Rahul Manchanda1, Anurag Mahajan2 and Neha Sinha3*
1Head of Department, Gynaecology Endoscopy Department, PSRI, New Delhi, India
2Senior Consultant, Medicine Department, PSRI, New Delhi, India
3Senior Registrar, Gynaecology Endoscopy Department, PSRI, New Delhi, India
*Corresponding Author: Neha Sinha, Senior Registrar, Gynaecology Endoscopy Department, PSRI, New Delhi, India.
Received: August 14, 2024; Published: August 27, 2024
Citation: Neha Sinha., et al. “Post Ectopic Transfusion Related Lung Injury - A Physician’s Nightmare: A Case Report and Review of Literature". Acta Scientific Paediatrics 6.9 (2024):24-27.
Analysis of one of the fatal reactions of blood transfusions (TRALI)- transfusion-related acute lung injury- diagnostic criteria, pathophysiology, and patient care. TRALI is an increasing life-threatening complication of blood transfusion in today’s medical field. Review of literature was done and a case review and discussion were used to analyze TRALI. By examining databases including PubMed, Cochrane database, Embase, Science direct, Google Scholar, and others, a review of several papers. The keywords used to search the articles were TRALI, blood transfusion, post ectopic TRALI etc. We searched a number of articles and studies, up until June 2024. It is based on relationship between the onset of hypoxemia and transfusion. It can range from mild symptoms to life threatening event. TRALI is a significant complication related to transfusion that is currently being better understood in terms of its frequency, pathophysiology, risk factors, potential prevention, and emergency therapies. A comprehensive clinical evaluation that takes into account the patient's signs and symptoms, fluid balance, heart health, brain natriuretic peptide levels, and leucocyte counts are just a few of the factors used to diagnose and treat it.
Keywords: TRALI; Ectopic Pregnancy; SpO2; Pulmonary Oedema; Acute Lung Injury
TRALI also known as transfusion related acute lung injury it is a rare complications of blood transfusion which can be life threatening [1]. It should be included as the differential diagnosis of acute lung injury in obstetrics and gynecological patient who has been give massive blood transfusion [2]. TRALI results in ARDS and non-cardiogenic lung oedema developing during 6 to 72 hours of transfusion [3].
The incidence is estimated to be 1 in 5000 blood products [3]. It manifests as dyspnoea and tachypnoea and sudden onset of Respiratory difficulty in few hours after transfusion. Chest X-ray shows lung infiltrates, decreased SpO2. A few cases of TRALI may require ventilator support. Brain Natriuretic Peptide and leucocyte count are few of the parameters to diagnose it [4].
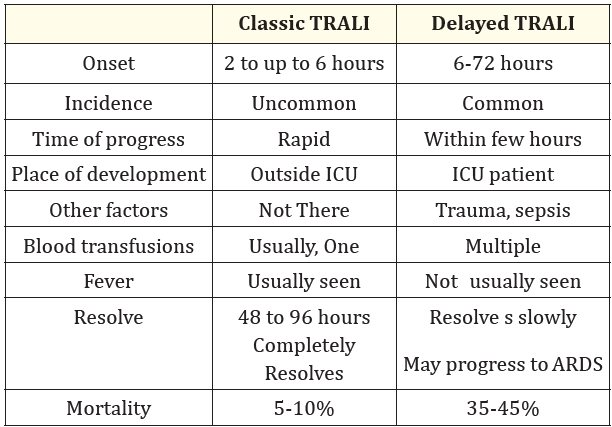
Table 1: Difference between Classic and Delayed TRALI.
Various articles were assessed for the non-systemic review on the post-ectopic TRALI, including methods and clinical applications of the TRALI in context with the fatal reaction of blood transfusion to acute lung injury. The articles were reviewed by searching various databases, including PubMed, Google Scholar, Embase, Web of Science, Science Direct, Cochrane database etc. the articles were filtered based on full text availability, year of publication and relevance of the topic until June 2024. The studies with description of TRALI, including their association with blood transfusion were selected for the review. The keywords used were TRALI, blood transfusion, fatal reaction of blood transfusion.
Mrs X aged 40 yrs living in a nearby area was admitted in emergency with presenting complaints of intense pain in abdomen since morning and bleeding per vaginum, there was history of giddiness since morning.
She was nullipara married for 2 years. Her menses were regular. Patient looked pale and dehydrated. Her ultrasound scan was suggestive of ruptured ectopic (left sided) with hemoperitoneum. On general examination pulse was 122/min, blood pressure was -80/60mmhg. SpO2 -98% on room air, on per abdominal examination - abdomen was tense and tenderness present over left iliac fossa and suprapubic region. Urinary pregnancy test was positive. ABG was done metabolic acidosis was reported, resuscitation was started with crystalloids solution. Patient was catheterized. Vasopressors were started.
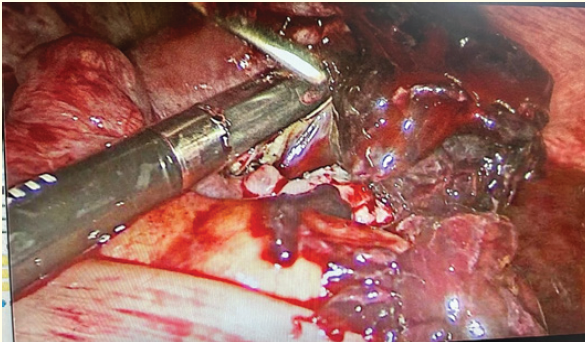
Figure 1: Ruptured ectopic (left side).
Investigations; - Hemoglobin 3.2 g%, blood group -B positive, Prothrombin time 16.2sec, INR- 1.47, viral markers and liver and kidney function tests were normal. Patient was catheterized and immediately taken for emergency laparoscopic Salpingectomy (left sided). Blood transfusion was started intraoperatively. Clots and blood of approximately 2.5 litres were removed. Patient was stable immediately after surgery, 5 units of blood were transfused. After shifting to ICU patient had a fall in SpO2 to 80% and also fall in blood pressure. Vasopressor’s dose was increased. On the next day patient was tachypnoeic, chest X-ray showed bilateral infiltrates and on chest auscultation there was bilateral crepitations present.
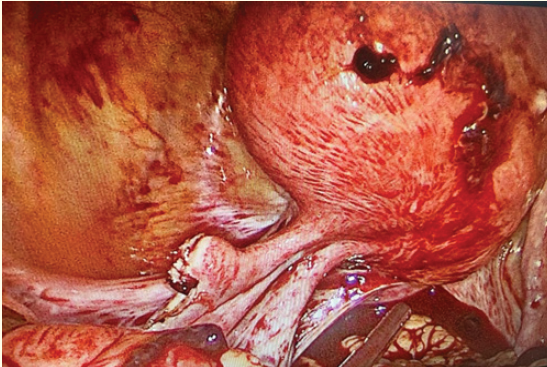
Figure 2: Post laparoscopic (left side) salpingectomy.
ECHO was suggestive of stress cardiomyopathy; blood culture was negative and Minibal (lung aspirates) showed no organism hence the diagnosis of TRALI was suspected. Following the progress of the patient she was on noninvasive ventilator following mechanical ventilation and intubation, central line insertion was done. Patient was on injectable antibiotics and steroids and lasix. Chest physiotherapy was started. Patient was extubated eventually and ventilator weaning was done gradually in ICU and it was uneventful. Patient was discharged on the 10th day.

Figure 3: Chest X-Ray showing bilateral lung infiltrates of the above patient.
In case of TRALI (transfusion related acute lung injury), there is crepitations and respiratory distress issues. TRALI is an acute non cardiogenic pulmonary oedema, which is typically associated with blood transfusion. In such cases lung injury is transient and returns to pretransfusion state within 48-96 hrs. In few cases, it has been recommended to provide noninvasive respiratory support along with positive airway pressure (BiPAP) or continuous positive airway pressure (CPAP), however, in severe cases endotracheal intubation is better option, when coupled with invasive mechanical ventilation [5]. In above presentation, the patient was over 40 years of age with ruptured ectopic pregnancy, before transfusion there was no respiratory distress, post-surgery and blood transfusion patient developed hypotension and respiratory difficulty. Based on clinical findings and no indication of origin of pulmonary oedema being cardiogenic, we decided to categorize and treat the condition as TRALI. Hemodynamic and ventilatory needs were the foundation of supportive treatment.
Although there is a lot of care, patients who survive TRALI typically recover gradually. A death rate of more than 12% is recorded following diagnosis [3]. After hepatitis and ABO blood incompatibility, transfusion-related deaths are most frequently caused by TRALI [6]. It has been estimated that the incidence rate of TRALI is between 0.01 and 0.08 percent per transfused unit containing plasma, with a death rate ranging from 5 to 14 percent [6,7]. TRALI is a clinical diagnosis because there are no identifying biomarkers (Table 2). The absence of a widely accepted terminology for TRALI has delayed research on the its epidemiology and underdiagnosis as well [8]. TRALI is not common but fatal side effect of blood transfusion that is getting more and more attention. Adding on to radiographic indications of pulmonary oedema and adequate heart activity, it shows pulmonary insufficiency [9]. The pathophysiology is linked to two primary theories: either higher pulmonary capillary permeability because of anti-leukocyte antibodies in the donor blood, or neutrophil activation brought on by physiologically active substances like lipids and cytokines [10].
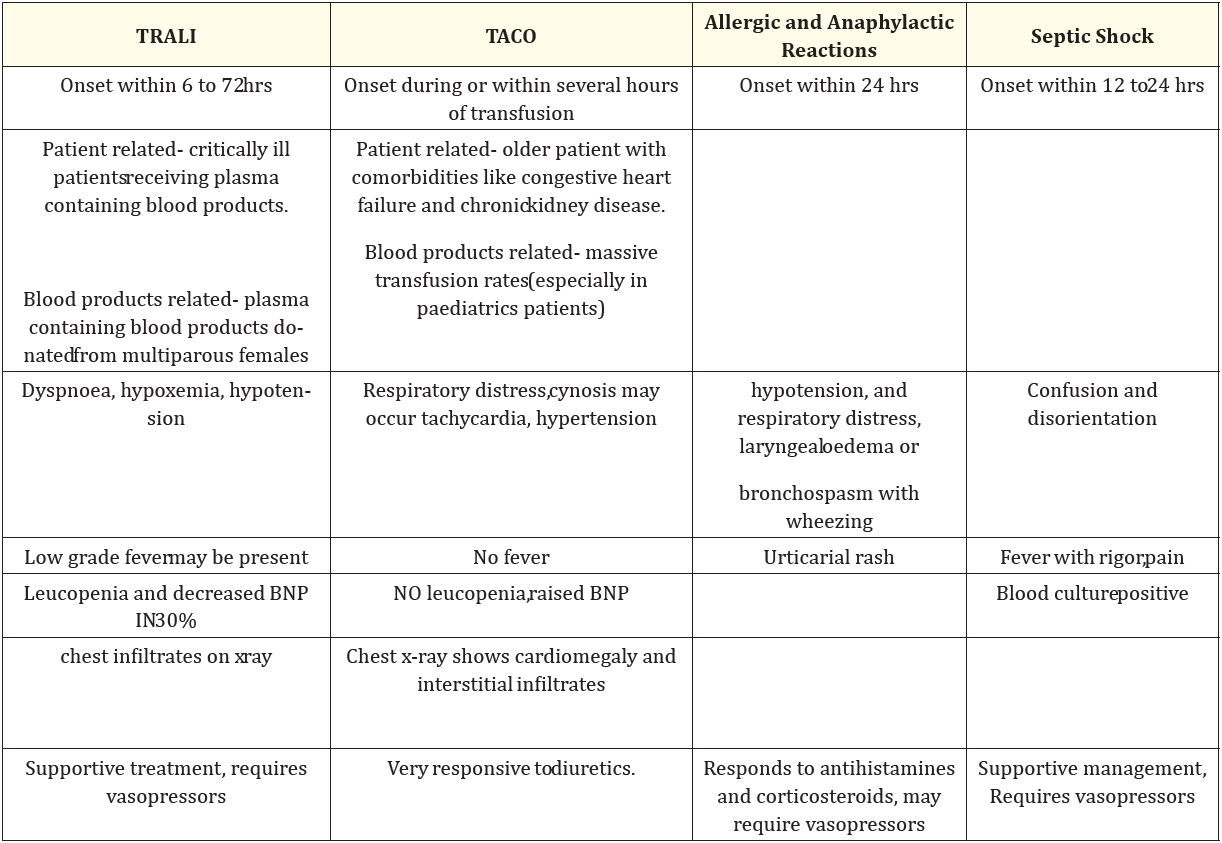
Table 2: Differential diagnosis of TRALI.
Due to Anti-leukocyte antibodies, the recipient leukocytes to become activated. This causes the leukocytes to get sequestered in the lung, where they degranulate and increase capillary permeability. The second process involves the activation of the pulmonary endothelium as a result of underlying medical diseases such as sepsis, inflammation, etc. This leads to the sequestration of neutrophils inside the lung, or "primed" neutrophils, which then trigger pulmonary capillary leaks when donor antibodies activate them [11]. In patients without a history of ALI (acute lung injury) prior to transfusion, the National Heart, Lung, and Blood Institute defined Acute Lung Injury that occurs within first 6 hours after transfusion [8]. TRALI should be performed in all cases of respiratory disorders with hypoxemia and a PaO2/FiO2 ratio of less than 300mmHg [11]. We have observed signs, such as tachycardia, leucopenia, fever, and hypotension in the present study. TRALI has included plasma comprising blood components such as complete blood, platelet concentrates, new solidified plasma, pressed reddish cells, granulocytes, cryoprecipitate, and intravenous immunoglobulin [10]. TRALI should be on the differential diagnosis of acute lung damage particularly after blood transfusion [12]. Decrease in hemoglobin isn't a reliable finding but neutropenia has been seen [13]. TRALI can be diagnosed on the clinical findings and investigations (CBC, Chest Xray, LFT, KFT, ABG etc.) [14]. Hospital management consists mostly of supportive care, diuretics, and respiratory assistance using either passive or direct ventilation. Mechanical ventilation can be utilized in low tidal volume and low blood pressure to prevent barotrauma [15].
TRALI is difficult to diagnose, and treatment takes time. The distinction between hydrostatic and permeability pulmonary oedema following blood transfusion is difficult to explain because the two symptoms can coexist. Despite numerous ideas, it is preventable with proper blood transfusion procedures. The outcome is determined by age, the necessity for artificial breathing, the number of organs implicated, and the responsiveness to the treatment administered. There is no specific treatment for TRALI. If the transfusion is still ongoing, it should be stopped immediately, and oxygen and supportive measures should be implemented. This syndrome is characterized by early onset of symptoms and progressive impairment of respiratory functions; despite good supportive care, death remains a major issue. It's crucial to have a multidisciplinary approach for predicting, preventing, treating and following up transfusion related acute lung injury like reactions.
Copyright: © 2024 Neha Sinha., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.