Gustavo Aroca Martínez1,2, Diana Marcela Perea Rojas2, Valentina Pérez Jiménez2, Kelly Katherin Hernández Rosero1,2, Carlos G Musso1,3*, Santos A Depine1,4, Andres Cadena Bonfanti1 and Joanny Judith Sarmiento Gutierrez1
1Clínica de la Costa, Department of Nephrology, Barranquilla, Colombia
2Universidad Simón Bolívar, Barranquilla, Colombia
3Research Department, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
4Confederación de Asociaciones de Diálisis de la República Argentina, Argentina
*Corresponding Author: Carlos G Musso, Clínica de la Costa, Department of Nephrology, Barranquilla, Colombia.
Received: September 20, 2024; Published: October 17, 2024
Citation: Carlos G Musso., et al. “A Descriptive Analysis of Risk Factors for Chronic Kidney Disease Among the Afro-descendant Population of San José de Saco in the Department of Atlántico, Colombia (2024)". Acta Scientific Nutritional Health 8.11 (2024):25-32.
Objective: To characterize the risk factors associated with kidney health in the Afro-descendant community of San José de Saco, a district of Juan de Acosta in the department of Atlántico, the Republic of Colombia.
Materials and Methods: In 2024, a community-based study with 217 participants was conducted in San José de Saco, Atlántico, Colombia. Data were collected on sociodemographic characteristics, vital signs, anthropometric measurements, and risk factors associated with chronic kidney disease (CKD). A descriptive analysis was conducted using Microsoft Excel. The study was performed under ethical principles according to the Declaration of Helsinki and Resolution 8430 of 1993, thus ensuring informed consent and respect for the privacy of the participants.
Results: Most participants were women (60%) in the 27-59-year age group (52%). Regarding educational accessibility, 44% had only completed primary schooling, 55% were unemployed, and 19% were not affiliated to the health system. Regarding their health status, 20% reported a personal history of high blood pressure, 4% reported type II diabetes mellitus (DM), 28% reported overweight, and 20% reported obesity. A history of low exposure to chemicals was observed (15%). Most participants (63%) found medical care accessible; however, 24% and 10% considered access to health “difficult” and “very difficult,” respectively.
Conclusion: The Afro-descendant population faces high rates of diseases such as high blood pressure, DM, overweight, and obesity, thus increasing the risk of more rapidly progressing CKD. These conditions are worsened by hindered access to medical care and limited social security coverage. Socioeconomic factors, such as unemployment and low educational levels, contribute to health problems. Implementing interventions that promote healthy lifestyles and improve equitable access to healthcare is crucial for reducing these disparities and improving the well-being of the Afro-descendant community.
Keywords: Kidney Disease; Kidney Health; Risk Factors; Afro-Descendants; Prevention; Public Health; Social Determinants
Chronic kidney disease (CKD) is defined as a decrease in kidney function over a period longer than 3 months. Chronic kidney failure occurs when the glomerular filtration rate is <60 mL/min/1.73 m2, with indirect manifestations such as changes in chronic nephropathy on imaging with kidneys reduced in size, thinning in the medullary cortex, increased echogenicity of the parenchyma or poor differentiation between the cortex and the renal sinus, presence of proteinuria, hypoalbuminemia, and active sediment in urinalysis [1,2].
CKD has become a serious public health concern with syndemic characteristics due to the diversity of variables and socioeconomic, environmental, and physical risk factors linked to predisposing or causal diseases. In addition, it generates high costs for the health system, and it represents an obstacle in the daily life of the affected population, mainly in patients with advanced CKD classified as stages 3b, 4, and 5 according to the Kidney Disease: Improving Global Outcomes guidelines [3]. This is because individuals need to interrupt work activities to undergo renal replacement therapy (RRT) every certain time, taking into account the transfer to outpatient renal units in the case of the hemodialysis-type modality [4].
The ASOCOLNEF (Colombian Association of Nephrology and Arterial Hypertension) reported to the CAC (Colombian High-Cost Accounts Fund) that, during the period from 2022 to 2023 in Colombia, 4.08% of people with CKD were in stage 5, for a total of 991,212 cases reported. Most cases resided in the city of Bogotá, the Pacific region, and the Caribbean region, respectively [5].
The San José de Saco district, considered a rural area, is the jurisdiction of the municipality of Juan de Acosta, located in the department of Atlántico on the Colombian Caribbean coast. It has a tropical dry forest-type ecosystem, a high unemployment rate where the majority of the population call themselves Afro-descendants, incomplete schooling, and problems with basic sanitation and accessibility to health services. All these create conditions that lead to the onset of risk factors, which increase the occurrence of chronic non-communicable diseases, such as CKD (6).
Identifying the proximal and distal risk factors associated with CKD should be a priority to prevent kidney damage and prevent the disease from progressing to its most invasive stages, which require RRT and kidney transplant. These risk factors should be counteracted with protective factors such as a healthy lifestyle and actions aimed at strengthening medical care, taking into account modifiable and non-modifiable factors (2,4).
Consequently, a comprehensive analysis of clinical, environmental, and socioeconomic variables that predispose to the appearance and natural progression of CKD will be conducted. This approach will be essential to design specific public health interventions that promote prevention and adequate treatment, adapted to the individual needs of the community.
A cross-sectional descriptive community research was conducted to collect information about the health status of the population and risk factors associated with the development of CKD so that preventive decisions can be made according to their needs and requirements. The study population belonged to the San José de Saco district of the municipality of Juan de Acosta (Atlántico, Colombia), with 217 participants who agreed to be part of the study in 2024.
Initially, participants were made aware of the objectives, phases, responsibilities, and importance of the execution of this project in the community, and then the survey was completed after obtaining informed consent.
This survey allowed us to determine the following aspects
A descriptive analysis was conducted based on estimations of measures of central tendency and dispersion for quantitative variables and, in turn, a calculation of relative frequency for categorical variables, using Microsoft Excel software.
This investigation had as ethical references the pillars of the Declaration of Helsinki and Resolution 8430 of 1993, whose Article 11, Chapter I, classifies it as riskless because it is limited only to the application of a questionnaire without manipulating variables intrinsic to the human being. That is, no intervention or modification of the physiological, psychological, or social variables of the study participants was conducted. In that sense, their privacy was not invaded, recognizing their right to participate in this investigation freely.
In the population under study, it was observed that 60% of participants were women and 40% were men. In terms of age, the majority was between 27 and 59 years of age (52%), followed by those 60 years or older (32%), while only 3% were under 18 years of age and 14% were in the 18-26-year range. Regarding educational level, 44% had primary education, 35% had secondary education, 12% had no schooling, 6% had technical or technological training, and only 2% had achieved university education. In terms of occupation, 55% were unemployed, 35% were self-employed, 6% were students, and 4% were dependent employees. Regarding affiliation to the SGSSS, 73% were under the subsidized regime, 19% had no affiliation, and 7% belonged to the contributory regime. This demographic and socioeconomic distribution reflects the predominant characteristics of the population, highlighting a higher proportion of women, a high unemployment rate, and a predominance of the subsidized social security regime (Table 1).
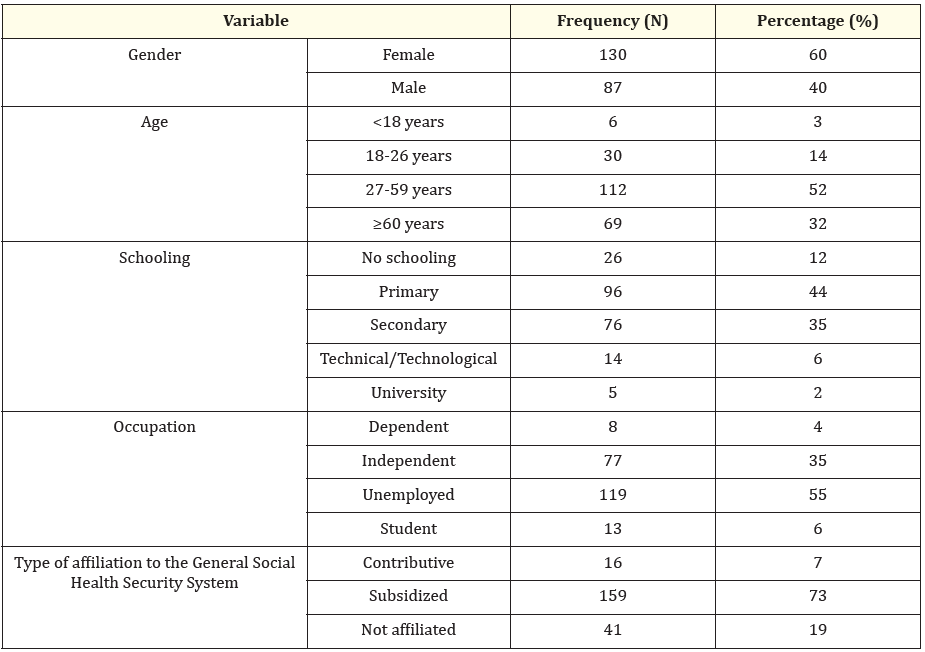
Table 1: Sociodemographic characteristics.
Regarding participants’ health factors, such as vital signs and anthropometric measurements, it was found that 80% had a systolic blood pressure of ≤130 mmHg, while 20% presented values of ˃130 mmHg. Regarding diastolic blood pressure, 54% had ≤90 mmHg, and only 4% had ˃90 mmHg. Regarding height, most participants (46%) measured between 1.50 and 1.60 m, followed by 36% with a height of 1.61-1.70 m, 12% exceeded 1.70 m, and 6% measured ˂1.50 m. Regarding weight, 42% were in the range of 61-80 kg, 34% between 41 and 60 kg, 20% weighed ˃80 kg, and 4% weighed ˂40 kg. Regarding BMI, 38% had a normal weight (18.5-24.9), 28% were overweight (25-29.9), 14% were underweight (<18.5), 15% had class 1 obesity (30-34.9), 2% class 2 obesity (35-39.9), and 3% class 3 obesity (≥40). These data provide a comprehensive view of blood pressure, height, weight, and BMI in the population, highlighting the prevalence of normal blood pressure and weight, although also evidencing a significant proportion of overweight and obesity (Table 2).
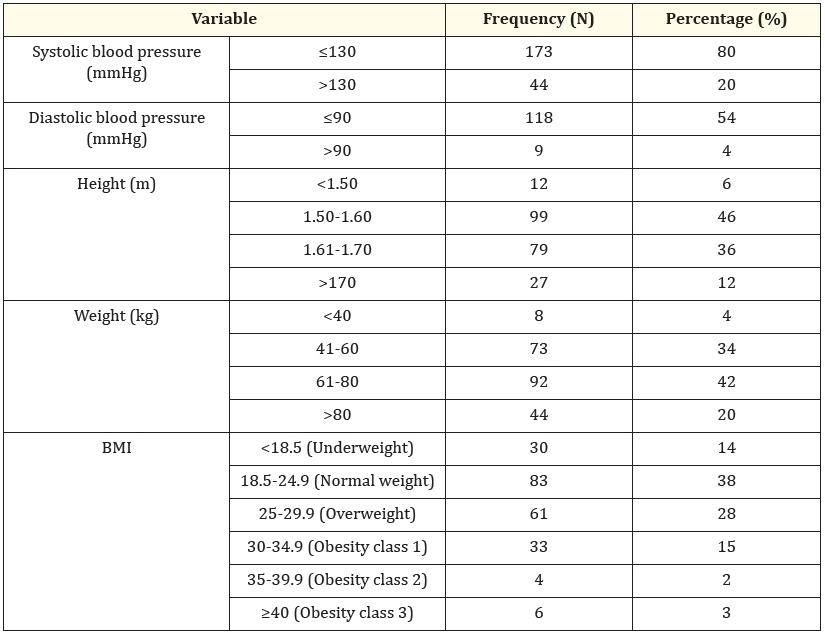
Table 2: Vital signs and anthropometric measurements.
In the analysis of the population’s personal medical history, it was identified that 20% of the participants reported high blood pressure, 4% had high cholesterol, and 4% suffered from type II diabetes mellitus (DM). In addition, 3% suffered from kidney stones, 2% had asthma, 2% had chronic gastritis, 2% had hypothyroidism, 1% had heart failure, 1% had CKD, 1% had cancer, and 1% experienced an ischemic event such as cerebrovascular accident or acute myocardial infarction. A significant number (52%) did not present any of these conditions, and 7% had other medical history (Table 3).
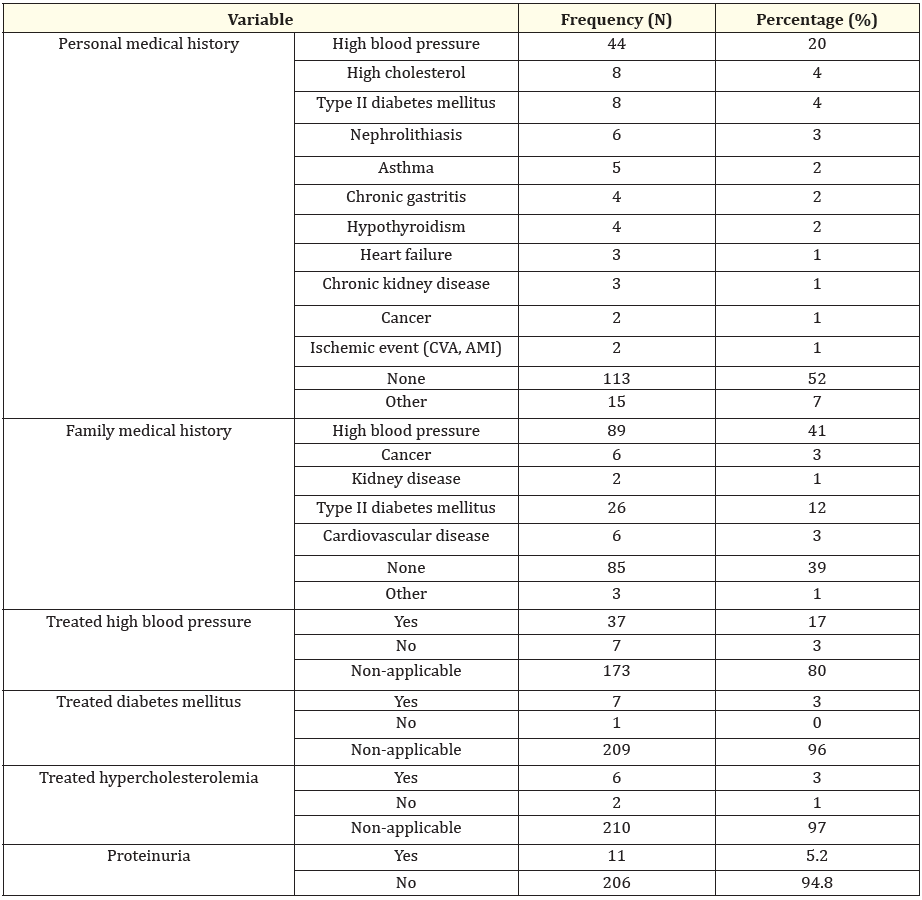
Table 3: Comorbidities.
Regarding family history, 41% reported a history of high blood pressure, 12% of type II DM, 3% of cancer, 3% of cardiovascular disease, and 1% of kidney disease. Furthermore, 39% had no family history of major diseases, and 1% mentioned other conditions (Table 3).
In terms of treatment, 17% of participants with high blood pressure were receiving treatment, while 3% were not being treated, and 80% had not this condition. In the case of DM, 3% were under treatment, <1% were not being treated, and 96% did not apply. Regarding hypercholesterolemia, 3% received treatment, 1% were not being treated, and 97% did not apply. These data highlight the prevalence and management of various chronic conditions among the population, focusing on high blood pressure and personal and family history. In addition, 5.2% of the population had protein in their urine, a key indicator of kidney disease (Table 3).
Regarding the frequency of substance use among the studied population, it was observed that 15% of participants consumed tobacco or cigarettes, while 85% did not have this habit. Regarding alcohol consumption, 46% reported consuming alcoholic beverages, compared to 54% who did not. Regarding drug use, only 2% of participants admitted to using them, while 98% did not report this behavior. These data indicate a low prevalence of drug and tobacco use but moderate alcohol consumption in almost half of the respondents (Table 4).
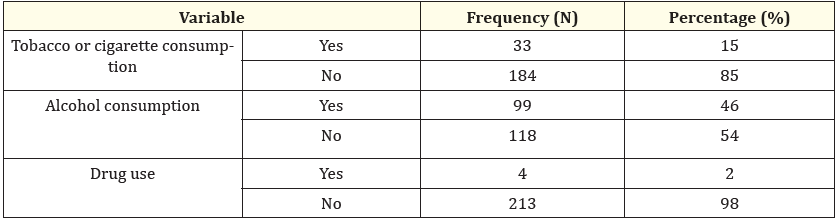
Table 4: Habits.
The analysis of exposure to chemical agents and hydration habits during the workday in the studied population revealed that 15% of participants had been exposed to agrochemicals, insecticides, nematicides, or fungicides, while 85% did not report this exposure. Regarding hydration, 48% of those surveyed consumed ˃1 l of liquid daily during work, and 18% drank ˃5 l. Also, 9% drank ˃200 cc, 6% <100 cc, 10% did not drink anything, and 9% did not know how much liquid they consumed. These results suggested that, although most of the population was not exposed to chemical agents, there was significant variability in hydration habits, with a significant proportion that could be at risk of dehydration due to insufficient fluid consumption (Table 5).
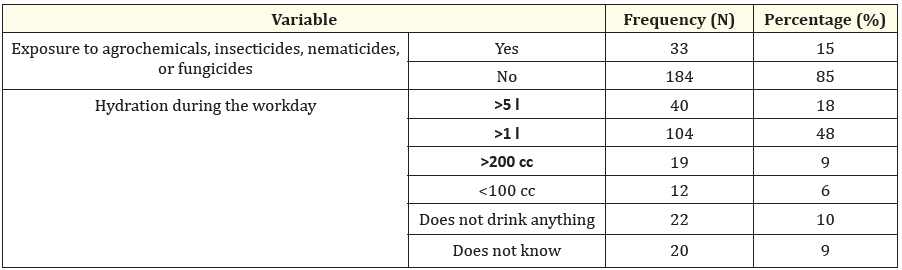
Table 5: Occupational factors.
An analysis of the frequency of medical visits and accessibility to medical care in the study population indicated that 29% of participants visited a doctor ˃3 months ago, while 21% did so a month ago and 14% a week ago. On the other hand, 10% visited the doctor ˃1 year ago and another 10% ˃2 years ago. Only 8% had their last medical visit ˃6 months ago, 5% did not remember when they had their last one, and 1% never visited a doctor. In terms of accessibility to healthcare, 63% of respondents found healthcare easy to obtain, 24% perceived it as difficult, 10% considered it very difficult, and 4% described it as very easy. These results show that, although the majority had relatively easy access to medical care, a significant portion of the population faced difficulties, which could influence the frequency of visits and health monitoring (Table 6).
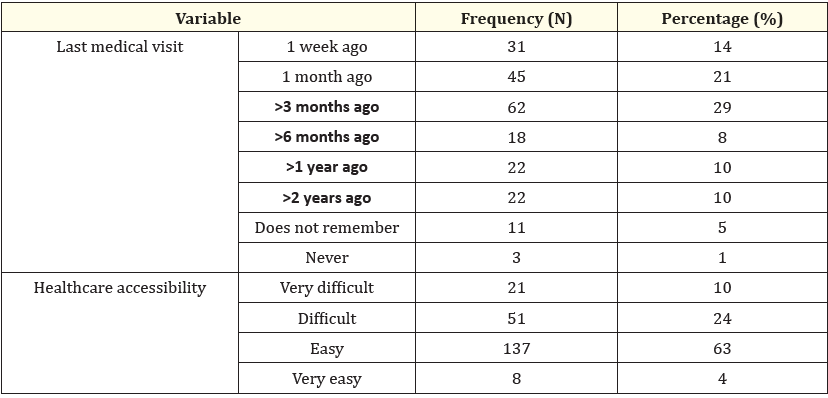
Table 6: Accessibility to the health system.
In recent years, it has been shown that the Afro-descendant population has a greater predisposition to the onset of non-communicable diseases such as high blood pressure, DM, and, consequently, CKD, taking into account lifestyle difficulties, accessibility to the health regime, and even genomics [6].
Although 63% of the population studied considered accessibility to medical care “easy,” it is striking that 24% and 10% considered it “difficult” and “very difficult,” respectively. This is attributed to the fact that 10% of participants had not attended medical checkups for ˃2 years, and there were even people who had never attended a doctor's consultation. Also, 19% were not affiliated to the SGSSS, an alarming fact since the right to health is set forth in the political constitution of the Republic of Colombia 1991 as a fundamental right [7]. Now, regarding the modifiable risk factors for the development and progression of CKD, kidney disease progresses more rapidly if they are not improved. Therefore, attendance at primary care for its prevention and treatment is of great importance for health promotion, at least annually [8].
The problem goes hand in hand with the poor schooling of the residents of San José de Saco since the majority only managed to finish primary school; that is, they do not have a high school diploma. Therefore, job opportunities and economic growth become scarcer. Due to this, 55% of the population is unemployed, and only 4% have a stable job. On the other hand, for the population not considered Afro-descendant, the DANE (National Administrative Department of Statistics) reported a total unemployment rate of 10.6% in 2023 [9].
These inequalities show the exclusion and discrimination that this population has received since colonial times, demonstrating the precariousness of their lifestyle and seriously increasing the risk factors. This information coincides with that of the study “La salud de la población afrodescendiente en América Latina” (Health of the Afro-descendant population in Latin America) by the Pan American Health Organization, which analyzed the situation in 18 countries, concluding that 80% of the countries studied had Afro-descendant people. They have a marked difference in relation to poverty, unemployment, and precarious access to health [10].
With respect to the risk factors associated with the progression of CKD, it was found that 20% had blood pressure levels outside the target values during the consultation. According to the American Heart Association 2024 [11], 20% reported having a medical history of high blood pressure, and 41% had a family history of high blood pressure. Only 17% of hypertensive people were receiving treatment, excusing themselves due to the difficult access to health centers and problems with affiliation to social security. Therefore, they did not have medications available. Regarding BMI, 8% of the studied population was overweight, and 20% were obese.
The study “Riesgo cardiovascular y factores asociados a la salud en personas hipertensas afrodescendientes residentes en la comunidad quilombola” (Cardiovascular risk and factors associated with health among hypertensive Afro-descendant people residing in the Quilombola community) conducted by Rosa, Randson, Souza., et al. demonstrated that hypertensive individuals had a higher cardiovascular risk according to the Framingham Risk Score, especially when the patient had a family history of cardiovascular disease, type II DM, overweight, obesity, and low education [11].
Obesity mainly causes metabolic syndromes, which, in the long term, are associated with HBP, insulin resistance, and, later, the development of DM, among the main causes of CKD. These diseases are related to vascular damage [12,13], produced due to oxidative stress and inflammation, among other factors, causing endothelial deterioration, leading to albuminuria. This last phenomenon can cause thrombosis because the release of vascular adhesion molecules increases and promotes greater extravasation of leukocytes, which ultimately favors the development of cardiovascular diseases [13,14]. Likewise, regarding the mechanism of stimulated hyperfiltration to satisfy the high metabolic demand, an increase in intraglomerular pressure occurs, which generates structural kidney damage, thus increasing the risk of developing CKD [15,16] and high blood pressure since higher blood pressure is required to eliminate the same amount of sodium, which leads to the development of salt-sensitive arterial hypertension [17].
Furthermore, it was found that 5.2% of the studied population had proteinuria in their urinalysis, a figure <17% observed in the general population. However, only 1% of these cases were related to CKD, although the presence of proteinuria is considered a factor indicative of kidney disease [18]. The presence of hematuria in urine was also evaluated, detected in 2.8% of the population studied, a proportion that in the world population varies between 0.5% and 2%, increasing to 20% in over 50 years of age, where it may indicate the presence of kidney disease [19,20].
Our findings underscore the urgent need for targeted interventions that address health disparities in this population. Effective strategies must include educational programs that promote healthy lifestyles, as well as public policies that improve equitable access to health services. Additionally, it is crucial to strengthen health infrastructure in underserved communities and ensure continued access to the medications and treatments necessary to manage chronic conditions.
Health inequalities among the Afro-descendant population must be addressed, therefore a comprehensive approach that considers both social determinants and biological and genetic factors is required. Only through coordinated efforts and inclusive policies can these disparities be reduced and significantly improve the kidney health and general well-being of this community in Colombia.
This study reveals an alarming situation for the Afro-descendant population in terms of kidney health and associated risk factors. The high prevalence of non-communicable diseases, such as high blood pressure and DM, among this ethnic group highlights a significant vulnerability toward the development of CKD. This vulnerability is exacerbated by multiple barriers, including difficulties in accessing the health system and limitations in social security coverage, resulting in unequal access to preventive and curative healthcare.
Furthermore, poor socioeconomic conditions such as high unemployment and low schooling contribute to an unfavorable environment for health promotion and disease prevention. Lack of educational and employment opportunities directly impacts the general well-being of the black community, thus exacerbating risk factors such as obesity and insulin resistance, which are common precursors to high blood pressure and DM.
None declared by authors.
None declared by authors.
Copyright: © 2024 Carlos G Musso.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.