Aparna KS, Manoj S*, Sumitha Phatak, Sreelekha S, Unnikrishnan Nair and Supreme Goel
Chaithanya Eye Hospital and Research Institute, Trivandrum, India
*Corresponding Author: Manoj S, Vitreo-retinal Consultant, Chaithanya Eye Hospital and Research Institute, Trivandrum, Kerala, India.
Received: August 30, 2024; Published: September 13, 2024
Citation: Manoj S., et al. “Multimodal Imaging in Posterior Uveitis; Is It Necessary?". Acta Scientific Ophthalmology 7.10 (2024): 16-21.
Purpose: To study the role of Multimodal imaging in posterior uveitic entities and identify if it had a bearing on diagnostic or management decision making.
Methodology: This Prospective observational study was conducted at a tertiary care uvea practice. 43 eyes of 27 patients with clinically diagnosed posterior uveitis were enrolled. All patients underwent a comprehensive examination and Multimodal imaging including Colour Fundus photography, Multicolour imaging (MCI), Infrared Reflectance (IR) Imaging, Fundus Autofluorescence (FAF), Fundus fluorescein angiography (FFA), Indocyanine green angiography (ICGA), Spectral domain OCT (SD-OCT) and OCT angiography (OCTA) in addition to traditional investigations in Uveitis. Multimodal Imaging was performed on the Heidelberg and ZEISS system.
Results: Patients were categorized into 5 groups -Tuberculosis, Presumed ocular Sarcoidosis, VKH disease, White dot syndromes and Idiopathic. Multicolor and IR imaging were inferior to color photography in detection of disc pathology, choroidal lesions and subtle vasculitis. However; MCI was superior in detection of surface abnormalities. ICGA with FFA continues to be investigation of choice especially in WDS, vasculitis and granulomatous entities. OCT was sensitive in identifying early macular disease and EDI mode helped in identification and follow up of choroidal granulomas. New biomarkers like choroidal hyperreflective foci helped to correlate disease activity. Though sometimes unreliable, OCTA findings seemed to correlate with conventional angiography.
Conclusion: Multimodal imaging is useful in evaluation of posterior uveitis and identifies certain specific entities. This series was not all encompassing, combining various modalities helped to improve diagnosis, rule out differentials, understand pathology and treatment responses. MCI over conventional photography and OCTA over traditional angiography offer limited advantages and artifacts hinder wider applications.
Keywords:Multimodal Imaging; Mulicolor Imaging; Fundus Clinical Picture; Infrared Reflectance Imaging; Fundus Autofluorescence; Fundus Fluorescein Angiography; Indocyanine Green Angiography; Spectral Domain Optical Coherence Tomography; Optical Coherence Tomography Angiography
MCI: Multicolour Imaging; CP: Clinical Picture; IR: Infrared Reflectance; FAF: Fundus Autofluorescence; FFA: Fundus Fluorescein Angiography; ICGA: Indocyanine Green Angiography; SD-OCT: Spectral Domain Optical Coherence Tomography; OCTA: Optical Coherence Tomography Angiography; VKH: Vogt Koyanagi Harada; WDS: White Dot Syndromes; SUN: Standardization of Uveitis Nomenclature; ERM: Epi Retinal Membrane; SRF: Sub Retinal Fluid; SRD: Sub Retinal Detachment; ILM: Internal Limiting Membrane; EZ: Ellipsoid Zone; ELM: External Limiting Membrane; APMPPE: Acute Posterior Multifocal Placoid Pigment Epitheliopathy; FAZ: Foveal Avascular Zone; DCP: Deep Capillary Plexus; SCP: Superficial Capillary Plexus; MFC: Multi Focal Choroiditis; EDI: Enhanced Depth Imaging; RPE: Retinal Pigment Epithelium; HRF: Hyper Reflective Foci
Posterior uveitic entities can be infective, non-infective or part of a systemic disease; they could also be limited to the eye as an ocular syndrome without any systemic involvement [1]. Though the Standardization of Uveitis Nomenclature (SUN) [2] has defined and classified posterior uveitis, continuing advancements in ocular imaging technologies now allow for multimodal imaging and better characterization of these entities. In posterior uveitis, combining images from different modalities helps clinician to improve diagnostic yield helps in ruling out certain differential diagnosis, to assess the extent of the disease, level of activity, response to treatment, decision on stopping therapy, possible reactivation and better understanding of the natural course of the diseases. Even though the role of Multimodal imaging in the diagnosis and management of specific posterior uveitic entities have been described in select entities, no comprehensive study has been done encompassing all posterior uveitic entities in a hospital based or population-based setting.
Therefore, the purpose of this study is to describe the findings in posterior uveitis on multimodal imaging and identify if it had a bearing on diagnostic or management decision making.
In this Prospective observational study, we reviewed consecutive patients with posterior uveitis who visited the Uvea Clinic at Chaithanya Eye Hospital from October 2019 to May 2020. The study was conducted after Institutional Ethical Committee clearance, in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All the patients underwent a comprehensive examination, including Colour Fundus photography, Multicolour imaging (MCI), Infrared Reflectance (IR) Imaging, Fundus Auto Fluorescence (FAF), Fundus Fluorescein Angiography (FFA), Indocyanine Green Angiography (ICGA), spectral-domain OCT and OCT angiography (OCTA). History, examination findings and imaging results were recorded onto a data sheet during baseline and follow up. Multi modal imaging was performed on the Heidelberg (HRA-2/SPECTRALIS) and ZEISS system during baseline visit. Repeated imaging was done in select cases to understand the pattern change on resolution. Statistical analysis included descriptive statistics, where quantitative data were expressed in mean ± SD. Qualitative data were expressed in frequency.
43 eyes of 27 patients with posterior uveitis including (16 bilateral case and 11 unilateral cases) were enrolled in the study. The study sample included 11 males (40.7%) and 16 females (59.2%). The mean age of study sample was 42.85 ± 17.31.
The study comprises 27 patients with posterior uveitis, categorized into 5 major groups; Tuberculosis (5 patients), Probable ocular sarcoidosis (3 patients), Vogt Koyanagi Harada disease (10 patients), White dot syndromes (4 patients) and 5 idiopathic cases (Figure 1). Four cases of White Dot Syndromes include Serpiginous choroiditis (1 case), Multi focal Choroiditis (2 cases) and Acute posterior multifocal placoid pigment epitheliopathy (1 case).
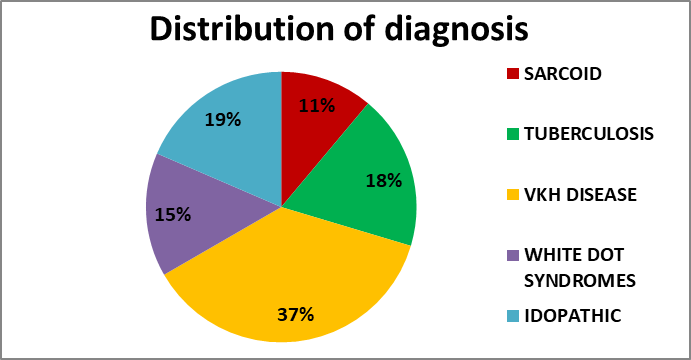
Figure 1: Posterior uveitic entities included in the study.
In our study out of 43 eyes, 25 eyes had mild to moderate vitritis which was detected by fundus color photography and OCT picked up only 13 eyes with vitritis.3 eyes had Snow balls identified by fundus CP, out of which only one case was identified in IR and Multicolor Imaging. Cases with severe vitritis were excluded from the study due to poor images.
Fundus Clinical picture showed oedematous/ hyperemic optic disc in 17 eyes, which was also detected on IR imaging as peripapillary folds in 9 eyes. MCI could identify disc pathology only in 5 eyes. FFA showed Disc leak in 26 eyes , 3 of them were not detected by any other imaging modalities. 3 eyes had peripapillary mottling also. OCT showed disc oedema in 2 eyes. In ICGA, 2 eyes had peripapillary hypofluorescent patches. In FAF, 7 eyes showed peripapillary hypoautofluorescence which correlated with the presence of disc edema. 2 eyes with disc leakage in FFA demonstrated the presence of peripapillary granulomas on OCT.
MCI showed Epiretinal membrane in 4 eyes, one of them was clinically not detectable. IR imaging and OCT could identify ERM in 2 eyes each. Sub Retinal Fluid- Out of 16 eyes with VKH, 15 eyes had Sub Retinal Detachment, picked in fundus CP. MCI could detect only 5 eyes with SRD. ILM folds were detected in 9 eyes with IR imaging and OCT, 4 eyes with MCI and 2 eyes with fundus CP. One eye had macular oedema in fundus CP and FFA. Four eyes showed vasculitis in FFA. ICGA was within normal limits in 4 eyes with peripheral vasculitis.
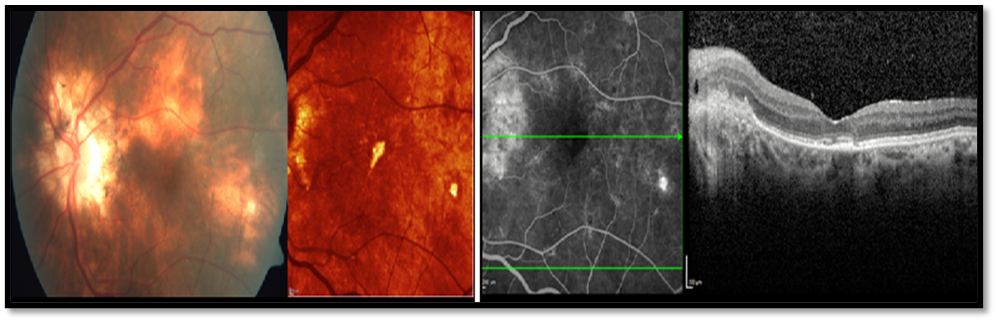
Figure 2: Fundus CP and MCI showing peripapillary granulomas and choroidal lesions. Corresponding FFA image showed hyperfluorescent lesions and OCT showed hyporeflective granulomas in a patient with Tubercular multifocal choroidal lesions.
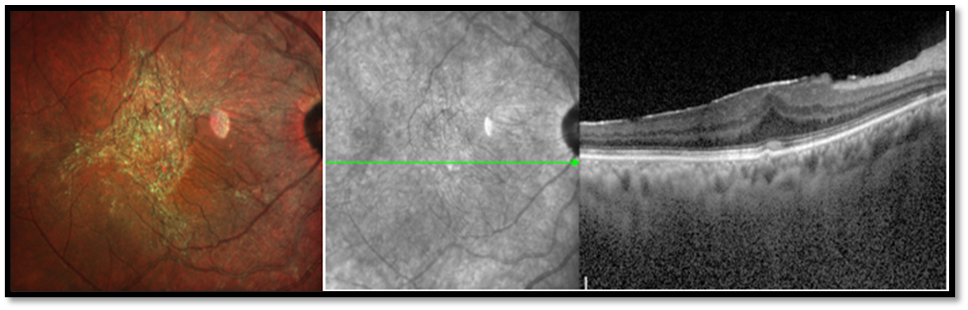
Figure 3: MCI showing ERM, which was not detected by IR imaging. OCT showing ERM with Central bouquet anomaly, in a patient with Tubercular multifocal choroidal lesions.
Choroidal nodules were picked up in 10 eyes with fundus CP. In MCI, 3 eyes showed choroidal nodules. Five eyes had Ghost maculopathy masquerading chorio retinal pathology. IR imaging showed hyperreflectance in macular area corresponding to choroidal nodules in fundus CP in two eyes, hyper reflective dots in 4 eyes. 14 eyes with multifocal choroiditis showed early hypofluorescence to later hyper fluorescence in FFA. ICGA in our study demonstrated early hypofluorescent patches persisting as hypofluorescent in late phase in the posterior pole or in the midperiphery (12 eyes) in tuberculous uveitis and ocular sarcoidosis. 2 eyes had peripapillary hypofluorescent patches. ICGA detected more lesions than FFA. While in 2 eyes with idiopathic multifocal choroiditis, they appeared hypofluorescent in early ICGA and became hyperfluorescent in the late phases. OCT imaging showed choroidal granulomas as well defined, hyporeflective lesions in 8 eyes. Choroidal folds were identified in fundus CP in 6 eyes. IR imaging could pick up choroidal folds in 10 eyes, but MCI could do so in only 2 eyes. OCT showed choroidal folds in 16 eyes, out of which 14 eyes had VKH disease with bumpy choroid. FFA and ICGA identified choroidal folds in 8 eyes each.
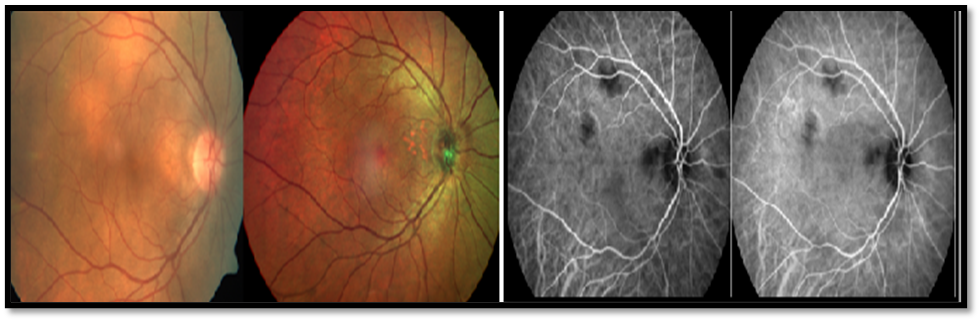
Figure 4: Fundus CP showing sub retinal yellow lesions but Multicolor imaging could not detect these choroidal lesions in probable ocular sarcoidosis. Corresponding ICGA showing hypofluorescence in the intermediate phase, this was maintained during the late phase.
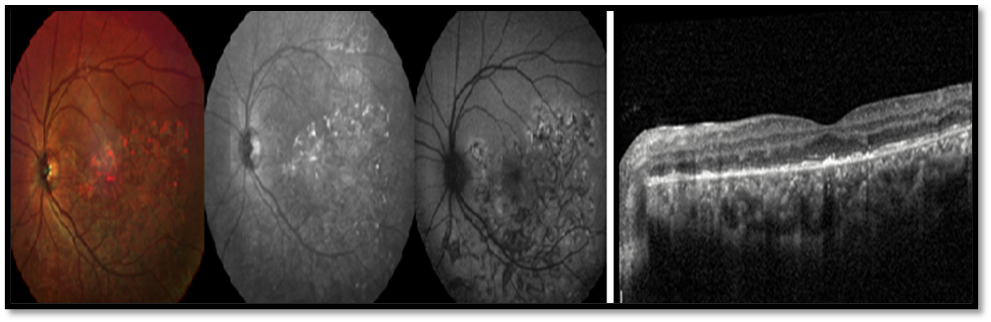
Figure 5: In an eye with serpigenous choroidopathy, MCI showing the lesions with a reddish hue and on the IR image lesions were hyperreflective. On FAF where they appeared hypo autofluorescent. OCT showed diffuse EZ loss with multiple foci of hyperreflective RPE and demonstrated HRF in the outer retina and choroid.
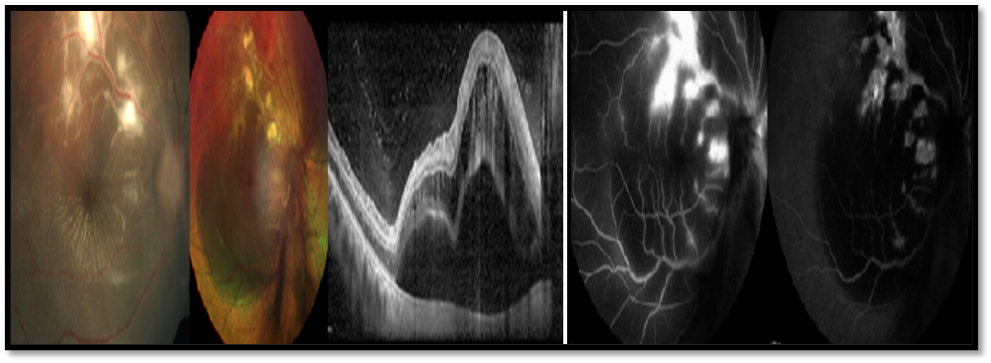
Figure 6: Fundus CP showing vasculitis, MCI picked up the retinochoroidal lesion and OCT showing serous detachment. FFA and ICGA identified the patchy vascular leakage which appeared to be venular in the periphery predominantly
The following were the other OCT findings; One eye with tubercular choroiditis showed Central Bouquet anomaly. Hyperreflective lesions spreading into the outer retinal layers correspond to changes in the cone outer segment tips were seen in 3 eyes. EZ loss and ELM loss was seen in one eye of APMPPE, 2 eyes with MFC and 2 eyes of Serpiginous choroidopathy.
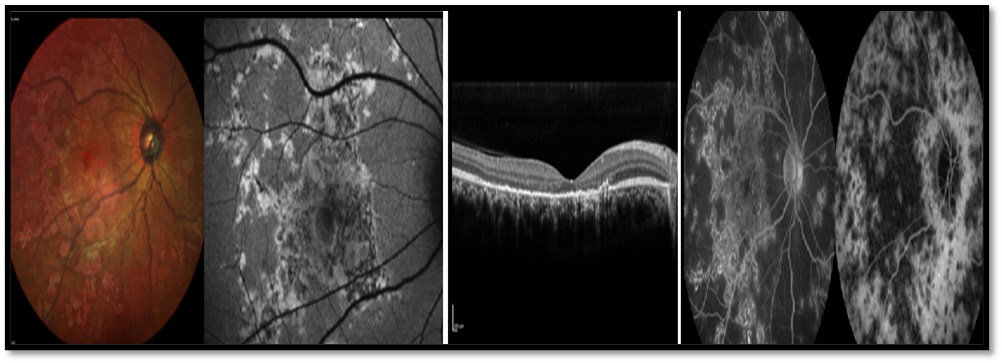
Figure 7: Multifocal choroiditis, on IR image these lesions were hyperreflective. On the OCT there was patchy EZ and ELM loss with involvement of the overlying retina also and demonstrated HRF in the outer retina and choroid. On FFA the lesions demonstrated increased fluorescence while appeared hypofluorescent in ICGA.
FAF revealed multiple patterns corresponding to serous pockets in VKH disease. Subtle hypoautofluorescent patches were seen in 7 eyes, hyperautofluorescent in 1 eye, mixed pattern with both hypo and hyper patches in 1 eye and 4 eyes showed normal FAF images. 7 eyes also showed peripapillary hypoautofluorescence which correlated with the presence of disc edema.
OCTA was done in only 11 cases which showed flow void areas in the choriocapillaris in 8 eyes and enlarged FAZ in DCP and SCP in 2 eyes.
Posterior uveitis may pose diagnostic challenge to clinicians due to their overlapping historical, clinical and imaging features. The usefulness of multimodal imaging in the diagnosis and management of posterior uveitis is highlighted in this analysis.
In our series both MCI and IR imaging were inferior to color photography in detection of disc pathology, choroidal lesions and in picking up subtle vasculitis of Tuberculous and sarcoid aetiology. But MCI identified more eyes with retinal surface abnormalities like ERM than colour photography. In VKH disease eyes, MCI and IR imaging have poor sensitivity to detect retinal and disc changes, though IR imaging was comparable to fundus photography in the detection of serous detachments. In all eyes with WDS, multicolor and IR imaging could detect the pathological lesions and was comparable to fundus photography. FAF however showed variable findings in these entities. In two patients with posterior scleritis of unknown aetiology, CP, IR and MCI could detect the presence of disc and peripapillary edema while hypoAF in the peripapillary region on FAF imaging was seen in both cases. In two eyes with vasculitis of unknown aetiology, CP detected the presence of these lesions but MCI, IR and FAF identified this in only one eye. Two eyes with idiopathic multifocal choroiditis with underlying granuloma and vasculitis of unknown aetiology revealed changes on CP and was superior to MCI, IR imaging and FAF. Newer investigations like MCI needs to be used judiciously as limited advantages were observed and artefacts continue to hinder wider applications.
In our series of Tuberculous posterior uveitis, typical tuberculous vasculitis or choroiditis were not seen. Angiography remains the mainstay in the evaluation of disc pathology (FFA) and choroidal lesions (ICGA).ICGA picked up more choroidal lesions than FFA. In FFA large choroidal granulomas show early hyperfluorescence with a dilated capillary bed, progressive increase in hyperfluorescence, and late pooling of dye in the subretinal space [3]. Out of the 6 MFC lesions picked up on ICGA, 4 eyes revealed early hypofluorescence which persisted in late phase probably denoting full thickness granulomas. Partial thickness granulomas of choroidal stroma show mass effect and appear as early hypofluorescent lesions which become isofluorescent during the late phases on ICGA [4,5]. EDI -OCT picked up features of granulomas in 3 eyes only, appearing as well defined, hyporeflective lesions. OCTA showed choriocapillary voids corresponding to the granulomas.
In Probable Sarcoid uveitis, angiography was superior in the evaluation of disc and choroidal lesions. FFA reveals focal or diffuse staining and leakage in active retinal vasculitis [6]. Our patients did not reveal any evidence of vasculitis on FFA. Subclinical papillitis may be detected as a hyperfluorescent disc on FFA, seen in 2 eyes. ICGA was more useful in detecting choroidal granulomas and picked up hypofluorescent lesions in 6 eyes. ICGA often reveals more lesions compared to FFA and can detect even very subtle lesions [7]. However, whether these lesions represented granulomas or atrophic areas was answered on OCT.
Out of the 6 eyes EDI OCT picked up features of granulomas in 3 eyes only, as well defined, hyporeflective lesions. Difference of homogenicity and non-homogenicity between sarcoid and tubercular granulomas could possibly be due to non caseating and caseating nature of the granuloma. OCTA in these 3 cases showed choriocapillary voids corresponding to the granulomas which displace surrounding vasculature of choroid.
In VKH disease, angiographic evaluation of these eyes is essential and the FFA leakages were more numerous than the hypocyanescent findings on ICGA.ICGA findings described include delayed choroidal perfusion, early choroidal stromal vessel hyperfluorescence and leakage, hypofluorescent dark dots during the early, intermediate and late phase, fuzzy vascular pattern of large stromal vessels and disc hyperfluorescence in the early and late phases [8]. VKH eyes also revealed choroidal folds with differential staining which were seen in both FFA and ICG angiography images especially in the late phases in 50% eyes. Corresponding OCT evaluation revealed typical serous detachment pockets in most eyes while some eyes revealed just intraretinal fluid. Majority of the eyes also revealed choroidal HRF. The SRF was significantly turbid in 1/4th eyes. The EDI showed diffuse thickening of the choroid with loss of normal architecture and bumpy RPE in all eyes. OCTA revealed patchy voids predominantly in the choriocapillary layer.
In eyes with WDS (serpiginous choroidopathy, MFC and APMPPE), OCT showed EZ loss with multiple foci of hyperreflective RPE with HRF in the outer retina as well as choroid in serpiginous choroidopathy and MFC but in APMPPE, OCT demonstrated similar changes with HRF in the outer retina but not in the choroid. On the FFA these lesions demonstrated increasing hyperfluorescence while they showed disappearing hypofluorescence on ICGA.
In two patients with unilateral posterior scleritis of unknown aetiology, FFA identified the typical pinpoint leaks with poolingand late hyperfluorescence due to staining of inflamed area while ICGA revealed hypofluorescent patches. OCT revealed elevated peripapillary RPE with thickened choroid. In two eyes with vasculitis of unknown aetiology, FFA was best in identifying the patchy vascular leakage more than what was seen clinically and on imaging and also detected disc leakage. On FFA, eyes with retinal vasculitis demonstrate focal, segmental, or diffuse vascular leakage due to inflammatory breakdown of blood–retinal barrier [9]. Compared with T-sign in colour Doppler imaging, which stayed positive through almost the whole course of disease, the changes of OCT were more sensitive in reflecting the response to treatment [10].
In two eyes with idiopathic multifocal choroiditis, FFA identified posterior pole pinpoint leaks with patchy vascular leakage involving the periphery. ICGA revealed early hypofluorescent patches later showing hyperfluorescence and well distributed. OCT revealed well defined homogenous hyporeflective granulomas corresponding to the ICGA. In view of the inadequacy of multimodal imaging during follow up, the importance of specific imaging modalities during follow up and recurrence could not be highlighted clearly in this study.
Multimodal imaging is useful in the evaluation and follow up of posterior uveitis. Some newer investigations like MCI needs to be used judiciously as limited advantages were observed and artifacts continue to hinder wider applications. Combined invasive angiography; ICGA along with FFA continues to be the investigation of choice in most posterior uveitis especially when clinical diagnosis is not evident. SDOCT with EDI is very useful to study the choroid structurally, helps to qualify hypoperfusion areas detected on angiography and helps to identify and follow up granulomas. New biomarkers like choroidal HRF predominate in some eyes and help to identify certain pathologies. Others like noninvasive OCTA are useful and helps to understand the degree of vascular involvement associated with choroidal pathology and correlates with conventional invasive angiography and may even add more information in select situations. Lastly performing all these investigations in the same multimodal imaging platform together or in various combinations helps us to understand the correlation of individual findings and pinpoint the anatomic foci of involvement thereby helping the physician to plan treatment modalities more effectively.
Copyright: © 2024 Manoj S.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.