Sanjo K John*, M Sacratis, N Shobana, V Sadeeshkumar and CJ Selvakumar
Resident, Department of Neurology, Coimbatore Medical College, Coimbatore, Tamil Nadu, India
*Corresponding Author: Sanjo K John, Resident, Department of Neurology, Coimbatore Medical College, Coimbatore, Tamil Nadu, India.
Received: June 26, 2024; Published: August 29, 2024
Citation: Sanjo K John., et al. “Internal Carotid Artery Occlusion - Clinical Profile, Treatment, and Outcome; An Observational Study on Patients in a Tertiary Care Center”. Acta Scientific Neurology 7.9 (2024): 08-11.
Background: The presence of internal carotid artery (ICA) occlusion in patients presenting with acute ischemic stroke are still debatable. The prevalence of ICA occlusion in India is reported to be above 40%. Various management strategies are reported in the literature for ICA occlusion, with best medical therapy to be administrated urgently in order to prevent further worsening of the symptoms. This study reported the clinical profile, treatment, and outcome at discharge and at 6-month follow up in patients with symptomatic ICA occlusion.
Methodology: The study included 30 patients admitted in our institution during the study duration, with first ever acute ischemic stroke and with ICA occlusion of more than 50% identified through CV Doppler or MR angiogram. The neurological assessment and serum analysis were documented and the treatment outcome at discharge and at 6-month follow up assessed using modified Rankin scale. Spearman correlation analysis was performed to assess the relationship between the severity of occlusion and outcome in the patients recruited for the study.
Results: The mean age of the recruited patients was 55.20 ± 11.71 years, and consisting of 27 males and 3 females. The complete occlusion of the right ICA was reported in majority of the patients (26.6%), followed by 70% occlusion of the left ICA (16.6%). The mean modified Rankin score at the time of discharge was 2.77 ± 1.073, and at 6-month follow up was 1.40 ± 0.968. There was no relationship identified between the severity of ICA occlusion and outcome in the patients with symptomatic ICA occlusion.
Conclusion: The study concludes that the outcome of patients at the time of discharge or at 6-month follow up does not depend on the severity of ICA stenosis, suggesting the possibility of other factors influencing the outcome. The best medical therapy found to be effective in symptomatic patients with ICA occlusion, with no mortality or a recurrence of neurological symptoms reported during the study period.
Keywords: Acute Ischemic Stroke; Internal Carotid Artery Occlusion; Modified Rankin Scale; Best Medical Therapy; Dual Antiplatelet Therapy
The spectrum of clinical manifestations due to an occlusion of internal carotid artery (ICA) ranges from no symptoms to a fatal cerebral stroke. The presence of ICA occlusion may increase the risk for stroke even in patients who are asymptomatic due to atherosclerosis. In the earlier literatures published before 1985, the risk of cerebral infarction with ICA occlusion was 23.5% [1]. But the mortality rate reported in the study was low (8.5%) during a follow-up period of 5 years. However, studies report a 100% increase in the incidence of stroke, when comparing data from 1970 and 2010 [2]. The prevalence of carotid artery stenosis in acute ischemic stroke patients in south India was reported to be approximately 46% [3]. This was similar to the crude prevalence reported by Kamalakannan., et al., in their systematic review of epidemiological studies from different parts of India (44.29559/100,000 persons) [2].
The observational study conducted by Barnett., et al., reported an incidence of 1039 strokes in 749 patients who had symptomatic internal carotid artery stenosis during a follow-up of five years [4]. They pointed out the reasons for stroke in these patients include disorders of heart and occlusions in small penetrating arteries. Bharathi., et al., suggested older age, male gender, presence of hypertension, diabetes, and hyperlipidemia, and smoking are leading causes for increased risk for carotid stenosis [3].
Management of ICA occlusion in patients with acute ischemic stroke include stenting and mechanical thrombectomy, which was reported to have better functional outcome and higher recanalization when compared to intra-arterial thrombolysis [5]. The management strategies are focussed on early restoration of blood flow and prevent risk of an event of stroke [6]. The recurrent ischemic stroke rate in those who underwent interventional management for ICA occlusion is reported to be 2.4% annually (95% CI: 1.5 to 3.6) [7]. The systematic review by Mokin., et al., reported 11.1%symptomatic intracerebral haemorrhage in patients underwent intra-arterial endovascular therapy when compared to 4.9% in those who underwent intravenous systemic thrombolysis for strokes secondary to ICA occlusion, and was statistically significant (p = 0.001) [8]. In a large population study of 8200 symptomatic patients with ICA occlusion, significantly lower rates of neurological symptoms were reported between the index event and carotid endarterectomy in those who received best medical therapy (1.6%; 95%CI: 0.5 to 4%) when compared to those who did not receive medical therapy (25%; 95%CI: 20 to 30%; p < 0.00001) [9].
Ischemic stroke related to ICA occlusion are usually reported to be severe, with higher rates of hospital admissions as well as mortality, and poor outcome. This study aims to determine clinical profile and the treatment of patients with symptomatic ICA occlusion and their outcome after six-month follow-up in a tertiary care center in south India. The study also assessed the relationship between the severity of ICA occlusion and the outcome of patients during discharge and at follow-up.
The study was conducted in our institution, which is a tertiary care multispeciality hospital in south India. An observational cross sectional study design was undertaken, recruiting patients admitted in the Neuromedicine ward and ICU between July 2023 and December 2023 with cerebral stroke. Study included patients of all gender above the age of 30 years, with first ever acute ischemic stroke and internal carotid artery occlusion more than 50% in CV Doppler or MR angiogram studies. Signed informed consent was obtained from the caregivers prior to recruitment to the study.
Detailed neurological assessment was performed for those patients who were eligible for the study. Serum values of Hb, MCV, ESR and RBS were documented. The patient outcome at the time of discharge and after 6-month follow up was assessed using modified Rankin scale.
Descriptive statistics was utilised to summarise the study results. The demographic details and other parameters were analysed and their mean values are reported in the study. The relationship between the severity of occlusion and the outcomes assessed using modified Rankin scale was assessed using spearman correlation analysis. The statistical significance was kept at p < 0.05. The analysis was performed using IBM SPSS statistical software (version 20.0).
A total of 30 patients were identified for the study, consisting of 27 males and 3 females. The mean age of the study population was 55.20 ± 11.71 years, ranging from 35 years to 72 years. The mean duration of hospital stay of the patients were 11.30 ± 4.82 days. Among the patients, 50% had ischemic stroke with left hemiparesis and 46.6% had right hemiparetic stroke. One patient was diagnosed with posterior circulation stroke without motor deficits.
On evaluation, seven patients (23.3%) had a history of diabetes and nine (30%) had hypertension. A previous history of coronary artery disease was reported by 10 patients. The serum evaluation reported a mean Hb value of 13.62 ± 1.37, mean MCV of 81.77 ± 21.07, mean ESR of 27.53 ± 10.86, and mean RBS of 162.17 ± 63.24.
The occlusion of ICA and other major arteries were assessed using CV Doppler or MR angiogram. One patient found to have 60% occlusion of left common carotid artery (CCA), and one had 50% CCA and 100% vertebral artery (VA) on the right side. Other patients were reported to have isolated occlusion of right or left ICA, which is summarised in figure 1.
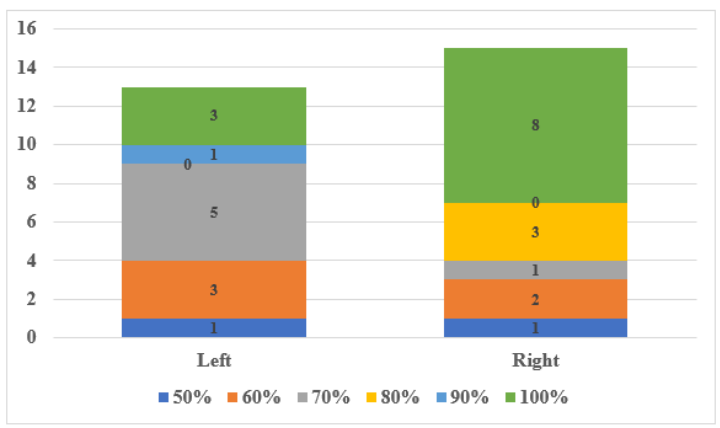
Figure 1: Distribution of ICA occlusion severity among the study population.
All patients received dual antiplatelet therapy as the best medical therapy during their stay in hospital. On discharge, the mean modified Rankin scale score at discharge was 2.77 ± 1.073, with a minimum score of 0 and maximum of 4. The patients were under direct follow-up of six months. The mean modified Rankin scale score at the end of follow up was 1.40 ± 0.968, ranging from 0 to 3.
On evaluating the relationship between the severity of occlusion and the outcome assessed using modified Rankin scale, there was no significance observed for the scores at discharge (ρ = -0.136, p = 0.472) and at 6-month follow up (ρ = -0.065, p = 0.734). However, significant correlation between the outcome assessed at discharge and at 6-months follow up was observed among the study population (ρ = 0.856, p < 0.0001).
The study identified 30 patients admitted in our institution during a period of six months with diagnosis of acute ischemic stroke and having ICA occlusion of more than 50%. It was also interesting to note that the complete occlusion of the right ICA was reported in majority of the patients (26.6%). We also identified that the severity of the occlusion does not have any relationship with the outcome after medical management or during a six month follow-up. The study also reported no mortality among the recruited patients at discharge or at follow-up. This suggest the role of various other factors determining the outcome of patients with acute ischemic stroke and an occlusion of ICA.
Paciaroni., et al., in their study reported a 45% mortality rate in those with first ischemic stroke and ICA occlusion [10]. They also found 75% of the study population to be functionally dependent at a mean follow-up of 1.2 years, suggesting the role of ICA occlusion in patient outcomes. The findings of this study was contradicting with our findings. However, the study by Burke., et al., on 4144 patients from the Canadian Stroke Registry found severe stenosis of ICA to have associated with lower risk of in-hospital death (OR = 0.40; 95%CI: 0.20 to 0.79) but to have poor functional outcome (OR = 0.62; 95%CI: 0.41 to 0.94) [11].
Our findings were in par with the findings by Verlato., et al., suggesting ICA occlusion a relatively benign condition in symptomatic or asymptomatic patients [12]. They also suggested an atherosclerotic occlusion of less than 75% does not worsen the outcome in patients with acute ischemic stroke.
Dual antiplatelet therapy was administered to all the patients in the study as part of the best medical therapy. The meta-analysis performed by Meershoek., et al., reported lower rates of 1-year any-stroke-or-death-free survival after best medical therapy (81.2%) when compared to carotid endarterectomy (96.1%) or carotid artery stenting (94.4%), suggesting best medical therapy not superior to other interventions [13]. However, studies have suggested early administration of aggressive best medical therapy to significantly reduce neurological symptoms in those who were indicative of carotid endarterectomy [5,9]. Our study reported no mortality and with better outcome assessed using modified Rankin scale, suggesting best medical therapy to be effective in symptomatic patients with ICA occlusion.
This study pose few limitations with regard to the lower sample size and minimal follow-up of the patients. However, the study provides the clinical picture of patients in our institution admitted with ICA occlusion of more than 50% and presented with acute ischemic stroke.
The study concludes that the outcome of patients at the time of discharge or at 6-month follow up does not depend on the severity of ICA stenosis, suggesting the possibility of other factors influencing the outcome. The best medical therapy found to be effective in symptomatic patients with ICA occlusion, with no mortality or a recurrence of neurological symptoms reported during the study period.
Nil.
Nil.
Nil.
Copyright: © 2024 Sanjo K John., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.