Adinarayana Andy1*, Divya Andy2 and Aman Suresh Tharayil3
1Pharmacy Manager Weatherwax Family Pharmacies Inc Spring Arbor, Michigan, USA
2Independent Research Consultant, Michigan, USA
3Assistant Professor, Department of Pharmacy Practice, Sandip Institute of Pharmaceutical Sciences, Nashik, Maharashtra, India
*Corresponding Author: Adinarayana Andy, Pharmacy Manager Weatherwax Family Pharmacies Inc Spring Arbor, Michigan, USA.
Received: September 24, 2024; Published: September 29, 2024
Citation: Adinarayana Andy., et al. “Pharmacological Interventions and Emerging Therapies in the Management of Obesity". Acta Scientific Pharmaceutical Sciences 8.10 (2024):35-41.
Obesity is a complex, chronic condition characterized by an excessive accumulation of body fat, defined by a Body Mass Index (BMI) of 30 or higher. It is a growing global health issue linked to numerous health complications, including type 2 diabetes, cardiovascular diseases, and certain cancers. The prevalence of obesity has escalated significantly in recent decades, affecting individuals of all ages and backgrounds. Its multifactorial causes range from genetic and environmental factors to behavioral and psychological influences. While lifestyle changes are central to obesity management, pharmacological interventions are increasingly being explored to enhance weight loss efforts. This paper explores the epidemiology, pathogenesis, and current pharmacological approaches to obesity management, including emerging treatments that offer new hope in the fight against this global epidemic.
Keywords: BMI; Obesity; Weight Loss
Obesity is a complex, multifactorial chronic disease that has become a major global health concern [1]. Characterized by an excessive accumulation of body fat, obesity is defined by a Body Mass Index (BMI) of 30 or higher (Table 1) [2]. This condition is not merely a cosmetic issue but a serious medical concern associated with a wide range of health complications, including type 2 diabetes, cardiovascular diseases, certain types of cancer, and increased mortality [3].
The prevalence of obesity has risen dramatically over the past few decades, affecting individuals across all age groups and socioeconomic backgrounds. According to the World Health Organization (WHO), more than 1.9 billion adults worldwide were overweight in 2016, with over 650 million classified as obese [4]. This trend shows no signs of abating, with obesity rates continuing to climb in both developed and developing nations.
The causes of obesity are multifactorial, involving an interplay of genetic, environmental, psychological, and behavioral factors. Sedentary lifestyles, poor dietary habits, and the widespread availability of high-calorie, nutrient-poor foods have contributed significantly to the obesity epidemic [5]. Additionally, factors such as genetics, hormonal imbalances, and certain medications can predispose individuals to weight gain.
Obesity poses a substantial burden on healthcare systems, with associated medical costs and productivity losses running into billions of dollars annually [6]. Beyond its physical health implications, obesity also has a profound impact on mental health, often leading to stigmatization, low self-esteem, and depression.
Given the complexity of obesity and its far-reaching consequences, effective management requires a multifaceted approach. This typically includes lifestyle interventions, behavioral therapy, and in many cases, pharmacotherapy or bariatric surgery. However, the challenges of sustained weight loss and the prevention of weight regain make obesity a difficult condition to manage long-term.
In response to the growing obesity crisis, there has been significant interest in the development of pharmacological treatments that can aid in weight loss. These medications offer an additional tool for individuals who struggle to achieve and maintain weight loss through lifestyle modifications alone [7]. As research continues to advance, new weight loss drugs are emerging, providing hope for more effective and sustainable obesity management.
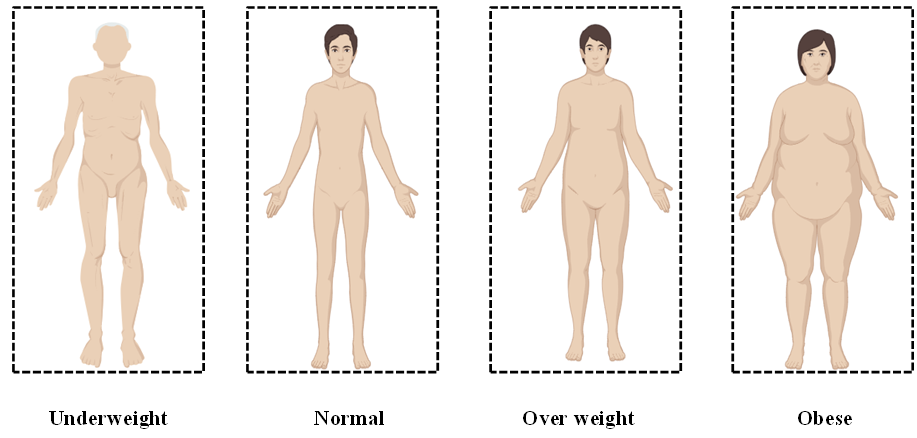
Figure 1: Classification of BMI.
Obesity is a significant public health concern with a rising global prevalence. According to the World Health Organization (WHO), more than 1.9 billion adults were overweight in 2016, with over 650 million of them classified as obese [4]. The prevalence of obesity has nearly tripled since 1975. In the United States, the Centers for Disease Control and Prevention (CDC) reports that 42.4% of adults were obese in 2017-2018, up from 30.5% in 1999-2000 [8]. Obesity rates are also increasing among children and adolescents, with 19.3% of U.S. youth affected in 2017-2018 [9]. This condition is associated with numerous health risks, including cardiovascular diseases, type 2 diabetes, and certain cancers, leading to increased mortality and a substantial economic burden on healthcare systems.
The pathogenesis of obesity is a complex process involving multiple factors, including genetic, environmental, and physiological influences.
Obesity tends to run in families, suggesting a strong genetic component. Genes can influence the storage and distribution of body fat, the rate of metabolism, and appetite regulation [10].
Rare genetic conditions, such as mutations in the leptin or leptin receptor gene, can cause severe obesity [11].
Most cases of obesity are polygenic, where multiple genes contribute small effects that collectively increase susceptibility to obesity [12].
High-calorie diets, particularly those rich in fats and sugars, contribute to energy imbalance and weight gain.
Sedentary lifestyles, influenced by modern conveniences, reduce energy expenditure and promote weight gain.
Lower socioeconomic status is often associated with limited access to healthy foods and opportunities for physical activity.
The body’s energy balance is regulated by a complex interaction between the central nervous system, peripheral organs, and hormonal signals. Dysregulation in these systems can lead to an imbalance between energy intake and expenditure [13].
Hormones like insulin, ghrelin, leptin, and cortisol play significant roles in hunger, satiety, and fat storage. For example, leptin resistance is commonly observed in obese individuals, where the body does not respond appropriately to the satiety signals from leptin [14].
Adipose tissue is not just a storage depot for fat but also an active endocrine organ that secretes various adipokines, which influence inflammation, insulin sensitivity, and energy metabolism. In obesity, adipose tissue can become dysfunctional, contributing to systemic inflammation and metabolic disturbances.
The composition of gut microbiota is different in obese individuals compared to lean ones. The gut microbiome can influence the efficiency of energy extraction from food, inflammatory processes, and the production of short-chain fatty acids, which may affect appetite and fat storage [15].
Stress and negative emotions can trigger overeating or preference for high-calorie comfort foods, contributing to obesity.
Lack of sleep is associated with hormonal changes that increase appetite and cravings for unhealthy foods, leading to weight gain.
Epigenetic modifications, such as DNA methylation and histone modification, can alter gene expression in ways that predispose an individual to obesity. These changes can be influenced by diet, physical activity, and other environmental factors [15].
The hypothalamus plays a central role in regulating hunger and energy balance. Dysregulation in the hypothalamic circuits, often due to genetic or environmental factors, can lead to increased food intake and reduced energy expenditure, contributing to obesity [16].
Weight loss occurs through several interconnected mechanisms, primarily involving a caloric deficit, where the body expends more energy than it consumes. This deficit forces the body to utilize stored fat as an energy source, leading to fat loss. Additionally, weight loss is influenced by hormonal changes that regulate appetite and metabolism. For instance, lower levels of insulin, a hormone that promotes fat storage, can enhance fat breakdown. Increased physical activity also plays a significant role by boosting metabolic rate and muscle mass, which in turn raises the body's energy expenditure. Furthermore, changes in diet, such as reduced carbohydrate intake, can lead to decreased insulin levels and increased fat oxidation. These combined factors contribute to overall weight loss, promoting a healthier body composition and reducing the risk of obesity-related diseases [17].
For many chronic conditions, including obesity, herbs have long been shown to be a vital and effective source of support. Herbs are not as harmful as single-compound medications, with the exception of a few allergic responses in those who are sensitive. Through a variety of mechanisms, including appetite suppression, triglyceride reduction, metabolic rate stimulation, inhibition of pancreatic lipase, and increased metabolic rate, medicinal herbs like green tea extract, Garcinia Cambogia, Glucomannan, Cayenne Pepper, Coleus Forskohlii and Bitter Orange (Table 2).
As of 2024, several weight loss drugs are available that target different mechanisms to promote weight loss. These medications are typically prescribed for individuals with obesity (BMI ≥30) or those who are overweight (BMI ≥27) with related health conditions. There are some current weight loss drugs shows in Table 3.
Approved for long-term use, orlistat is effective in reducing fat absorption. Clinical studies show that patients using orlistat can achieve modest weight loss (3-5% of body weight) over a year. However, its side effects, such as gastrointestinal discomfort and potential fat-soluble vitamin deficiencies, can limit its use [18].
Orlistat works by inhibiting gastric and pancreatic lipases, the enzymes responsible for breaking down dietary fats into absorbable forms in the intestines [19]. By blocking these enzymes, orlistat prevents the hydrolysis of triglycerides, leading to reduced fat absorption—about 30% of ingested fat is excreted undigested in the feces. This results in decreased caloric intake, promoting weight loss. Since orlistat acts locally in the gastrointestinal tract with minimal systemic absorption, it mainly affects fat absorption without influencing other nutrients.
This combination drug offers substantial weight loss (8-10% of body weight) but comes with potential risks, including increased heart rate, mood changes, and teratogenic effects. It is generally recommended for short-term use in individuals with a BMI ≥ 30 or ≥ 27 with comorbidities [20].
Phentermine-Topiramate (Qsymia) works through a combination of mechanisms to promote weight loss. Phentermine, a sympathomimetic agent, stimulates the release of norepinephrine in the brain, suppressing appetite and increasing energy expenditure [21]. Topiramate, originally an anticonvulsant, enhances the effects of GABA, inhibits glutamate, and blocks sodium channels, leading to reduced appetite and increased satiety. Additionally, topiramate can alter taste perception, reducing cravings for high-calorie foods. Together, these effects lead to reduced food intake and increased energy utilization, supporting weight loss.
Originally developed for diabetes management, liraglutide has shown effectiveness in promoting weight loss [22]. Patients may experience a 5-10% reduction in body weight, with additional benefits in glycemic control. Common side effects include nausea, vomiting, and a risk of pancreatitis.
Liraglutide (Saxenda) is a GLP-1 (glucagon-like peptide-1) receptor agonist that promotes weight loss by mimicking the effects of the naturally occurring hormone GLP-1 [23]. It works by stimulating insulin secretion and reducing glucagon release, thus improving glucose metabolism and stabilizing blood sugar levels. In addition to its effects on glucose, liraglutide slows gastric emptying and increases feelings of fullness, helping to reduce overall food intake. It also acts on the hypothalamus, the brain’s hunger-regulating center, to suppress appetite. These combined effects lead to reduced calorie consumption and weight loss.
This combination targets appetite and reward-related eating, resulting in moderate weight loss (4-8% of body weight) [24]. However, it carries risks such as elevated blood pressure, seizure risk, and psychiatric effects, necessitating careful patient selection.
Naltrexone-Bupropion (Contrave) is a combination medication that promotes weight loss by targeting the brain's reward and appetite regulation pathways. Bupropion, an antidepressant, stimulates the release of norepinephrine and dopamine, which suppress appetite and increase energy expenditure [25]. It also acts on the hypothalamus to reduce hunger and cravings. Naltrexone, an opioid receptor antagonist, blocks opioid receptors involved in the brain’s reward system, reducing the pleasure associated with eating, particularly high-calorie foods [26]. Together, these mechanisms reduce both food intake and cravings, helping individuals achieve and maintain weight loss.
A newer GLP-1 receptor agonist, semaglutide has demonstrated significant weight loss (up to 15% of body weight) in clinical trials [27]. It is particularly promising for patients with obesity and type 2 diabetes. Common side effects include gastrointestinal issues, and there is a need for long-term studies on safety.
Semaglutide (Wegovy) is a GLP-1 (glucagon-like peptide-1) receptor agonist that promotes weight loss by mimicking the action of the natural hormone GLP-1 [28]. It enhances insulin secretion while inhibiting glucagon release, leading to improved glucose control. Semaglutide also slows gastric emptying, increasing feelings of fullness and reducing overall food intake. Additionally, it acts on the appetite-regulating centers in the brain, particularly the hypothalamus, to suppress hunger and promote satiety. These combined effects lead to reduced caloric consumption and support significant weight loss in individuals using the medication.
This dual GLP-1 and GIP receptor agonist has shown remarkable efficacy in weight loss, with some studies indicating up to 20% body weight reduction [29]. It holds promise for those with severe obesity and type 2 diabetes. Ongoing trials are assessing its long-term safety and efficacy.
Tirzepatide is a dual GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide) receptor agonist that promotes weight loss and improves glucose metabolism. By activating both GLP-1 and GIP receptors, it enhances insulin secretion, reduces glucagon levels, and improves insulin sensitivity, leading to better blood sugar control [30]. Additionally, tirzepatide slows gastric emptying, which increases satiety and reduces food intake. Its action on the brain's appetite-regulating centers further suppresses hunger. These combined effects result in reduced caloric consumption, improved glucose regulation, and significant weight loss.
Targeting the melanocortin-4 receptor, setmelanotide is designed for patients with rare genetic obesity disorders [31]. Early results are promising, but its use will be limited to specific populations with genetic predispositions.
Setmelanotide is a melanocortin-4 receptor (MC4R) agonist that promotes weight loss by targeting the brain’s central energy balance and appetite regulation pathways. MC4R is a key part of the melanocortin system, which plays a critical role in controlling hunger and satiety [32]. By activating MC4R, setmelanotide reduces appetite and increases energy expenditure. It is particularly effective in individuals with rare genetic disorders, such as POMC, LEPR, or PCSK1 deficiencies, where the melanocortin pathway is disrupted. Through its action on MC4R, setmelanotide helps restore normal appetite control, leading to reduced food intake and weight loss.
(table 3)
Obesity remains a critical global health challenge with significant implications for both physical and mental health. The multifactorial nature of obesity, influenced by genetic, environmental, and behavioral factors, makes it difficult to manage. Traditional approaches, including lifestyle modifications and behavioral therapy, are essential but often insufficient for long-term success in many individuals. Pharmacological interventions, while effective, come with limitations such as side effects and varying efficacy among patients.
Recent advances in pharmacotherapy have provided hope for more sustainable obesity management. Emerging drugs, such as GLP-1 receptor agonists and dual-acting medications like tirzepatide, offer new mechanisms of action and show promising results in weight reduction. However, continued research is necessary to assess their long-term safety and efficacy. Moving forward, personalized treatment approaches that integrate lifestyle modifications, psychological support, and pharmacotherapy may be the key to addressing the obesity epidemic effectively.
Copyright: © 2024 Adinarayana Andy.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.