Charles Masese1*, Abel Cherotich2, Timothy Wachira3, Anthony Gikonyo4, Premanand Ponoth5 and Dan Gikonyo4
1 Head Cardiology Lecturer, The Karen Hospital Medical Training College, Kenya
2 Cardiology Clinical Officer, The Karen Hospital Medical Training College, Kenya
3 Lecturer, The Karen Hospital Medical Training College, Kenya
4 Senior Cardiologist, The Karen Hospital Medical Training College, Kenya
5 Chief of Cardiothoracic and Vascular Surgery, The Karen Hospital Medical Training College, Kenya
*Corresponding Author: Charles Masese, Head Cardiology Lecturer, The Karen Hospital Medical Training College, Kenya.
Received: July 22, 2024; Published: August 16, 2024
Citation: Charles Masese., et al. “Effect of Early Anticoagulation in Post Partum Deep Venous Thrombosis as a Preventive Measure for Pulmonary Embolism -Case Report". Acta Scientific Nutritional Health 8.9 (2024): 34-36.
Background: Deep vein thrombosis (DVT) is a serious complication occasionally seen during pregnancy and puerperium. Incidence of DVT is approximately 1 in 1000-2000 pregnancies. Pulmonary embolism arising from deep vein thrombosis is one of the important causes of maternal mortality.
Objectives: To demonstrate the effectiveness of early anticoagulation in management of deep vein thrombosis in a post-partum and in prevention of pulmonary embolism.
Method: 35-year-old female who presented to the facility after being discharged a week later after successful delivery. Patient was admitted with Exertional dyspnea, palpitation, bilateral leg swelling, syncope, orthopnea and elevated levels of blood pressure. Provisional diagnosis of Post partum deep vein thrombosis with possible pulmonary embolism was made. Bilateral Doppler ultrasound confirmed the presence of DVT of the left leg. Transthoracic echocardiography (TTE) was done and showed normal cardiac functions and structure with ejection fraction of 83 percent. Computed tomography pulmonary angiogram (CTPA) confirms absence of the PE with small bilateral pleural effusion. The patient was anticoagulated with unfractionated heparin and clinical and hemodynamic response was excellent with no maternal hemorrhagic complications. Data was analyzed using images before and after the intervention.
Results: Anticoagulation is a rapid and life-saving therapeutic measure reducing the risk of developing pulmonary embolism and shortens hospital stay and post-partum mothers should be initiated as soon as possible when the diagnosis of DVT has been made.
Conclusion: Deep vein thrombosis in postpartum complicating pulmonary embolism (PE) carries a high mortality rate.
Keywords: DVT; Deep Vein Thrombosis; Pulmonary Embolism; Post Partum DVT
DVT: Deep Venous Thrombosis; ECG: Electrocardiogram; CRP: C Reactive Protein; VTE: Venous Thromboembolism; CTPA: Pulmonary Angiogram CT scan; HCARD: Higher Diploma in Cardiology; TTE: Transthoracic Echocardiogram; P/E: Pulmonary Embolism; UK: United Kingdom; CDC: Center of Disease Control; CUS: Compression Ultrasound
Pregnancy increases the risk of venous thromboembolism (VTE) 4- to 5-fold than the nonpregnant state. VTE is more common in the postpartum period The two manifestations of VTE are deep venous thrombosis (DVT) and pulmonary embolus (PE). Although most reports suggest that VTE can occur at any trimester, studies suggest that VTE is more common during the first half of pregnancy. Sequelae of DVT and PE include complications such as pulmonary hypertension, post-thrombotic syndrome, and venous insufficiency.
30-year population-based study by Heit et al documented that the risk of VTE and pulmonary embolism (PE) was 5-fold and 15-fold, respectively, in the postpartum period compared to during pregnancy.
In pregnancy, DVT is much more likely to occur in the left leg compared with the right leg. The predilection for left lower extremity DVT is postulated to be the consequence of May-Thurner syndrome, in which the left iliac vein is compressed by the right iliac artery [1].
According to the Center for Disease Control’s National Pregnancy Registry Surveillance System, between 1991 and 1999, pulmonary embolism (PE) was the leading cause of maternal mortality. Of the 4,200 pregnancy related deaths reported in the United States during those years, 20% of maternal death was attributed to PE, surpassing pregnancy-related hypertensive disorders, postpartum hemorrhage, and infection [2].
Statistically significant decrease in maternal death due to VTE in 2006-2008 era was noted after the first publication of the Royal College of Obstetricians and Gynecologist Green Top Guideline “Thrombo-prophylaxis during Pregnancy, Labor and after Vaginal Delivery” in 2004.The prevalence of VTE and associated mortality are high following surgery and in pregnant and postpartum women in sub–Saharan Africa. At least one quarter of women who are at risk for VTE in sub–Saharan Africa are not receiving prophylaxis [3].
In Kenya, DVT during pregnancy is associated with high mortality, morbidity, and increased financial implications. Pulmonary embolism (PE), its most feared complication, and is the leading cause of maternal death in the developed world. DVT can also result in long-term complications that include post thrombotic syndrome (PTS) adding to its morbidity. The current standard of care for this condition is anticoagulation. The hypercoagulable state of pregnancy likely evolved to protect women from excessive bleeding during miscarriage and childbirth [4].
35-year-old woman with history of caesarian section a week ago was admitted with leg swelling, dyspnea, palpitation and high blood pressure. Doppler ultrasound showed left popliteal-tibial-DVT. Patient was sick looking, bilateral leg swelling. There was no pallor, jaundiced, cyanosis or dehydration. BP-160/100mmhg, Heart Rate 98 beats per minute, spo2 94%, temperature 36.6 degrees.
Abdomen was Soft and non-tender; Chest was clear with normal heart Sounds. ECG showed sinus tachycardia. Echocardiography- LVEF83% with moderate TR RVSP-38mmHg.
CTPA-pleural effusion with no evidence of pulmonary embolism. Lab Elevated CRP 204.51 (0.3-1) mg/dl, otherwise findings were unremarkable.
ECG showing sinus tachycardia before treatment
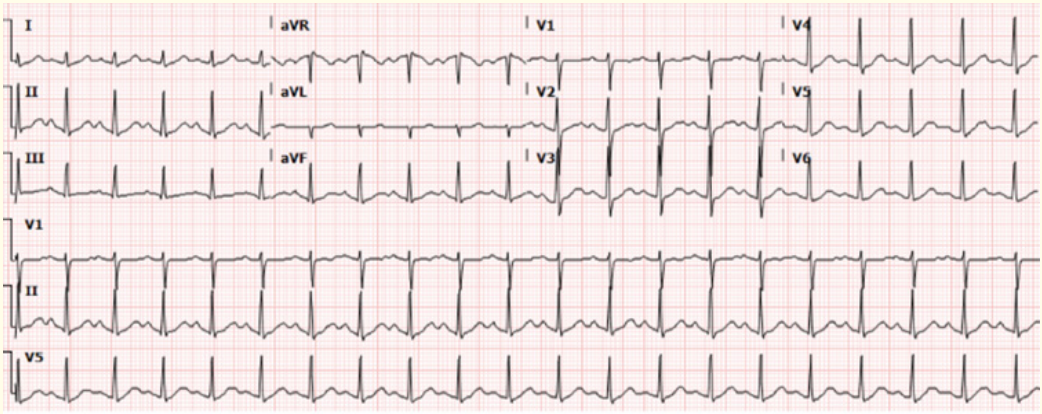
Figure a
She was anticoagulated with clexane 80 mg BD and warfarin 5mg started simultaneously till we achieved the desired INR (between 2-4) with other medication of azithromycin 500mg od, syrup ascoril 10 mls tds P.O Unicontin 400mg Od, Aldomet 250mg bd, iv Lasix 40 mg bd. Patient was in hospital for 11 days and made complete recovery and is on regular follow up. She was advised to continue anticoagulation for 6 months.
Sinus Rhythm with controlled rate after treatment

Figure b
The most important risk factors are caesarean section, post-partum and hypercoagubility states.
The current initial test of choice in the evaluation of VTE is compression ultrasound of the lower extremity veins, shown to be more than 95% sensitive and specific for proximal lower extremity DVT. The approach to manage DVT is Anticoagulation with heparin and is generally considered to be the safest treatment.
Complications from treatment such as epistaxis, hematuria, cerebral bleed are rare.
Chan., et al. used the mnemonic LEFt
Risk factors VTE remains the most common cause of maternal deaths. In pregnancy there is imbalance between prothrombotic and anticoagulant factors both increasing fibrin deposition and reduce fibrinolysis resulting in procoagulant state along with there is reduced flow velocity in the lower limbs in third trimester.
All women should be assessed for risk factors for VTE in early pregnancy, intrapartum and postpartum. The complications could be prevented with early diagnosis and therapy with favorable clinical outcomes.
Deep vein thrombosis needs emergency response in the setting of dyspnea. Anticoagulation therapy is simple and readily available, when administered quickly can help prevent further thrombus formation and thus preventing pulmonary embolism.
Copyright: © 2024 Charles Masese., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.