Muskan Goyal1, Balbir Singh2, Indu Khosa1, Pavan Kalra3, Anand Aggarwal1*, Shubham Mittal1, Amit Chopra1, Aman Kalia1 and Divjot Kaur1
1Department of Ophthalmology, Government Medical College, Patiala, India
2Member Legislative Assembly and Honorable Health Minister, Vidhan Sabha Punjab, Chandigarh, India
3Director, Kalra Eye Hospital, Yamunanagar, Haryana, India
*Corresponding Author: Anand Aggarwal, Cornea, Glaucoma and Refractive Surgery Services, Department of Ophthalmology, Government Medical College, Patiala, India.
Received: August 13, 2024; Published: September 03, 2024
Citation: Anand Aggarwal., et al. “Evaluation of Impact of Posterior Subtenon Triamcinolone Acetonide Injection on Cataract Surgery Outcomes in Patients with Diabetes Mellitus". Acta Scientific Ophthalmology 7.10 (2024): 02-11.
Design: This was a comparative, prospective, randomized study.
Setting: Department of Ophthalmology, Government Medical College, Patiala, Punjab.
Purpose: To evaluate the impact of posterior subtenon triamcinolone acetonide (STTA) injections on visual and anatomical outcomes at end of cataract surgery in diabetic patients.
Methods: This prospective, comparative, interventional study involved 200 eyes from 100 diabetic patients undergoing bilateral cataract surgery. Patients were divided into two groups: Group A (100 eyes) received STTA at the end of surgery, and Group B (100 eyes) did not. Pre-operative and post-operative assessments included best-corrected visual acuity (BCVA), uncorrected visual acuity (UCVA), central macular thickness (CMT), intraocular pressure (IOP), and complications. Data were collected at multiple time points: baseline, post-operative day (POD) 1, 7, 28, 90, and 180.
Results: Both groups showed similar improvements in UCVA and BCVA post-surgery with no significant differences between groups. CMT measurements were significantly lower in Group A at POD 28, 90, and 180, indicating reduced postoperative macular edema. IOP remained stable and comparable between groups across all follow-up visits. Complication rates were similar, with no statistically significant differences noted between the two groups.
Conclusion: Intraoperative Posterior subtenon triamcinolone acetonide injection at conclusion of cataract surgery in diabetic patients effectively reduce postoperative macular edema without compromising visual outcomes or increasing complication rates. These findings support the use of STTA as a safe and effective adjunctive therapy in managing diabetic patients undergoing cataract surgery. Further studies with longer follow-up periods are warranted to validate these results conclusively.
Keywords: Posterior Sub-Tenon Triamcinolone Acetonide Injection; Phacoemulsification; Central Macular Thickness; Visual Acuity
Diabetes mellitus has emerged as a significant global health concern, with the World Health Organization (WHO) reporting a marked increase in cases due to lifestyle changes and economic factors [1]. Key contributors include population growth, aging, urbanization, high-fat diets, sedentary lifestyles, and obesity [2].
Diabetic retinopathy (DR) progresses from mild non-proliferative abnormalities, characterized by increased vascular permeability, to moderate and severe non-proliferative diabetic retinopathy (NPDR), marked by blood vessel closure. It culminates in proliferative diabetic retinopathy (PDR), where new blood vessels form on the retina and vitreous. In type 1 diabetes, vision-threatening retinopathy is rare in the first few years or before puberty, but nearly all patients develop it within two decades. In type 2 diabetes, up to 21% of patients have retinopathy at diagnosis, with most developing it over time. Vision loss in DR can occur due to macular edema or capillary closure impairing central vision, and PDR causing retinal distortion, detachment, and hemorrhage. New blood vessels associated with PDR can rupture, causing further vision impairment [3].
Diabetic maculopathy, particularly diabetic macular edema (DME), is the leading cause of vision loss in individuals with diabetes mellitus (DM) [4]. DME formation is primarily due to the breakdown of the inner blood-retina barrier. Diabetes alters the distribution of occludin within retinal vascular endothelium, contributing to barrier dysfunction. Müller cells proliferate, increasing microvessel permeability, while astrocytes reduce their production of glial fibrillary acidic protein, potentially affecting the blood-retina barrier's integrity. Prolonged high blood sugar levels decrease oxygen perfusion to the inner retina, triggering autoregulation that dilates arterioles and increases capillary and venule hydrostatic pressure, leading to long-term damage. This increased pressure causes fluid leakage into the extravascular compartment, which re-enters the retinal vessels through the pigment epithelial cells' pumping action [5].
Understanding the pathophysiology of diabetic macular edema (DME) informs its treatment. Grid laser treatment improves inner retina oxygenation by reducing photoreceptor oxygen consumption and shortening diffusion distance for choroidal oxygen. Focal photocoagulation targets leakage sources like microaneurysms and may enhance retinal pigment epithelium (RPE) function. Anti-VEGF medications block the permeability-inducing effects of vascular endothelial growth factor (VEGF), while corticosteroids reduce VEGF gene expression and various VEGF receptors, modulate inflammatory responses, and decrease microvascular permeability. Vitrectomy increases intravitreal oxygen levels, lowers VEGF production, and releases trapped cytokines, alleviating macular traction [6,7].
Corticosteroids, first used medically in the 1940s, have broad anti-inflammatory effects and restore the structural integrity of tight junctions, reducing paracellular permeability. They inhibit cytokines and chemokines, and modulate adenosine signaling, decreasing blood-retinal barrier permeability [8]. Studies show corticosteroids reduce multiple cytokines and chemokines in the aqueous humor, unlike anti-VEGF treatments that mainly reduce VEGF levels [9]. For eyes unresponsive to VEGF inhibitors, corticosteroids are an alternative, with Triamcinolone Acetonide (TA), dexamethasone (DEX) intravitreal implant, and fluocinolone acetonide (FA) intravitreal implant being extensively investigated for DME management.
Cataract surgery (CS) can exacerbate DME due to perioperative inflammatory responses breaking down the blood-retinal barrier [10]. While anti-VEGF agents are standard for DME treatment, they are less effective post-CS due to the involvement of other cytokines [11]. Corticosteroids are favored for reducing macular edema post-CS. Triamcinolone Acetonide (TA) is commonly used with CS due to its affordability and ease of administration, either intravitreally or as a posterior sub-tenon injection [12].
The effectiveness of different corticosteroid administration methods remains debated. Sub-tenon injections may have reduced drug penetration and shorter action duration compared to intravitreal injections [13]. However, intravitreal injections pose higher risks of increased intraocular pressure (IOP) and endophthalmitis [14]. Sub-tenon injections are easier to administer and safer, though less popular due to potential drug deposition away from the target area [15]. This study aims to quantitatively and qualitatively analyze macular changes in diabetic subjects administered with sub-tenon Triamcinolone Acetonide (STTA) compared to those not given the injection, using data obtained from optical coherence tomography (OCT).
This study aimed to evaluate the effect of triamcinolone acetate injection in the posterior sub-tenon space on macular edema and visual outcomes after cataract surgery in diabetic patients. It was a prospective, comparative, interventional study involving 200 eyes from 100 diabetic patients with bilateral cataracts undergoing phacoemulsification surgery at Government Medical College, Patiala. Patients were divided into two groups: Group A (100 eyes) received a single-dose posterior sub-tenon triamcinolone acetate (STTA) at the end of the surgery, and Group B (100 eyes) did not.
Inclusion criteria included patients aged 36-84 years, diagnosed with type 2 diabetes, managed with oral hypoglycemic agents or insulin, with controlled blood sugar levels, and undergoing uncomplicated phacoemulsification surgery. Exclusion criteria included patients with dense white cataracts, ocular conditions interfering with the study, active eye infections, recent vitreous surgery, previous use of corticosteroids, recent laser photocoagulation, recent changes in insulin treatment, anemia, pregnancy, or other chronic systemic illnesses.
Detailed histories, including age, gender, chief complaints, ocular history, systemic diseases, diabetes, smoking, and hypertension, were taken. Pre-operative workup included adiposity markers, tests for HIV/HBV/HCV status, ECG, hemoglobin, HbA1c, random blood sugar (RBS), lipid profile, urine microalbumin, and blood pressure measurement. Ocular examinations recorded corrected and uncorrected visual acuity using the Snellen chart, near vision, and intraocular pressure (IOP) using non-contact tonometry. Slit lamp biomicroscopic examination assessed the severity and type of cataract, and optic disc examination checked for diabetic retinopathy and other disorders. Biometry included keratometry values and axial length measurement. IOL power was calculated using the SRK-T formula, and the spherical equivalent was determined.
Optical coherence tomography (OCT) was performed after pupillary dilation, and macular thickness was measured using the retinal thickness map analysis protocol with an ETDRS grid. The central macular thickness (CMT) was defined as the mean thickness in the nine sections of the ETDRS grid and was used for comparisons.
The intervention involved injecting a single dose of triamcinolone acetate (40 mg in 1 ml) in the posterior sub-tenon space in Group A patients following phacoemulsification and IOL implantation, followed by a sub-conjunctival injection of gentamicin. Group B patients did not receive STTA when their second eye was operated on. The effects of STTA were analyzed by comparing best-corrected visual acuity (BCVA), IOP, and CMT pre-operatively and post-operatively on days 1, 7, 28, 90, and 180 between the two groups.
Statistical analysis was performed using SPSS software, and all results were recorded in a Microsoft Excel sheet.
The present study was conducted for assessing the effect of triamcinolone acetonide injection in the posterior sub-tenon space on the outcomes of cataract surgery in diabetics. A total of 100 diabetic patients with presence of bilateral cataract were enrolled. All the 200 eyes were randomly divided into two study groups with 100 eyes in each group; Group A: Patients who were given triamcinolone acetonide injection in posterior sub-tenon space, and Group B: Patients without triamcinolone acetonide injection in posterior sub-tenon space.
Mean age of the patients was 65.17 years. 55 percent of the patients were of urban residence while the remaining were of rural residence. Among group A patients, mean RBS and HbA1c levels at the time of surgery was 155.97 mg/dL and 6.16% respectively while mean RBS and HbA1c levels at the time of surgery among patients of group B was 156.43 mg/dL and 6.16% respectively; while comparing the results statistically in between the two study groups, non-significant results were obtained.Mean duration of diabetes was 6.45 years.Mean urine microalbumin levels were found to be 9.18 mg/L.
Mean abdominal circumference and mean waist hip ratio was found to be 94.51cm and 0.811 respectively. 15% of the patients had a BMI in the range of 18.5-22.9 kg/m2, 34% of the patients had a BMI ranging from 23.0-24.9 kg/m2, 35% of the patients had a BMI between 25.0-29.9 kg/m2, and remaining 16% had a BMI falling in the range of 30.0-40.0 kg/m2. Deranged lipid profile was seen in 65 percent of the patients. Graph 1 shows BMI distribution among patients.
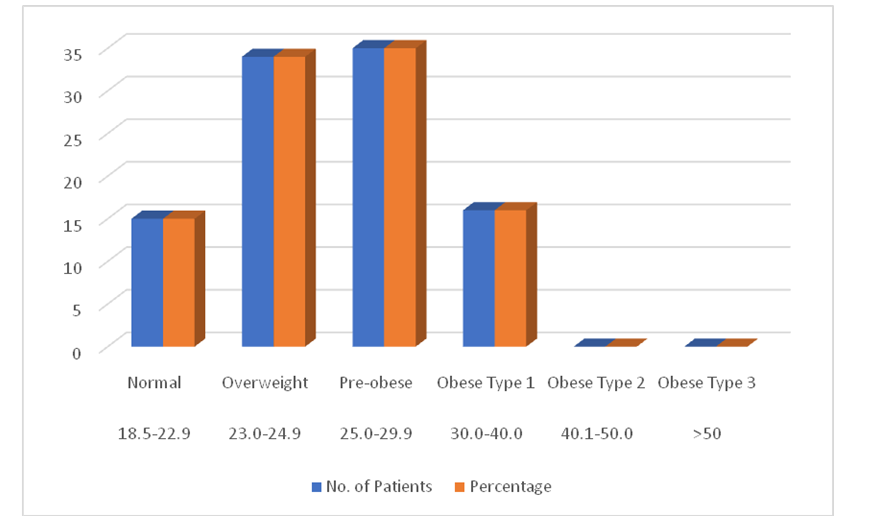
Graph 1: BMI (kg/m2).
Among group A patients, mean SBP and DBP at the time of surgery was 134.62 mm of Hg and 84.21 mm of Hg respectively while among patients of group B; mean SBP and DBP at the time of surgery was 132.23 mm of Hg and 82.31 mm of Hg respectively; on comparison statistically, non-significant results were obtained.
Among patients of group A, right eye surgery was done in 48 percent of the patients while left eye surgery was done in the remaining 52 percent of the patients while among patients of group B, right eye surgery was done in 52 percent of the patients while left eye surgery was done in the remaining 48 percent of the patients; on comparing statistically between the two study groups, non-significant results were obtained.
At baseline, 90% of Group A and 92% of Group B had UCVA between 6/24 and 6/60, while 10% and 8%, respectively, had UCVA worse than 6/60. Postoperatively, improvements in UCVA were noted across all time points (POD 1, 7, 28, 90, and 180) in both groups, with a majority achieving 6/12 to 6/18 by POD 180. Statistical analysis showed no significant differences in UCVA between groups at any time interval. Graph 2 demonstrates UCVA distribution at all time intervals while Table 1 compares mean UCVA (logMAR) at different time instances between both groups.
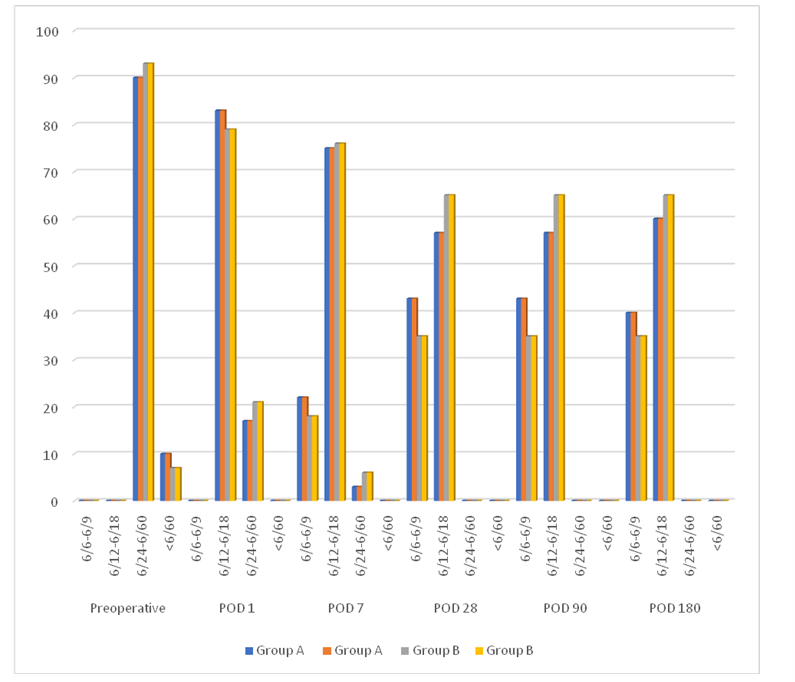
Graph 2: UCVA distribution at all time intervals
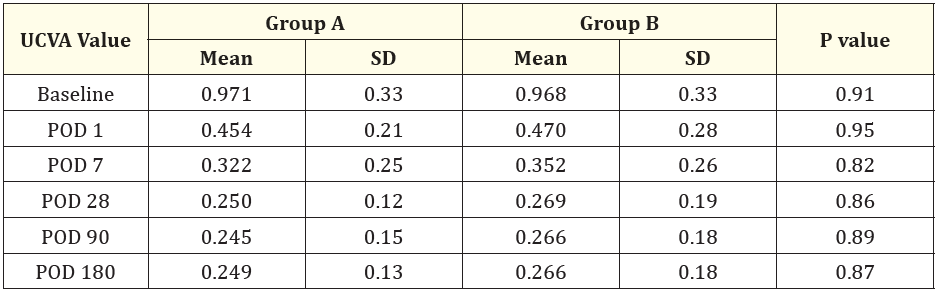
Table 1: Mean UCVA (logMAR) values at all time intervals
Similar to UCVA, BCVA improved postoperatively in both groups, with no significant differences between Group A and Group B at baseline or across subsequent follow-up periods (POD 1, 7, 28, 90, and 180). Graph 3 demonstrates UCVA distribution at all time intervals while Table 2 compares mean UCVA (logMAR) at different time instances between both groups.
Near vision outcomes were comparable between groups throughout the study period. At POD 7, 28, 90, and 180, all patients in both groups achieved near vision in the range of N8 to N6, indicating consistent near vision improvement postoperatively with no significant intergroup differences. Near vision distribution is illustrated in Graph 4.
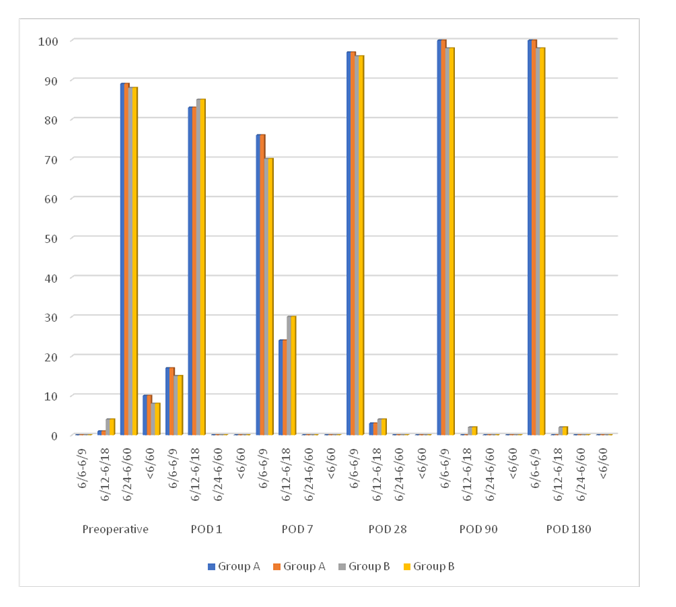
Graph 3: BCVA distribution at different time intervals.
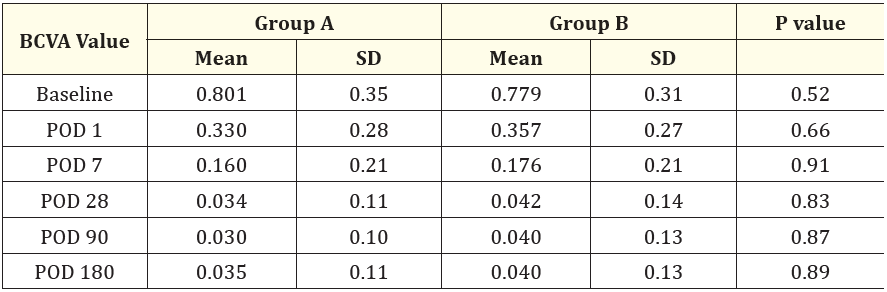
Table 2: Comparison of mean BCVA values (logMAR) at different time intervals.
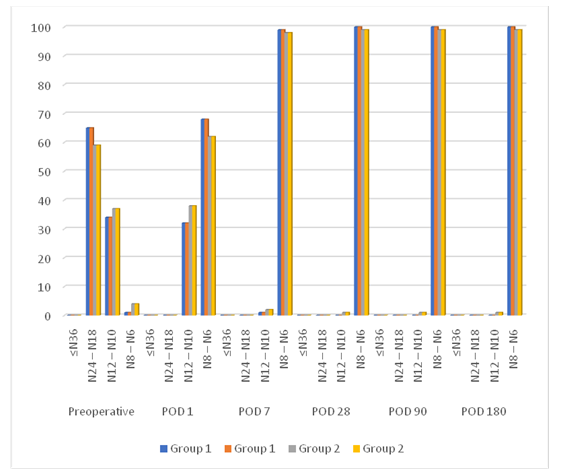
Graph 4: Comparison of distribution of near vision values at different time intervals.
Spherical equivalent refraction (SER) values showed no significant differences between Group A and Group B at POD 1, 7, 28, 90, and 180, suggesting similar refractive outcomes postoperatively in both groups. Mean SER values are recorded in Table 3.
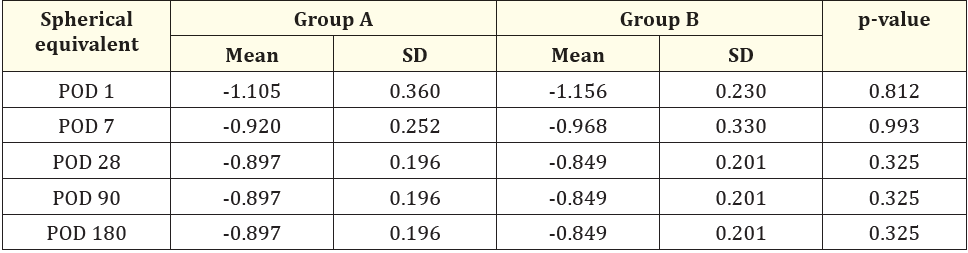
Table 3: Comparison of mean spherical equivalent values at different time intervals.
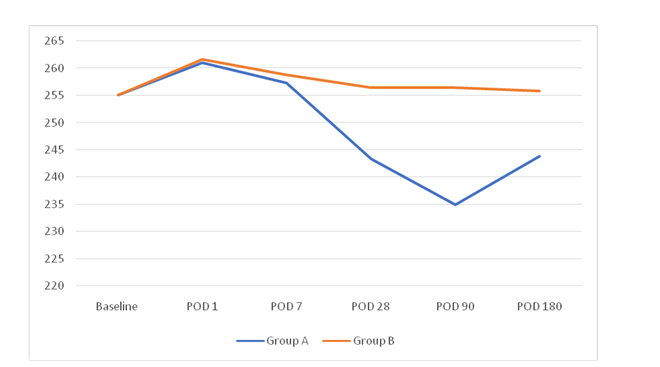
Graph 5: Comparison of CMT values at different time intervals.
Central macular thickness (CMT) measurements differed significantly between groups at POD 28, 90, and 180. Group A consistently showed lower CMT values compared to Group B at these time points (p < 0.05), indicating a potential benefit of triamcinolone acetonide in reducing postoperative macular edema in diabetic patients undergoing cataract surgery. Mean CMT values at different time instances are illustrated in Graph 5 and recorded in Table 4.

Table 4: Comparison of cmt values at different time intervals.
IOP measurements remained stable and comparable between Group A and Group B at baseline and across all follow-up visits (POD 1, 7, 28, 90, and 180), with no statistically significant differences observed. Table 5 shows IOP recording at all intervals of both the groups.
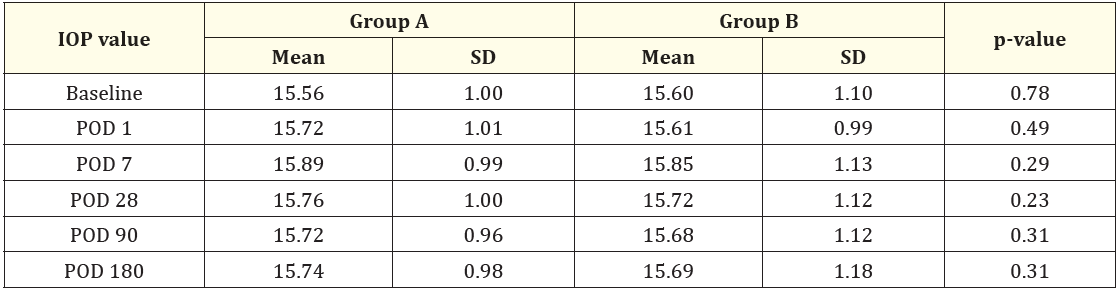
Table 5: Comparison of IOP values at different time intervals.
The incidence of complications such as pigment dispersion, striate keratopathy, wound dehiscence, corneal edema, anterior chamber reaction, retinal detachment, and vitreous hemorrhage was similar between Group A and Group B, with no statistically significant differences noted. Table 6 shows occurrence of post-operative complications in group A and group B.
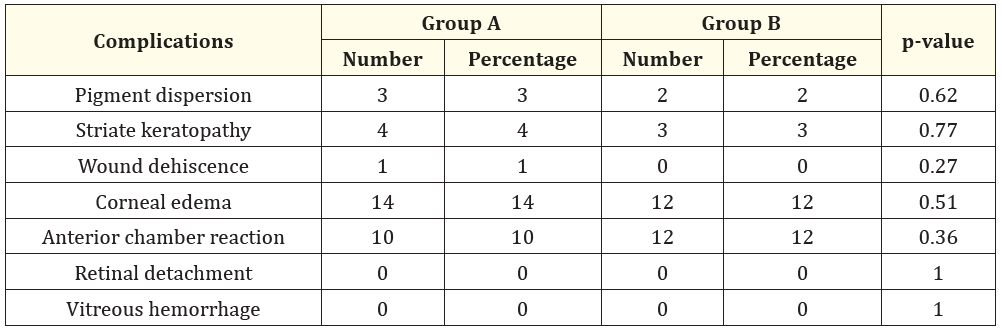
Table 6: Complications.
Diabetes mellitus (DM) is widely recognized as a leading systemic condition associated with vision impairment, particularly due to its impact on the retina, leading to diabetic retinopathy (DR) and diabetic macular edema (DME). Among individuals aged 20 to 65 years, DM stands as the primary cause of impaired visual function, underscoring the critical need for effective management strategies, especially in the context of surgical interventions like cataract surgery.
Diabetic macular edema (DME) remains a significant challenge in diabetic eye care, characterized by the accumulation of fluid in the macula due to increased vascular permeability. The pathophysiology involves a complex interplay of factors, including ischemic retinas releasing endogenous agents that compromise the blood-retina barrier, such as prostaglandins that enhance vascular permeability. While focal DME often results from microaneurysm and capillary dilation leakage, diffuse DME manifests as widespread cystoid changes due to extensive intraretinal and subretinal fluid accumulation.
Traditionally, laser photocoagulation has been effective in treating focal DME by sealing off leaking microaneurysms. However, its efficacy in diffuse DME is limited, necessitating alternative therapeutic approaches. Corticosteroids, known for their potent anti-inflammatory properties, have emerged as a viable treatment option for DME. Triamcinolone acetonide, administered via posterior sub-tenon injection (STTA), reduces inflammation by lowering levels of vascular endothelial growth factor (VEGF), thereby stabilizing the blood-retina barrier and reducing vascular permeability.
The present study aimed to evaluate the impact of single-dose STTA following cataract surgery in diabetic patients, specifically assessing its effects on postoperative outcomes such as visual acuity, macular thickness, intraocular pressure (IOP), and complications.
A total of 100 diabetic patients undergoing bilateral cataract surgery were enrolled, randomly assigned to two groups: Group A received STTA immediately following surgery, while Group B did not receive STTA. Baseline demographic characteristics, including age distribution (mean age 65.17 years, with a significant proportion aged 61-70 years), residence (55% urban), and glycemic profiles (mean RBS 155.97 mg/dL, mean HbA1c 6.16%), were comparable between the groups. This ensured a balanced starting point for evaluating the intervention's effects.
Visual outcomes were assessed through uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) measurements at multiple postoperative time points (POD 1, 7, 28, 90, 180). Both groups showed similar improvements in UCVA and BCVA over time, with no statistically significant differences observed between STTA and non-STTA groups. While there were notable enhancements in visual acuity observed, it is important to interpret these findings cautiously, considering that cataract surgery alone can independently improve visual outcomes.
Anatomical outcomes, specifically central macular thickness (CMT), were significantly reduced in Group A compared to Group B at POD 28, 90, and 180 (p-value < 0.05). This suggests that STTA effectively mitigates postoperative macular edema, potentially enhancing long-term visual outcomes in diabetic patients.
IOP, an important consideration given the potential for steroid-induced glaucoma, did not show significant differences between groups across all postoperative time points. This indicates that STTA administration did not lead to clinically significant increases in IOP, supporting its safety profile in this cohort.
Complication rates, including pigment dispersion, striate keratopathy, wound dehiscence, corneal edema, and anterior chamber reaction, were similar between groups, with no statistically significant differences observed. This underscores the safety of STTA as an adjunctive therapy in diabetic cataract surgery, corroborating findings from previous studies.
The study's findings highlight the cost-effectiveness and clinical utility of STTA in managing diabetic patients undergoing cataract surgery. By effectively reducing CMT without compromising visual outcomes or increasing complication rates, STTA emerges as a valuable therapeutic option. Its ease of administration and favorable safety profile makes it particularly suitable for integration into routine cataract surgical practice.
The study's strengths include its randomized controlled design, comprehensive assessment of various visual and anatomical parameters, and a relatively large sample size. However, limitations such as the short-term follow-up and potential variations in individual responses to treatment should be acknowledged. Future research with longer follow-up periods and larger sample sizes would be beneficial to further elucidate the long-term efficacy and safety of triamcinolone acetonide in diabetic cataract surgery.
To summarise, STTA administered in the posterior sub-tenon space following cataract surgery offers promising benefits in managing diabetic macular edema without compromising visual outcomes or increasing complication rates. This study contributes to the growing body of evidence supporting STTA's role as a safe and effective adjunctive therapy in diabetic eye care, underscoring its potential to improve postoperative outcomes and enhance patient quality of life.
Based on the findings, it can be concluded that administering triamcinolone acetonide via posterior sub-tenon injection following cataract surgery in diabetic patients led to reduced increases in central macular thickness (CMT). Uncorrected and best-corrected visual acuities (UCVAs and BCVAs) showed significant improvements throughout the postoperative period, although it is important to note that cataract surgery alone may have contributed to these improvements. This suggests that while triamcinolone acetonide injection is a cost-effective prophylactic measure for diabetic patients, mitigating postoperative inflammation and potentially reducing the risk of macular edema without causing significant adverse effects like transient intraocular pressure (IOP) elevation, further studies with longer-term follow-ups (1 year and higher) are warranted to validate these findings conclusively.
Copyright: © 2024 Anand Aggarwal.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.