Paul Hartel1* and Aoife Ryan1,2
1Department of Pathology, University Hospital Sligo, Ireland
2Atlantic Technological University, Galway, Ireland
*Corresponding Author: Paul Hartel, Professor, Department of Pathology, University Hospital Sligo, Ireland.
Received: September 03, 2024; Published: September 18, 2024
Citation: Paul Hartel and Aoife Ryan. “Clinical Impact of Hysteroscopically Normal Endometrium Samples Submitted to Pathology". Acta Scientific Women's Health 6.10 (2024):28-30.
In light of recent best practice recommendations and strategic laboratory reform efforts, we evaluated the clinical impact of endometrial samples from hysteroscopically and transvaginal sonographically normal endometrium in routine ambulatory gynaecologic clinics. We found that, while it may be necessary to depart from best practice recommendations in the interests of specific patients and circumstances, endometrial sampling with normal hysteroscopy and transvaginal endometrial thickness < or = 4mm has no clinical impact and is essentially of no clinical value. Avoiding submission of such samples to pathology laboratories will allow for the more expedient processing and reporting of more clinically meaningful tissue samples.
Keywords: Normal Endometrium; Hysteroscopy; Transvaginal Sonography; Laboratory Reform; Best Practice Recommendations
Best practice recommendations published by the Royal College of Pathologists [1] should assist pathologists in providing a high standard of care for patients. BPRs are based on the best available evidence at the time and systematically developed statements intended to assist the decisions and approach of practitioners and patients about appropriate actions for specific clinical circumstances. A section of the most recent BPRs suggests that routine endometrial sampling may not be necessary in women with dysfunctional uterine bleeding and normal transvaginal ultrasound showing thin endometrium without focal lesions, and normal hysteroscopy. Considering ever-increasing histology laboratory workloads and lack of laboratory scientific staff, a reduction in tissue samples that ultimately have no clinical impact would be optimal. This would allow for more meaningful samples, such as those from new and more clinically urgent ambulatory gynaecology clinics. Endometrial samples submitted to Sligo University Hospital histopathology laboratory in the year 2023 were identified by CoPath pathology archive search. Those with normal hysteroscopy and transvaginal ultrasound findings indicated on the pathology requisition at the time of sampling were selected for review. Clinical variables including patient demographics, symptomatology, hysteroscopy and transvaginal scanning results, medical record review and histology findings were anonymously recorded. Patients (n = 75) ranged in age from 29 to 73 years (m = 51) and had symptoms of abnormal or post-menopausal bleeding. All had normal hysteroscopy and transvaginal ultrasound findings. Endometrial sampling histology showed benign predominantly proliferative or atrophic endometrium without atypia, malignancy or chronic endometritis. Four samples were non-diagnostic. In none of the cases did histology add information beyond that determined at hysteroscopy or transvaginal scan or affected or altered clinical management.
Endometrial samples submitted to Sligo University Hospital histopathology laboratory in the year 2023 were identified by CoPath pathology archive search. Those with normal hysteroscopy and transvaginal ultrasound findings indicated on the pathology requisition at the time of sampling were flagged for audit. Age, symptoms, hysteroscopy and transvaginal scan findings and histology were anonymously tabulated. Medical record was reviewed to determine clinical impact of histology findings above and beyond hysteroscopic and transvaginal sonography findings. If histology added information to clinical findings in a way that affected or altered clinical management, this was noted. Hysteroscopies and transvaginal ultrasounds were performed by senior specialist consultant gynaecologists and histology slides reviewed by senior consultant specialist histopathologists.
Patients (n = 75) ranged in age from 29 to 73 years (m = 51) and had symptoms of post-menopausal bleeding (26), menorrhagia (21), metrorrhagia (12) and discharge (1) with the remaining having no symptoms documented on histology requisition. All had normal hysteroscopy (Figure 1) and transvaginal ultrasound findings. Endometrial sampling histology (Figure 2) showed benign atrophic (24), proliferative (28), secretory (7) or some combination of these (12) without atypia, malignancy or chronic endometritis. Four samples were non-diagnostic. In none of the cases did histology add information beyond that determined at hysteroscopy or transvaginal scan or affected or altered clinical management.
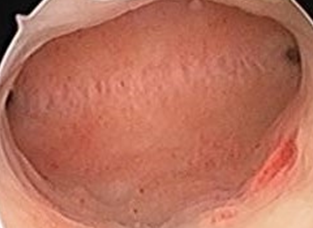
Figure 1: Hysteroscopically normal uterus.
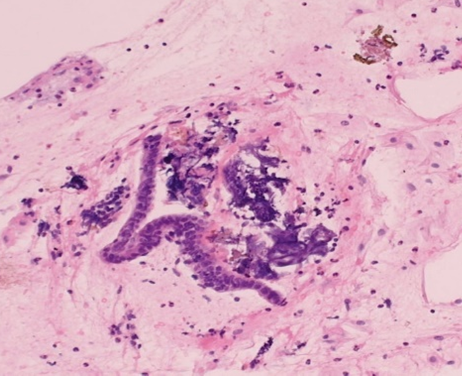
Figure 2: Histology, scant benign endometrium, H & E stain, medium power.
Currently, Pipelle endometrial sampling is widely used to diagnose endometrial cancer in women with abnormal uterine bleeding and postmenopausal bleeding [2]. The method became very useful due to easiness and simplicity of the procedure, availability of a device, as well as high sensitivity in detecting endometrial cancer [3,4]. Many studies compared the validity and accuracy of Pipelle biopsy with dilation and curettage in the detection of various endometrial pathologies. Published results state that Pipelle biopsy and uterine curettage are almost equally reliable in the evaluation of endometrial pathologies [5-7]. For initial clinical visualisation, transvaginal sonography is most important for diagnosis of uterine anatomical lesions, as hysteroscopy is most specific and sensitive for diagnosis of polyp but less specific for endometrial hyperplasia [8]. In general, both methods have been shown highly sensitive, but hysteroscopy was more specific than transvaginal sonography [9]. A recent report concluded that transvaginal ultrasound remains the first line diagnostic procedure in postmenopausal women without abnormal uterine bleeding because it has high sensitivity for detecting endometrial cancer and other endometrial disease, but that outpatient hysteroscopy with biopsy is mandatory in all postmenopausal women with abnormal uterine bleeding [10].
The utility of endometrial biopsy is undebated in instances of focal uterine abnormalities or suspicious lesions and cases of thickened endometrium in patients with abnormal uterine bleeding, typically > 4mm, on transvaginal sonography [11,12]. However, in postmenopausal patients with bleeding, biopsy is not indicted when endometrial thickness is <or = 4 mm, and the significance of thickened endometrium in nonbleeding postmenopausal women has not been validated and also need not require tissue sampling [13]. Royal College of Pathologists, UK, best practice recommendations state that endometrial sampling should not routinely be performed in women with abnormal bleeding under the age of 40 years. Some gynaecologists do not biopsy the endometrium even in women over this age if the transvaginal ultrasound shows a thin endometrium with no focal lesions, and a normal hysteroscopy [1]. It is rare for a significant abnormality to be found on histopathology if the gross examination is negative [14]. The results reported here support this contention.
While it may be necessary to depart from best practice recommendations in the interests of specific patients and circumstances, this study supports that endometrial sampling with normal hysteroscopy and transvaginal endometrial thickness < or = 4mm has no clinical impact and is essentially of no clinical value. The clinical risk of departing from the best practice recommendations should be assessed and documented. Considering ever-increasing histology laboratory workloads and lack of laboratory scientific staff, a reduction in tissue samples that ultimately have no clinical impact would be optimal. This would allow for more expedient processing and reporting of more clinically meaningful samples.
We would like to thank Linda Bredin, Laboratory Medical Scientist, for her assistance in data retrieval.
None.
Copyright: © 2024 Paul Hartel and Aoife Ryan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.