, including hormones, changes in the center of gravity, and posture. Unfortunately, it typically gets worse as pregnancy progresses. The causes are: the hormones relaxing and progesterone relax muscles and loosen ligaments and joints, especially in the pelvic area; the extra weight and body changes in pregnancy along with these loosened joints and ligaments can cause discomfort and even lead to injury; as the uterus grows and becomes heavier, the center of gravity changes the weight of the baby and weakening of belly muscles pulls the lower spine forward, adding strain to back muscles. Back pain during pregnancy is a frequent clinical problem even during the early stages of pregnancy. Back pain during pregnancy typically takes the form of aches, stiffness and soreness in the upper or lower back and hips that can sometimes extend into the legs and buttocks. The back pain started early in pregnancy and increased over time. It can persist or sometimes worsen as the second trimester progresses and especially in the third trimester, up until you give birth. Back pain starting during pregnancy may be a special entity and may have another origin than back pain not related to pregnancy. Mogren et coll. investigated prevalence and risk factors for low back pain and pelvic pain (LBPP) during pregnancy [17]. The prevalence of LBPP during pregnancy was 72%. Most cases reported both anterior and posterior pain. They concluded that a majority of pregnant women report LBPP. In most cases, sciatica happens when the sciatic nerve gets compressed by bulging, slipped or ruptured discs, or a narrowing of the spinal cord (spinal stenosis). But rarely, women experience sciatica as a short- term side effect of pregnancy. The main causes are: weight gain and increased fluid retention which can put pressure on the sciatic nerve compressing it; expanding uterus might also press down on the sciatic nerve in the lower part of the spine; position of the baby's head which can rest directly on the nerve when he starts to settle into the proper birth position in the third trimester.
Pregnancy and birth put intense pressure on the organs and tissues in the pelvis, often causing swelling, bruising, and soft tissue tears. Under the intense pressure of a baby’s head pushing up against the vaginal opening during labor, the perineum can get swollen and sometimes even tear, leading to vaginal pain. There are different causes postpartum perineum pain:
Paterson., et al. investigated the prevalence and characteristics of all types of genital and pelvic pain in the second year postpartum, and to explore risk factors for their persistence [18]. Almost half of the 114 participants (reported a current (18%) or resolved (26%) episode of genital or pelvic pain lasting 3 or more months. This pain was described at various locations (e.g., vaginal opening and pelvic area), as moderate in intensity and unpleasantness, and most often as burning, cutting, or radiating. Their conclusion was that postpartum genital and pelvic pain persists for longer than a year for a significant percentage of mothers. Women with a history of other chronic pain appear to be particularly vulnerable to developing persistent genital or pelvic pain. Rosen et coll. reviewed the available evidence to compare and contrast the prevalence, risk factors, and repercussions of postpartum genito-pelvic pain vs dyspareunia [19].
The prevalence of postpartum pelvic pain is much lower than that of postpartum dyspareunia.
Postpartum pelvic pain and dyspareunia are associated with impaired sexual functioning. They suggested that this approach should be spearheaded by a multidisciplinary group of researchers of diverse and relevant expertise, including obstetricians, gynecologists, anesthesiologists, and psychologists. The objective of the study of Novo., et al. was to estimate the prevalence of dyspareunia and SUI during pregnancy and after delivery, in addition to evaluating possible associated risk factors [20]. The prevalence of SUI and dyspareunia after delivery were 20.4% and 23.4% respectively. The presence of dyspareunia during pregnancy (adjusted prevalence ratio PR 2.1), breastfeeding (PR 1.2), and having a history of episiotomy were all variables associated with the presence of dyspareunia after delivery. These variables should be included in the clinical history of every pregnant woman.
Pelvic bone problems are painful but they usually get better on their own. Postpartum coccydynia is pain that appears as soon as a sitting position is adopted after delivery. Coccyx morphology, body mass index, instrumental delivery, and short perineum in women with difficult delivery are risk factors. During labor the lower back, sacrum and coccyx have to move and tip to allow baby to engage and then come out. The coccyx can commonly be injured or disrupted during birth, this is far more common with labors that have been going on for a long time, prolonged pushing, forceps and ventouse deliveries. The altered load, strain or damage through the PFM is a huge contributor to coccyx pain. Although childbirth is a well- known cause of coccydynia, this condition has not been studied previously. Maigne., et al. explored the characteristics of postpartum coccydynia and identify risk factors [21]. A series of 57 women was analyzed and compared with a control group of 192 women suffering from coccydynia due to other causes. The deliveries had often been performed with instruments (forceps 50.8% vacuum-assisted deliveries: 7.0%). Luxation of the coccyx was observed in 43.9% of the cases and 17.0% of the controls. A body mass index >27 and ≥2 vaginal deliveries were associated with a higher prevalence of luxation of the coccyx. They concluded that postpartum coccydynia is often associated with a difficult delivery, with the use of forceps in 50.8% of cases.
Pregnancy-induced biomechanical, hormonal, and vascular changes are likely to give rise to a wide variety of musculoskeletal problems. Fluid retention leads to compression of soft tissues in pregnancy. Consequently, a pregnant woman is susceptible to musculoskeletal injuries. Low back pain has been reported as the most frequent disorder. Joint laxity develops secondary to hormone level fluctuations. Fluid retention leads to compression of soft tissues in pregnancy. The purpose of the study of Kesikburun., et al. is to provide a comprehensive look at the musculoskeletal pain and symptoms experienced during pregnancy [22]. 184 women (mean age 30.9 ± 5.0 years) were enrolled. The most frequent musculoskeletal complaints during pregnancy were low back pain (70.7%), back pain (43.5%), hand–wrist (33.2%) and hip pain (32.1%). The results of the study suggest that numerous musculoskeletal problems may complicate pregnancy especially in the third trimester. MSK conditions include conditions that affect: osteoarthritis, rheumatoid arthritis, spondylarthritis, carpal tunnel syndrome; osteoporosis, traumatic fractures. Another common post-partum dysfunction is diastasis rectus abdominis (DRA) or a separation of the abdominal muscle bellies. Most women will experience some degree of abdominal separation during pregnancy. It is a common condition and often gets better in the first 8 weeks after having a baby. Abdominal separation is partly due to the pressure of the growing baby, and partly due to the hormonal changes that take place during pregnancy. Abdominal separation is more common in women who have had more than 1 child, are aged over 35 or who are having twins or triplets (or more).
Lifting objects, walking or performing everyday tasks; low back pain. Fei., et al. aimed to investigate the association with the severity of DRA for developing PFDs among women during the first year postpartum [23]. This is a retrospective cohort study which collected data from 229 postpartum women. Prevalence of DRA was 82.6% during the first postpartum year. The report shows that the relationship of the DRA and pelvic floor dysfunction has no connection, even with the severity of inter-rectus distance increasing.
Growing a baby is hard work for the body—it goes through enormous changes. While many of these changes or symptoms will disappear after delivery there are some parts of the body that may take longer to heal, or may stay changed. The body may have become wider during pregnancy. The ribs may have expanded, and the hips will often widen to make it easier for the baby to exit the birth canal. While many of these changes will disappear after having a baby, there are some parts of the body that may take longer to heal, or may stay changed. Weight gain in pregnancy varies greatly and is based on the BMI before pregnancy. Most pregnant women gain between 10kg and 12.5kg (22lb to 28lb), putting on most of the weight after week. The second trimester (weeks 14 to 27), is when the pregnant woman might begin to see that gradual weight gain. Much of the extra weight is due to the baby growing, but the body will also be storing fat, ready to make breast milk after the baby is born. Liang CC., et al. evaluate the effects of pre-pregnancy BMI on pregnancy outcomes, prevalence of urinary incontinence, and quality of life [24]. 2210 pregnant women who were divided into 4 groups according to their pre-pregnancy BMI: (<18.5; 18.5–24.9; 25–29.9; ≥30). They report that maternal pre-pregnancy overweight and obesity are associated with greater risks of preeclampsia, gestational diabetes, macrosomia and urinary incontinence. The breast has no muscle tissue, however they are attached via ligaments to the muscles of the chest wall. These ligaments stretch during pregnancy and don’t tighten again. This means that breasts will droop, and they may never be the same shape they were before pregnancy. Stopping breastfeeding suddenly could put at risk of engorgement, blocked ducts or mastitis. Right after giving birth, estrogen and progesterone levels drop, and prolactin, the hormone that helps to make breast milk, kicks in.
Postpartum period are: a visible bulge or "pooch" that protrudes just above or below the belly button; difficulty even bigger than they were during pregnancy. Breasts will be swollen, sore and engorged with milk for a couple days after birth. Most women experience breast changes after pregnancy, regardless of whether they breastfeed. In general, the breasts tend to revert to their original size when the body resumes its pre-pregnancy weight. However, the shape of the breasts may change permanently. Even if the breasts never return to their pre- pregnancy state, most of the changes are cosmetic, meaning that they are not a medical concern. Stretch marks, medically known as striae, can appear on the skin as red linear streaks. They are often present in people who are pregnant or overweight, or who have experienced rapid weight gain or weight loss. Stretch marks are narrow, streak-like lines that can develop on the surface of the skin. They can be pink, red, purple or brown, depending on your skin color. They are common in pregnancy, affecting around 8 out of 10 pregnant women. They usually appear on the tummy, or sometimes on the upper thighs and breasts, as your pregnancy progresses and the bump starts to grow. Shoe size can increase during pregnancy. Extra weight can flatten out the foot arch and the shoe size might increase. Hormone relaxing helps to relax the ligaments and bones and also relaxes the ligaments of the feet. This may cause the feet to flatten and spread out and increase the shoe size. These changes to the feet are permanent so it’s important that you find shoes that fit correctly after pregnancy. Varicose veins aren't exclusive to pregnancy, but pregnancy can signal their arrival — or make them worse. At the end of pregnancy, the uterus is large and compresses the inferior vena, especially when the pregnant woman is lying on her back. This large vein is the one that brings blood from the pelvis and legs to the heart. Its compression hinders this venous return and blood pressure increases in the veins and venules of the legs. Varicose veins of the legs are a more severe form of venous insufficiency. The veins under the skin dilate permanently under the pressure of blood that "stagnates" in the legs. Most often, in women who have never had them before, varicose veins disappear after childbirth. In some cases, varicose veins in the legs can rupture and cause bleeding. The veins in the legs are more often affected because they work against gravity, but the vulva (vaginal opening) or rectum can also be affected, leading to hemorrhoids. Pregnancy seems to increase the risk of varicose veins. These cause considerable pain, night cramps, numbness and tingling, make the legs heavy and painful and are quite ugly. Scar tissue after C-section are becoming more frequent. Globally, C-section rates have increased in recent decades, depending on the country. C-section occurs in different circumstances: in emergency when labor conditions require it to preserve the health of the mother and baby; scheduled when vaginal delivery is contraindicated for the mother and/or baby; of convenience. The unprecedented high rate of cesarean delivery make necessary awareness of the potential complications that are associated with repeat cesarean delivery Among these risks include increased adhesions, infections and wound complications. This occurs because there has been a break in the body’s tissues as a result of the C-section. The body produces more collagen, as part of the healing process. Collagen builds up where the tissue has been damaged, helping to heal and strengthen the wound. For a period of about three months or longer, new collagen continues to form and blood supply increases, causing the scar to become raised, lumpy and red. Although scars are permanent, they can fade over a period of up to two years. It is unlikely they will fade any more after this time. The density of adhesions can vary considerably and their size and location. probably influence clinical effects. The adhesions are particularly thick and dense after several caesarean sections. In a retrospective study of 542 patients it was shown that the percentage of women with adhesions increases with each caesarean section [25]. Women with intraperitoneal adhesions had more vascular, hyperpigmented, less flexible and raised scars confirming that these adhesions occur in people who have healing defects.
During pregnancy and postpartum, conservative therapy or PFR by pelvic floor muscles exercises (PFME) is the first-line intervention to treat SUI. Pregnant women are often instructed to perform PFME to prevent the development and treat symptoms of SUI during pregnancy. It is beneficial for all new CW to have their PFMs evaluated after they’ve been cleared to resume sex and physical activities. This kind of early intervention can help address any concerns, and ultimately enable new moms to return to functional and active lives while possibly preventing future PFDs. Physiotherapy/Physical Post-Natal Assessment is highly recommended at 4-6 weeks post-delivery but can still be relevant for up to 12 months [26]. A physiotherapy postnatal check-up assesses the PFM, the abdominal muscles and other body parts to help a fully recover from birth. It is necessary to check: PFMs strength, endurance and coordination; abdominal, core and diastasis recti assessment; pelvic assessment: sacroiliac joint, pubic symphysis, modifications of standing posture, pelvic or back pain; full external musculoskeletal screen; any scars or wounds (perineum and/or Caesarean scar).
From this assessment we will prescribe appropriate management strategies, which may include: prescription of specific/individualized PFMT; advice about posture & back care; specific abdominal exercises and recommendations on return to exercise and fitness. According to the “International Survey Questionnaire on Pelvic-Floor Rehabilitation After Childbirth”, countries in Europe are much more likely to recommend and fund pelvic floor rehabilitation programs after birth than USA or Asian countries [14].
Electrical stimulation of the PFM is typically used for patients who experience USI, OAB, FI and POP. It is also used to help PFMs strengthening in women with weak vaginal muscle tone. Pelvic floor electrical stimulation activates pudendal nerve afferents, provides a form of passive exercise with the goal of improving the urethral closure mechanism. In addition, ES can be useful in teaching PFMs contraction to women who cannot identify or contract these muscles voluntarily because of extreme weakness. A non-invasive electrical stimulation with no probe exists that can deliver NMES. The magnetic chair stimulates all of the muscles in the pelvic floor region to rebuild strength and endurance to restore bladder and bowel control. Treatment is painless with power levels able to be adjusted to ensure comfort at all times.
Biofeedback therapy BF can be defined as the use of monitoring equipment to provide individuals with information on the functional activity of their PFMs. Vaginal, anal sensors, surface EMG electrodes, intra-vaginal or anal balloons have been used to make patients more aware of muscle function, and to enhance and motivate patient efforts during training. Recently a magnetic biofeedback device offers a new way of working the pelvic floor, highly effective and non-invasive and allows to strengthen the muscles of the pelvic. This chair scans and records the activities of the pelvic muscles thanks to a special sensor integrated into the seat surface. The muscle contractions are measured in real time by the sensor during training and throughout the sessions to monitor the evolution.
As described above, different techniques are proposed such as PFMT, manual therapy, BF, ES and bladder training. Women's health physiotherapists (WHPTs) can also provide guidance on pain management during pregnancy and postpartum. Physiotherapists/Physical therapists are skilled at evaluating and treating people with MSK problems and can be helpful in reducing symptoms experienced by women during pregnancy and postpartum. Physical therapy, through a combination of manual therapies, specific treatments and therapeutic exercise, can improve health outcomes for new mothers in the postnatal period.
Among the key recommendations is that all women should be given evidence-based information and advice about pelvic floor muscles training and an opportunity to discuss pelvic care with a qualified healthcare professional, like a midwife or a continence nurse. Most continence problems do resolve during the first weeks following birth, but midwives should be checking antenatally. It is really important that this becomes part of normal practice. PTs have the expertise to deliver this training, there is not an interface between PTs and pregnant women unless there is a problem. Midwives are the key profession working with pregnant women, but they have also said they need more training to confidently deliver pelvic health education. Given the prevalence of female UI and its impact on exercise participation, PFMT should be incorporated as a routine part of women’s exercise programs in general. There is a knowledge gap between women’s health and physical therapy, there’s a communication gap between obstetricians and PTs, and there’s a gap between what’s considered “fully recovered” from pregnancy and the demands today’s fit woman places on her body. It is really important to find a midwife or a specialist nurse during pregnancy as well as it’s important to find a physiotherapist/physical therapist with advanced training in assessment and treatment of the pelvic floor.
There are so many terms for the conservative management of PDFs and many health care providers involved in the postpartum including: gynecologists, obstetricians, urologists, coloproctologists, physicaltherapists/physiotherapists, midwives, nurses. In the general population, nobody knows exactly who is specialized in the postpartum management. It will be important to find the right title of these pelvic health professionals and to provide an international network for the childbearing women, in connection with public and media. Pelvic floor complications after childbirth can be painful, embarrassing, and frustrating, but they are treatable.
Women in the UK receive a postnatal check on the state-funded national health system (NHS) which is usually provided six weeks post birth. They may also choose to have a self-funded private postnatal check. The state funded postnatal checks are short with currently no standardized protocol of specific questions and the time allocated doesn’t allow for a complete assessment of the abdominal muscles, diastasis recti or pelvic floor or musculoskeletal dysfunctions. A doctor may specifically ask if a woman is experiencing any incontinence or muscular pain symptoms, or follow up from any birth notes provided from the hospital but the NHAS postnatal checks may be more focused on the baby rather than the mother. If a woman is experiencing pregnancy or postpartum related incontinence, pelvic floor or muscular pain she may not immediately seek help and rather tolerate symptoms believing it is ‘part of having a baby ’or avoid seeking help due to the challenges of caring for a new baby, lack of sleep or support at home, transport issues to attend appointments or a lack of clarity as to which type of service would help her best. From my experience of supporting women be fit and strong during pregnancy and beyond, some women I’ve helped have not been made aware of the importance of seeking help from a Women’s Health Physiotherapist (WHP) or pelvic therapist who have the specific experience, qualifications, assessment protocols and treatment programs for pregnancy and postpartum related pelvic floor disorders, incontinence, muscular pain or diastasis recti. A woman’s body changes fundamentally during pregnancy, labor and birth and along with the need to have emotional well -being to care for her baby, my bias that all women, who give birth vaginally or via caesarian are provided a quality, standardized postnatal assessment. This assessment by trained specialists would check for diastasis recti, pelvic floor dysfunction, back pain or other muscular pain to then offer the best recommendation. If there were no symptoms that needed specific care, at least appropriate recommendations for pelvic health and re-strengthening of the abdominal muscular structure would help women return to optimal strength to lift and carry their baby pain free, return to exercise or sports safely, reduce the risk of injury or pain and have a positive effect on their mental and emotional wellness too.
Having worked in the pelvic health field for over 18 years now I am elated with the increased awareness especially in the younger generations. I started out working with pregnant women and new moms because I felt it was such a missed opportunity to educate women about the pelvic floor, how to prepare for birth, how to recover and to set in place preventive wellness tactics to help them maintain pelvic health for life. As my own life stage evolved into perimenopause and menopause I realized that pelvic health is a topic that needs attention through all life stages. So many women I work with have suffered for years and are now faced with an increase to their suffering with the onset of genitourinary syndrome of menopause. I believe that with the younger generations becoming more informed, they will not accept suffering and will be in a better position to manage the transition to menopause. It is my hope that sometime in my lifetime I will see other countries adopting the practices used in France. Pelvic health should be provided free of charge to women in pregnancy, postpartum and yearly for life. The cost savings to governments would be immense and the quality of life for women would increase significantly. I believe pelvic health care can save marriages, can ease depressive symptoms, and can reduce the risks of heart disease and osteoporosis. Pelvic health is like oral health. We have been conditioned from a young age to brush our teeth twice a day, floss and go see the dentist once or twice a year. We should adopt the same strategies for our pelvic health. Be taught from a young age how to do pelvic floor exercise and protect the pelvic floor muscles as we age, do regular pelvic floor exercise and see a pelvic floor physical therapist once a year.
As illustrated in this interesting and fact-filled article, physiotherapists have a lot to offer in terms of prevention, treatment and quality of life during the perinatality period. In Canada, access to physiotherapy during pregnancy and the post-partum period has increased exponentially over the past three decades. Research in this field is innovative and continuing, the scope of evidence-informed practice has widened substantially, and the availability of continuing education in this focused field of expertise has increased. In addition, expectant and new mothers have become increasingly informed about pelvic health and the benefits of pelvic floor physiotherapy, resulting in increased consultation through direct access. Canadian pelvic health physiotherapists counsel people during pregnancy and delivery, address urinary, sexual and ano-rectal consequences, work on pregnancy-related musculoskeletal problems as well as consequences of Cesarean section, and help with breastfeeding-related issues. With the help of Canadian guidelines, they also assist with physical activity during pregnancy, post-partum recovery and return to optimum physical activity. Canadian universities include basic information about pelvic floor disorders in their core curriculum. Government bodies have been mandated to explore the advantages of increased accessibility for publicly funded physiotherapy for women during the perinatality period (the French example is cited regularly!). And, pelvic floor physiotherapy services are becoming increasingly available in the public sector, including post-partum treatments in adult institutions and services for new mothers in paediatric facilities.
France is decades ahead of the United States in taking care of the post-partum woman. I’ve worked in the pelvic health realm of physical therapy since 1999. In the early 2000’s, we saw some patients referred to PT by their obstetricians. These women had significant birth injuries - a 4th degree perineal tear or severe symphysis pubis dysfunction. The “average” new mom was not referred to us. Most women did not know pelvic health physical therapy existed. Physicians and the general population lacked education in the care we could provide. A turning point in consults to pelvic health PT for this population came in 2018 when the American College of Obstetricians and Gynecologists updated an opinion paper redefining post-partum care. The “fourth trimester” started trending in pregnancy/new mom groups through social media and the concept took hold. Midwives and OB/GYNs, who were now seeing new moms at 3 weeks instead of the typical 6-week mark, began to consult physical therapy early in the birth recovery process. Women started to contact our clinics on their own to schedule a PT evaluation via direct access/self-referral. Our practice saw a significant increase in volume of post-partum women. These were no longer only those with traumatic birth injuries or elite athletes, but finally a variety of new moms with common concerns about their body and function after giving birth. Our physical therapy assessment addresses all concerns raised by the patient. We provide education and treatment in several areas including: diastasis rectus abdominis, pelvic muscle exercise, posture, back/pelvic pain, pelvic organ prolapse, scar tissue mobilization, sexual health, pain neuroscience, and return to exercise/running. All bowel, bladder, and pelvic muscle coordination deficits are treated. Many insurances in the US will cover PT post-partum when a covered diagnosis such as muscle weakness or pelvic girdle pain is applied. The duration and frequency of pelvic health PT varies based on the individualized plan of care established. Some women present themselves to us with few issues and only need one to two PT visits. Others have significant incontinence and/or pain requiring several sessions. Treatment may include sEMG biofeedback. Real-time ultrasound is not yet readily available in PT clinics in the US. I believe as we educate and treat new mothers in the 4th trimester, we will see fewer women with serious incontinence and prolapse issues in the years ahead.
I appreciate all the efforts of Alain Bourcier to bring light to the worldwide need of prenatal/postpartum care and the need to bolster the building of relationships between the Ob-Gyn, Nursing, Midwife, Physiotherapy and other peri-natal healthcare communities. In the US, there is still a disconnect between physiotherapists and the Ob-Gyn/Midwife communities with post-partum referrals to PT increasingly stemming from new moms seeking out and requesting this care based on information consumed on their social media feeds. Although, the increased awareness that there are healthcare providers that can assist with pregnancy and post-partum dysfunctions, the misinformation prevalent in social media is alive and well for this easily targeted population. Education for the Ob-Gyn/Midwife/nursing community about care team options for their pregnant/post-partum clients is essential to optimize the care their patients are given. In the US in 2018, our American College of Obstetrics and Gynecology (ACOG) officially recognized the need to update their postpartum care allowing for a more wide-ranged assessment to meet the needs of the new mom with the 6-week post-partum check modified to include: mood and emotional well-being, infant care and feeding, sexuality contraception and birth spacing, sleep and fatigue, PHYSICAL RECOVERY FROM BIRTH, chronic disease management and health maintenance. Per ACOG: “The re-design emphasis for the post-partum visit has been termed 4th trimester care” The goal is to create a team approach with providers from various disciplines to meet the new mom’s needs. Cross discipline education would be useful for Ob-Gyns, Nurses and Midwives to more fully understand the capabilities of physiotherapy intervention for addressing musculoskeletal pain, pelvic pain, dyspareunia, bladder/bowel/sexual dysfunction as stated in this article. Some interdisciplinary steps forward in the US have included the creation of Pelvic Guru (https://pelvicguru.com/) which has a free multidisciplinary international directory of providers to address Pelvic Health. Pelvic Guru also provides educational resources for providers to learn about each other’s professional disciplines. Another excellent giant leap forward in the COORDINATION of pre-natal/postpartum care (over 300 specialty options) is being provided by MAVEN digital health care for women. MAVEN provides care advocates that coordinate care for prenatal/postpartum women and allows for excellent interdisciplinary communication between many disciplines including Physiotherapy. The Maven Care Team can even coordinate in person care with various providers as needed. I am thankful for all of research that has been done to show where the deficits in continuum of care are present as this has paved the way for the gaps to be filled.
The probability of incidence of having PFDs is very high in the region due to many contributing factors like high parity, obesity, cultural background, and lack of awareness. There is no data regarding the prevalence of pelvic floor disorders in postpartum in the UAE. Postpartum care is usually compromised due to a lack of postnatal referrals for physical therapy unless the development of certain symptoms. However, a multidisciplinary approach and timely therapy have reflected promising outcomes in the young population. Therapy is solely based on the evaluation of pelvic floor muscles, muscle coordination, and joints by a specialist physiotherapist. Based on the above observations, patients are educated about their musculature and posture correction and are trained with biofeedback-assisted pelvic floor therapy. Individual therapy plans are formulated and carried over for a minimum duration of 10 to 12 weeks. The progress is constantly monitored and the therapy plan is modified when indicated. Pelvic floor muscle (PFM) re-education is an effective, low-risk intervention that reduces pelvic floor disorders significantly, especially in postpartum patients. Post-partum examination and assessment before discharge from the hospital should be mandatory to minimize the therapy-related burden associated with delayed reporting by the related population. Trained Pelvic Floor therapist can play vital role in carrying out the result oriented therapy program for individuals with PFDs.
The changes that occur with pregnancy and postpartum lead to imbalances throughout the body and one of the most affected is the pelvic floor, which plays a fundamental role in evacuation processes, continence, and sexual function. However, their lack of knowledge is really important, which is why this type of article gives us the opening to know the changes that occur throughout this stage and how future dysfunctions can be prevented. In many postpartum women, their desire to return to the ideal body image begins to perform high-impact exercises to obtain a flat belly, doing sit-ups, cross-fit and other hyper-pressive activities that increase abdominal pressure. In other cases, many women view tutorials from various virtual platforms, in which they "teach" to indiscriminately strengthen their pelvic floor, without having to undergo a training, personalized muscle and even more, without knowing if they carried out an adequate command and efficient recruitment. All this leads us to raise awareness of the important work that pelvic floor physiotherapy has a preventive role, being the basis for maintaining optimal pelvic health and thereby reducing associated health costs in the future. Under the same scheme, these health systems still consider routine episiotomy, although many health professionals are increasingly considering it as elective. In some cases, after the vaginal delivery, the patients are discharged, without any subsequent follow-up and shortly after, when they want to return to their sexual activity, they complain of pain without knowing why. In general, all these consequences can be efficiently addressed with an adequate postpartum rehabilitation program, which will range from the assessment of the pelvic floor to postural alignment, because, during the lactation stage and the carrying of the baby, they will see many modifications reflected both at the level of the shoulder girdle and pelvic girdle. Finally, pelvic floor physiotherapy is a specialty that little by little has gained worldwide reach and it is of vital importance for the prevention and treatment of symptoms or dysfunctions associated with pregnancy and postpartum.
Pregnancy, vaginal delivery and c-section generate physical changes that often determine disfunctions like urinary incontinence, pelvic organ prolapse, pelvic girdle pain, low back pain, to mention some. This issues impact in a strong way in women health and quality of life and may associate with physical activity and labor desertion. Even the American College of Obstetricians and Gynecologist in its committee opinión number 736 exposed the need of redefining the postpartum visit. Unfortunately, there is a lack of information about this important topics in the training programme of health care professionals. In opposition to that, women started to talk about the difficulties they expierenced during this trascendent moment of their lives and motive other women to ask for information and resources to have and optimal recovery. Pelvic Physiotherapy have a lot to offer to respond to those needs. Pelvic Floor Rehabilitation include life style interventions, ergonomy advice, manual theraphy, especific ecxercises end theraphies like bioffedback. In other words effective, evidence based, simple, economy and almost secondary effects free resources. But much work remains to be done. In Argentina there are a few Public Hospitals that offer Pelvic Physiotheraphy and, although the practic is agreed by prepaid medicine, the payment is bad and most of the centers works privately. Nevertheless, there is a growing interest and we hope it changes soon. With the Sociedad Kinesica Argentina de Pelviperineologia, which I have the honor to preside, we are working hard to spread the importance of Pelviperineal Physiotherapy in women health and lives.
Although the taboo about pelvic floor dysfunction and body changes postpartum seems to decrease in networks of women’s health professionals, we might not underestimate the lack of knowledge the lay public still has about these topics. Previous studies showed that Belgian women of all ages acknowledge that they don’t know enough about the pelvic floor. They also revealed that women are eager to receive more information, but on the other hand, that women often don’t search for information proactively. These finding have inspired us to launch an online information platform and social media campaign in Belgium, with clear goals: breaking taboo, raising awareness and sharing knowledge to the lay public. Women need to learn what is normal and what is not. Women have the right to be informed what could happen in the postpartum and how body changes and pelvic floor problems might affect their quality of life. We are strongly convinced that informing women better, will increase their intrinsic motivation to search for help and to stay adherent to therapy once they started. But also to increase the effectiveness of prevention. Physiotherapy in Belgium for perinatal care and pelvic floor reeducation is very well organized. We have many well-educated physiotherapist, that are able to support, guide and coach women during these important events in life. But often women don’t find their way to the physiotherapist. Evidence clearly shows that early promotion of pelvic floor exercises is possible. Although the effects on the longer term might be contradictory, we are convinced that during pregnancy and in the postpartum we have a window of opportunity to reach out to women. To raise awareness and convince them that prevention is better then cure. But also that if pelvic floor problems later in life would occur, good personalized care is key to improve their quality of life. In conclusion, in the peripartum period empowering women in selfcare and emphasizing on good education might be key to improve women’s health care also later in their lifecycle. Physiotherapist specialized in pelvic floor reeducation are the most suitable women’s health care professionals to invest in both general education, prevention and personalized specialized advices if they also invest enough effort in communication with the other colleagues from the multidisciplinary team and if they learn how to reach out to women with empowering information. To support all women’s health professionals with those goals, we developed www.thepelvicfloor.be in Belgium, a digital information platform with online self-check and online self-management exercise program and many more ambitions for the future.
Website: www.Jointdynamicsevolve.com
In Hong Kong, there is still a big gap in post partum care. Post natal checks (when available) focus mostly on the medical considerations and there is little in depth assessment of the pelvic floor, abdominal wall, scar or general posture. Pelvic Health Physiotherapy remains somewhat primitive and awareness and access is primarily in the private Healthcare setting. The majority of referrals are clients who self refer seeking more guidance and support with their post partum journey. A multidisciplinary approach and access to all should be the goal worldwide!
I am particularly grateful for the assistance given by Angie Rantell (King's College Hospital NHS Foundation Trust, UK), Kathe Wallace (Physical Therapy Resources, USA) and Gail Zitterkopf (Memorial Hermann Healthcare System, USA).
I would like to thank the following people who participated to the “International Survey on Pelvic Floor Rehabilitation after Childbirth » which was the cornerstone of this article.
Kaven Baessler (DE), Rebeka Das (IN), Gráinne Donnelly (UK), Maria Elliott (UK), Jenny Fielding (HK), Tanya Gutierrez (CA), Sarah Haag (USA), Mirian Kracochansky (BR), Diane Lee (CA), Maale Madjob (MA), Ingrid Nygard (USA), Ferit Saracoglu (TR), Jane Simpson (UK), Anna Padoa ( IL), Małgorzata Starzec-Proserpio (PL) Carla Mendes Torrieri (BR).
Copyright: © 2024 Lino Di Rienzo Businco., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.