Sumit Sharma1*, Tanya Gupta2, Harshita Gupta2, Shalini Singh2, Ananya Das3 and Suvarna Sharma4
1Professor and Head, Department of E.N.T., Dr. KNS Memorial Institute of Medical Sciences, Barabanki, UP, India
2Postgraduate Third Year, Department of E.N.T., Dr. KNS Memorial Institute of Medical Sciences, Barabanki, UP, India
3Postgraduate Second Year, Department of E.N.T., Dr. KNS Memorial Institute of Medical Sciences, Barabanki, UP, India
4Postgraduate First Year, Internal Medicine, GSVM Medical College, Kanpur, India
*Corresponding Author: Sumit Sharma, Professor and Head, Department of E.N.T., Dr. KNS Memorial Institute of Medical Sciences, Barabanki, UP, India.
Received: July 16, 2024; Published: September 29, 2024
Citation: Sumit Sharma., et al. “Unilateral Parotitis Presenting with Ipsilateral Sensorineural Hearing Loss – Case Report". Acta Scientific Otolaryngology 6.10 (2024):39-42.
Hearing loss as a presenting symptom of parotitis is an uncommon clinical scenario. The parotid glands play a critical role in saliva production, which is essential for digestion and oral health. However, parotitis is not commonly linked with auditory symptoms, making cases where hearing loss is a primary presenting symptom particularly intriguing. The connection between parotitis and hearing loss can be understood through the anatomical proximity of the parotid glands to the ear structures. Conductive hearing loss is more common than Sensorineural Hearing Loss (SNHI). Inflammation and swelling of the parotid glands can potentially impinge on the auditory pathway, leading to conductive hearing loss. In this study we wants to present a case of Sensorineural hearing loss associated with Parotitis reported in the department, the condition is rare hence reported; along with discuss similar cases reported in literature with reference to Incidence, management and preventive measures. Hearing loss is a rare but significant clinical scenario of Parotitis that underscores the importance of understanding the intricate relationship between the parotid glands and auditory structures. Timely diagnosis and appropriate management are essential to prevent complications and ensure optimal patient outcomes.
Keywords:Parotid Glands; Parotitis; Sensorineural Hearing Loss; Hearing Loss
Parotitis, the inflammation of the parotid glands, is a condition traditionally associated with viral or bacterial infections, autoimmune diseases, and ductal obstructions. The parotid glands, the largest of the salivary glands, are located on either side of the face, anterior to the ears and extending to the angle of the mandible. These glands play a critical role in saliva production, which is essential for digestion and oral health. However, parotitis is not commonly linked with auditory symptoms, making cases where hearing loss is a primary presenting symptom particularly intriguing.
Hearing loss as a presenting symptom of parotitis is an uncommon clinical scenario. Typically, patients with parotitis exhibit symptoms such as swelling and pain in the affected area, fever, and xerostomia (dry mouth). The connection between parotitis and hearing loss can be understood through the anatomical proximity of the parotid glands to the ear structures. Conductive hearing loss is more common than Sensorineural Hearing Loss (SNHI). Inflammation and swelling of the parotid glands can potentially impinge on the auditory pathway, leading to conductive hearing loss. Additionally, the inflammatory process can extend to the Eustachian tube or the middle ear, further contributing to auditory dysfunction (Schleuning, 2007).
Parotitis can occur in individuals of all ages, though certain populations are more susceptible. Acute viral parotitis, commonly caused by the mumps virus, is seen predominantly in children and unvaccinated individuals. Mumps parotitis can lead to significant complications, including orchitis, oophoritis, pancreatitis, and, in rare cases, sensorineural hearing loss [1]. Bacterial parotitis, often caused by Staphylococcus aureus, is more prevalent in elderly individuals, immunocompromised patients, and those with reduced salivary flow or poor oral hygiene [2].
Viral parotitis, most commonly caused by the mumps virus, can sometimes present with sensorineural hearing loss (SNHL), a condition that requires immediate and multifaceted management. Sensorineural hearing loss in the context of viral parotitis occurs due to the viral invasion and subsequent inflammation of the inner ear structures, which can damage the cochlea or auditory nerve [1]. The following discussion outlines the management strategies for this condition. Ikeda., et al. [3] states that the exact mechanism of viral-induced hearing loss is not fully understood but is believed to involve direct viral invasion and subsequent inflammatory damage to the cochlea.
The study wants to present a case of Sensorineural hearing loss associated with Parotitis reported in the department, the condition is rare hence reported; along with discuss similar cases reported in literature with reference to Incidence, management and preventive measures.
A 28 year old male presented to the Department of ENT, Dr. KNS Memorial Institute of Medical Sciences, Gadia Barabanki with complaints of swelling on the left side of the face for 7 days with mild heaviness on the cheek on the left side. There was no swelling on the right side but he felt mild discomfort on the right side. Before the swelling appeared patient had prodromal symptoms like low-grade fever, headache, malaise, myalgia, and anorexia. This lasted a few days before the swelling appeared. The swelling in the left parotid area was tender it caused pain, particularly when chewing or swallowing. Besides this patient did not have any other symptoms suggestive of other associated complications like orchitis (inflammation of the testicles) in post-pubertal males, oophoritis (inflammation of the ovaries) in females, pancreatitis, rarely, encephalitis or meningitis. Patient also complained for Hearing Loss on the side of swelling which was sudden in onset and severe because of which he could not hear from left side. He also had mild tinnitus on the left side but no vertigo.
On examination patient has a mildly tender parotid swelling on teh left side and mild tenderness on the right side with no swelling. The swelling was moderate in size. Facial nerve functions were normal on both sides. Ear examination was normal and Tuning fork test revealed Sensorineural hearing loss on the left side. There was no significant findings in Local or systemic examination.
Patient was investigated in the department and we found that
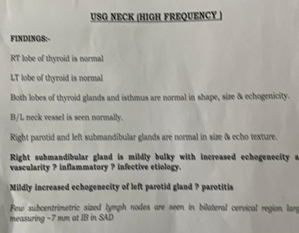
Figure 1: Ultrasound report showing Left sided Parotitis.

Figure 2: Audiometry report showing Left sided SNHI.
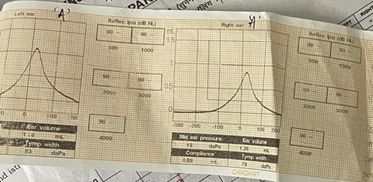
Figure 3: Tympanogram of the patient showing normal middle ear.
Viral parotitis, particularly caused by the mumps virus, can present with a rare but significant complication: sensorineural hearing loss (SNHL).
The incidence of sensorineural hearing loss in patients with viral parotitis, especially mumps, varies across studies. Historically, mumps has been a well-known cause of viral parotitis, but its complications, including hearing loss, have received varying levels of attention. According to Hviid., et al. [1], mumps-induced SNHL occurs in approximately 0.5 to 5.0 per 100,000 cases. This wide range is reflective of differences in study populations, diagnostic criteria, and methods of hearing assessment.
In contrast, a study by Kanra., et al. [4] found that SNHL was more frequent, occurring in about 1% of patients with mumps. The discrepancy in these figures may be due to underreporting, variations in the sensitivity of diagnostic techniques, or differences in population immunity levels. Vaccination rates significantly impact the incidence of mumps and its complications. Countries with high vaccination coverage, such as the United States and parts of Europe, report fewer cases of mumps and associated SNHL compared to regions with lower vaccination rates [5].
The pathophysiology of mumps-induced SNHL involves direct viral invasion and inflammation of the inner ear structures. The mumps virus can cross the blood-labyrinth barrier, leading to viral replication and immune-mediated damage within the cochlea [3]. This inflammatory process damages the hair cells and the auditory nerve, resulting in sensorineural hearing loss.
Studies such as those by Paparella and Shumrick [6] have provided histopathological evidence of cochlear inflammation and degeneration in patients with mumps-induced SNHL. Their findings showed significant lymphocytic infiltration and fibrosis in the cochlear structures. More recent studies using advanced imaging techniques have confirmed these findings, illustrating the direct impact of the mumps virus on inner ear structures.
Patients presenting with parotitis and concurrent hearing loss require a thorough clinical evaluation to ascertain the underlying cause. The clinical history should include questions about recent infections, vaccination status, autoimmune disorders, and any relevant systemic diseases. Physical examination typically reveals swelling over the parotid gland. Diagnosing mumps-induced SNHL involves a combination of clinical assessment and audiometric testing. Audiometric testing is essential to quantify the degree and type of hearing loss, distinguishing between conductive and sensorineural components. Affected individuals typically present with sudden onset hearing loss, which can be unilateral or bilateral. Audiometric evaluations reveal sensorineural patterns, often with a significant drop in high-frequency hearing thresholds. Studies comparing diagnostic approaches have emphasized the importance of early and accurate diagnosis. For instance, Kanra., et al. (2004) highlighted the utility of otoacoustic emissions (OAEs) and auditory brainstem responses (ABRs) in detecting early cochlear damage. These tests are sensitive and can identify subclinical hearing loss that might be missed by conventional audiometry. Ikeda., et al. [3] also recommended magnetic resonance imaging (MRI) to rule out other potential causes of sudden SNHL and to visualize inner ear pathology.
The management of mumps-induced SNHL is primarily supportive, with no specific antiviral treatment available for mumps. However, the use of corticosteroids has been explored in several studies with mixed results. Berrettini., et al. [7] conducted a controlled study on the efficacy of corticosteroids and found that early administration could improve hearing outcomes by reducing cochlear inflammation. Conversely, a systematic review by Wei., et al. [8] concluded that the benefits of corticosteroids in viral-induced SNHL are uncertain, with some studies showing no significant improvement. The variability in outcomes may be attributed to differences in the timing of treatment initiation, dosage, and individual patient responses. Audiological rehabilitation remains a cornerstone of management for those with persistent SNHL. Hearing aids and cochlear implants can significantly improve the quality of life for affected individuals. Berrettini., et al. [7] emphasized the importance of early audiological intervention to maximize the benefits of these devices. There is no recommended specific antiviral treatment for mumps.
Vaccination is the most effective preventive measure against mumps and its complications, including SNHL. The introduction of the mumps vaccine has dramatically reduced the incidence of the disease and its associated complications in many parts of the world. The Centers for Disease Control and Prevention [5] report high efficacy rates for the mumps component of the MMR (measles, mumps, rubella) vaccine, which has been instrumental in controlling mumps outbreaks.
However, vaccine coverage gaps still exist, leading to periodic outbreaks. The resurgence of mumps in certain areas underscores the need for maintaining high vaccination coverage and public health vigilance. Studies by Hviid., et al. [1] and others have shown that vaccinated individuals have a significantly lower risk of developing severe complications, including SNHL.
A multidisciplinary approach involving otolaryngologists, infectious disease specialists, rheumatologists, and audiologists is crucial for comprehensive management. This ensures that both the parotitis and the associated hearing loss are adequately addressed, improving patient outcomes and preventing complications [9].
Parotitis presenting as hearing loss is a rare but significant clinical scenario that underscores the importance of understanding the intricate relationship between the parotid glands and auditory structures. Timely diagnosis and appropriate management are essential to prevent complications and ensure optimal patient outcomes. Further research into the pathophysiological mechanisms linking these conditions may provide deeper insights and improve management strategies for affected individuals.
Copyright: © 2024 Sumit Sharma., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.