Jameel A Patel*, Fahad Salem Alshahrani and Abdullah Ibrahim Altamimi
Ophthalmology Department, Security Forces Hospital, Riyadh, Saudi Arabia
*Corresponding Author: Jameel A Patel, Senior Registrar, Ophthalmology Department, Security Forces Hospital, Riyadh, Saudi Arabia
Received: August 30, 2024; Published: September 09, 2024
Citation: Jameel A Patel., et al. “Prevalence of Keratoconus During Screening Among Patients Seeking Laser Vision Correction in Riyadh, Saudi Arabia". Acta Scientific Ophthalmology 7.10 (2024): 12-15.
Background: Keratoconus (KCN) is a progressive, bilateral, and non-inflammatory corneal disorder that leads to ectasia and thinning of the central or paracentral cornea, causing substantial changes in the cornea’s shape, thickness, and biomechanical properties. This condition often results in decreased visual quality or quantity and varies in incidence based on geographic location, ethnicity, and diagnostic criteria. Typically presenting at a young age, keratoconus can profoundly affect vision and quality of life.
Methods: This retrospective study is being carried out to explore the incidence of keratoconus during screening for laser vision correction workup in Security Forces Hospital Riyadh for one year from the age group of 18 to 48 in 299 patients and 598 eyes. The diagnosis of keratoconus screening was based on the assessment of parameters derived from the Pentacam HR system (Oculus, GmbH, Wetzlar, Germany).
Results: In our data, the prevalence of keratoconus was 4.3% (13/299). According to gender, the prevalence in males was 9.26% (10/108) and 1.57% (3/191) in females. Among all patients, 3.3% (10/299) patients had bilateral keratoconus (manifest keratoconus in both eyes), and 1% (3/299) had unilateral keratoconus.
Among all patients (11.03%) 33/299 were diagnosed for Hyperopia, (55.52%) 166/299 were diagnosed for myopia, and (3.01%) 9/299 were diagnosed for anisometropia. According to gender, (9.95%) 19/191 of females and (12.96%) 14/108 of males were diagnosed for Hyperopia. While (86.91%) 166/191 of females and (83.3%) 90/108 of males were diagnosed for Myopia. Also, (3.14%) 6/191 of females and (2.77%) 3/108 of males were diagnosed for anisometropia.
Conclusion: The overall prevalence of keratoconus in the study population was 4.3%. while, Myopia was the most common refractive error, affecting 55.52% of patients. The data highlights a significant gender disparity in the prevalence of keratoconus, with males being more affected than females. More studies are important in this field to investigate the prevalence of keratoconus and to determine causes and prevention procedures.
Keywords: Keratoconus - (KCN); Laser-Assisted In Situ Keratomileusis (L ASIK); Laser Vision Correction (LVC); Ultraviolet (UV)
Keratoconus (KCN) is a bilateral, progressive, non-inflammatory corneal disorder characterized by ectasia and thinning of the central or paracentral cornea [1]. Patients usually present with decrease in visual quality or quantity or both. The pathophysiology of KC includes mainly genetic factors. However, biomechanical, biochemical, and environmental factors can also act as disease triggers [1]. The worldwide prevalence of KC is 1.38 per 1000 people [2] in Saudi Arabia it varies with regions with the highest rate of KC (0.0128%) to lowest rate (0.0014%) [3]. There are well defined bio microscopic, ophthalmoscopic, and retinoscopic signs, but topography is the gold standard for diagnosis of early disease [1]. Posterior surface changes and changes in corneal thickness are real signs of the ectatic condition because in many subclinical cases of keratoconus anterior surface may be normal [4]. Keratoconus is an absolute contraindication for corneal refractive surgery, and detection of it is very important in refractive surgical screening. It is well-known that iatrogenic ectasia is a late complication of Laser in situ keratomileusis (L ASIK) [5]. Therefore, corneal topographic and tomographic measurements have to be complete, including anterior and posterior evaluation maps, corneal surface curvature maps and pachymetric maps that can provide detailed information of suspected ectasia or high-risk corneas [6]. Aiming for a spectacle free vision, the surgeon and the patient both have high expectations following the laser vision corrective procedures. To avoid the risk of postoperative complications and achieve a good visual outcome (early and late), proper patient selection is of paramount importance. Topography is an indispensable tool for preoperative workup and decision making [2,3]. Patients with topographic abnormalities suggestive of KCN or suspect KCN are excluded.
This retrospective case study involved 5,980 eyes from 2,990 patients who were screened for keratoconus undergoing laser vision correction (LVC) workup at Security Forces Hospital Riyadh Saudi Arabia. Data collection spanned from January 2023 to December 2023. The patients under 18 years of age and those with corneal pathologies other than keratoconus, and individuals who had post refractive surgery or corneal surgery were excluded. The study was conducted in accordance with the national committee of Bio Ethics (NCBE) in Saudi Arabia accreditation number (H-01-R-069).
This study examined data retrospectively from the patients record of the patients who were attending ophthalmology department of Security Forces Hospital seeking LVC from January 2023 to December 2023. Every patient was examined by standard ophthalmological evaluation like refraction, detailed anterior segment and fundus examination, corneal topography with Pentacam HR system (Oculus, GmbH, Wetzlar, Germany) patients excluded were younger than 18 years of age and those having previous ocular surgery or trauma and who had lost follow up.
The data collected for this particular case study were gender, age , date , vision equity ,refractive errors , K readings, corneal topography , and excluded patients under the age of 18 and with oblique corneal pathologies or/with oblique previous ocular surgeries. Out of 2990 patients included in the study, 108 were males and 191 were females. The mean age of patients being 27.9, Subjects were diagnosed with keratoconus if they met at least two of the following criteria: corneal thickness below 500 µm, an asymmetric bowtie pattern on the corneal topography map, corneal steepening of 47 D or more, a skewed radial axis exceeding 21°, posterior elevation greater than 20 µm, or an inferior-superior (I-S) asymmetry over 1.4 D. Those were identified as keratoconus suspects if they met at least one of these criteria: corneal thickness below 450 µm, an asymmetric bowtie pattern on the corneal topography map, corneal steepening of 48 D or more, posterior elevation above 25 µm, or I-S asymmetry exceeding 1.6 D.
Categorical data has been summarized as absolute numbers and percentages. Continuous data summarized as mean and standard deviation (SD). Proportions in groups compared using chi square test or Fisher exact test. Comparison between groups for continuous variable performed using student’s T test or wilcoxon test. Multiple logistic regression models used to estimate the adjusted relative risk, adjusting for other predictors. The Kaplan–Meier estimator used to compare the incidence between groups.
The number of patients taken for this study were 299 with the range of their ages being from 18 to 41. The prevalence of keratoconus was 4.3% (13/299). According to gender, the prevalence in males was 9.26% (10/108) and 1.57% (3/191) in females. Among all patients, 3.3% (10/299) patients had bilateral keratoconus (manifest keratoconus in both eyes), and 1% (3/299) had unilateral keratoconus. The prevalence of keratoconus among the patients was highest in the age group of 28 to 41 years.
Among all patients (11.03%) 33/299 were diagnosed for Hyperopia, (55.52%) 166/299 were diagnosed for myopia, and (3.01%) 9/299 were diagnosed for anisometropia. According to gender, (9.95%) 19/191 of females and (12.96%) 14/108 of males were diagnosed for Hyperopia. While (86.91%) 166/191 of females and (83.3%) 90/108 of males were diagnosed for Myopia. Also, (3.14%) 6/191 of females and (2.77%) 3/108 of males were diagnosed for anisometropia.
A statistically significant difference was detected between males and females for the prevalence of keratoconus (X^2 Chi-Square, P = .024). While no significant difference was found between males and females for the refraction errors. (X^2 Chi-Square, P = .481).
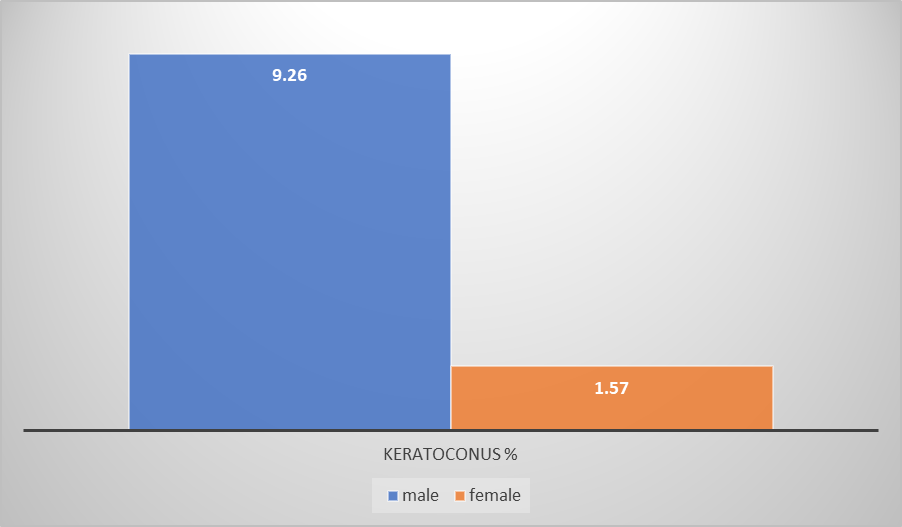
Figure 1
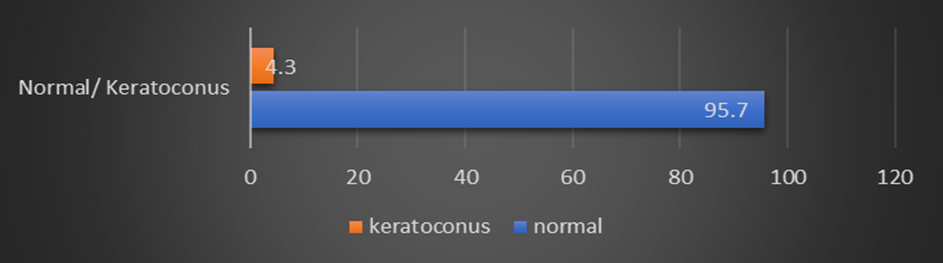
Figure 2
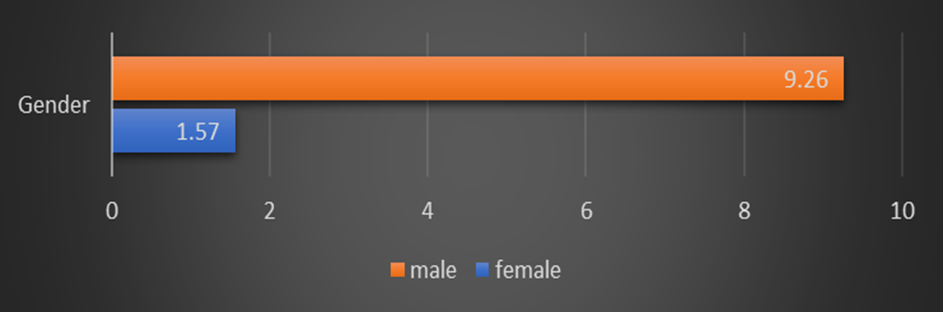
Figure 3
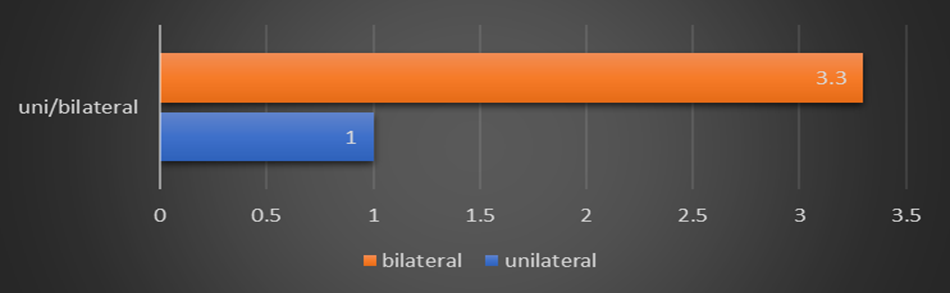
Figure 4
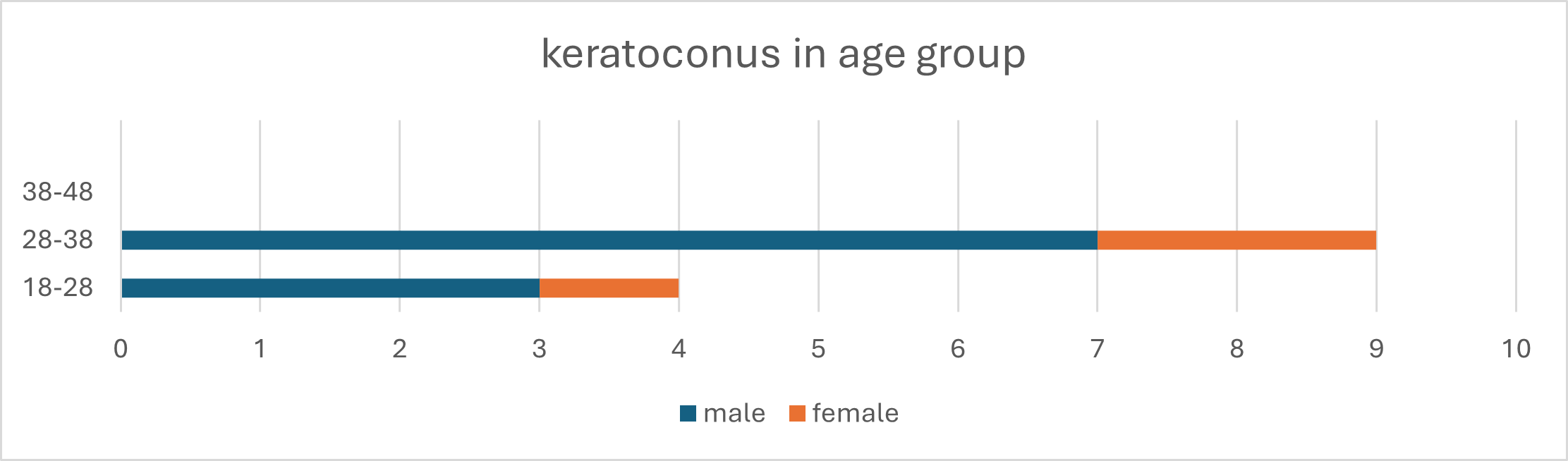
Figure 5
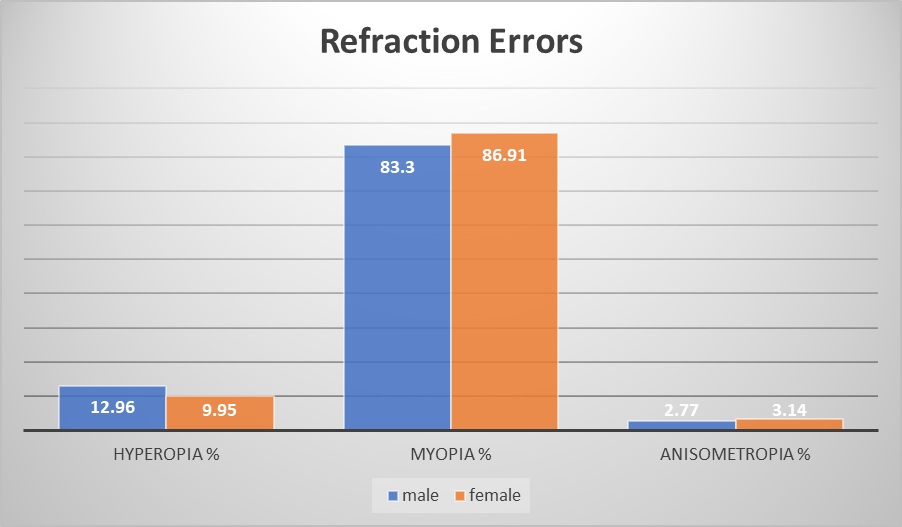
Figure 6
Keratoconus is a progressive, non-inflammatory eye condition characterized by the thinning and cone-like bulging of the cornea, leading to visual distortion [1]. In the Middle East, keratoconus has been observed at a higher prevalence compared to other regions ranging from 0.76% to 3.3% [7-11], which has prompted extensive research and clinical focus on the condition within this population.
This study were done in Riyadh, central region of Saudi Arabia, results showed an overall incidence of keratoconus at 4.3%. which is slightly higher because of the unique and focused screening sample, than the reported range of 0.03–3.18% [7] in the similar study done in Asir province of southwest Saudi Arabia, and the 2.75% incidence reported in the eastern region of the country [12]. Moreover, the other study, conducted when population density was taken into account, the hilly areas of Al Baha, Aseer, and Najran showed the greatest rate of keratoconus (0.0128%), followed by the desert region (0.0028%). The lowest rate (0.0014%) was found in coastal locations [17].
Participants in this study who were male having keratoconus 9.26% (10/108) outweighed those who were female1.57% (3/191), which is in line with other earlier findings [17]. Several factors contribute to the higher prevalence of keratoconus in the Middle East. Genetic predisposition plays a significant role, with studies suggesting that familial cases [13,14] are more common in this region. The higher rate of consanguineous marriages [15,16] prevalent in many Middle Eastern cultures is thought to contribute to the genetic transmission of keratoconus.
Environmental factors, such as high exposure to ultraviolet (UV) radiation [7] due to the region's sunny climate, have also been implicated in the increased occurrence of keratoconus. Additionally, habits such as eye rubbing, which is associated with allergic conditions like vernal kerato-conjunctivitis, are more common in the Middle East and may exacerbate the progression of keratoconus.
Clinically, the management of keratoconus has evolved significantly, with early detection and intervention becoming increasingly common. The widespread use of advanced diagnostic tools like corneal topography and tomography, including devices like the Pentacam, has improved the accuracy of keratoconus screening and allowed for earlier intervention. Treatment approaches range from conservative measures, such as the use of rigid gas-permeable contact lenses, to more advanced procedures like corneal cross-linking (CXL) [19], which has become a standard treatment to halt the progression of keratoconus. In severe cases, corneal transplantation remains a viable option, with outcomes generally favourable due to the availability of advanced surgical techniques.
The data reveals several key insights into the prevalence of keratoconus and other refractive errors among the studied population. The overall prevalence of keratoconus in the study population was 4.3%. while, refractive Errors Myopia was the most common refractive error, affecting 55.52% of patients.
The data highlights a significant gender disparity in the prevalence of keratoconus, with males being more affected than females. These findings underscore the importance of targeted screening and intervention strategies, particularly for high-risk groups. Because of this highly sophisticated early screening techniques we can filter the risky and fit patients and prevent possible complications, convincing patients about safety of refractive procedures.
The authors declared that there are no conflicts of interest.
Copyright: © 2024 Jameel A Patel.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.