Sukumar Sura*, Rajendra Reddy, Abhinandan Reddy M, Tulsi Ram, Harshit Dave, Padma Ravikanti and Naresh Kumar Padigamarry
Department of Spine Surgery, Asian Spine Hospital, Hyderabad, India
*Corresponding Author: Sukumar Sura, Department of Spine Surgery, Asian Spine Hospital, Hyderabad, India.
Received: June 17, 2024; Published: August 26, 2024
Citation: Sukumar Sura., et al. “Management of Ventral Epidural Abscess by Endoscopic Approach in a Young Patient: A Case Report”. Acta Scientific Neurology 7.9 (2024): 04-07.
Background: Epidural abscess occurring because of spondylodiscitis requires prompt intervention. Posterior interlaminar and transforaminal endoscopic techniques have gained popularity in the recent past as an effective intervention for discectomy and decompression. Endoscopic techniques can be very promising in treating lumbar epidural abscess. We report a case of ventral epidural abscess resulting from pyogenic spondylodiscitis that was treated successfully by posterior Interlaminar approach.
Case presentation: Our patient was a 17-year-old boy presented with severe back pain, urinary retention and inability to walk due to pain and weakness of both lower limbs. Magnetic resonance imaging revealed ventral epidural abscess accompanied by spondylodiscitis of L3-L4, giving radiological picture of Pott’s spine. We performed endoscopic decompression of the neural elements by removal of epidural abscesses via posterior interlaminar approach. Immediate pain relief was achieved along with improvement in motor power of lower limbs. Culture sensitivity yielded Staphylococcus aureus and patient responded well for antibiotic therapy given for a period of 6 weeks.
Conclusion: Posterior interlaminar endoscopic approach allows us to access the epidural abscesses easily, with effective drainage of the abscess in a least invasive manner possible to the patient.
Keywords: Interlaminar Endoscopy; Epidural Abscess; Spondylodiscitis
Psoas and epidural abscesses are usually the result of pyogenic spondylitis or due to Pott’s spine [1]. Management by antibiotic therapy alone would suffice most of the times; however, surgical intervention and drainage of abscess becomes necessary if it’s a large abscess or when antibiotic therapy proves ineffective [2]. Surgical debridement and decompression of neural elements by open surgery has been the time-tested practice; however, CT or USG guided drainage have become common now a days because of less invasiveness [3]. Open surgery is practiced when percutaneous drainage proves ineffective. Transformational and Interlaminar endoscopic techniques are usually used for discectomy and decompression [4]; Off late endoscopy in spine surgery is being used extensively to address various pathologies of Spine. Endoscopic technique helps us to reach the abscess easily and to perform lavage and drainage efficiently in least invasive way compared to traditional open surgery. We here report a case of ventral epidural abscesses in a patient with pyogenic spondylodiscitis treated successfully by endoscopic decompression.
A 17-year-old boy who presented to us with inability to walk due to severe back pain and both lower limb weakness along with urinary retention. Magnetic resonance imaging (MRI) revealed ventral epidural abscesses accompanied by spondylitis at L3- L4 leading us into making provisional diagnosis of Pott’s spine. His lab reports showed white blood cell count of 14700/mm3, C-reactive protein level of 42.5mg/L and ESR being 40 mm after one hour. On admission, he was afebrile. On examination his lower limb power was as follows: hip flexor, 4/5; knee extensor, 3/5; ankle extensor, 4/5; and ankle flexor, 5/5. MRI demonstrated ventral epidural abscess extending from upper end plate of L3 to lower end plate of L4 with hyper intensity signal on T2 weighted images with enhancement on gadolinium contrast in L3 and L4 bodies suggestive of spondylodiscitis (Figure 1). As the patient presented with neurological deficits and urinary retention, without any delay we went ahead with posterior interlaminar endoscopy at L3-L4 level and cleared ventral epidural abscess under general anaesthesia. The sensation and power in the lower limbs improved after the surgery along with significant relief from the pain. Purulent material collected intraoperatively was sent for culture sensitivity testing, HPE and also for TB PCR to detect tubercular bacilli. To our surprise culture grew Staph aureus sensitive to Linezolid and Meropenem. Specimen tested negative for tubercular bacilli and our diagnosis confirmed with biopsy reports. Antibiotic therapy with Linezolid and Meropenem was continued for 6 weeks. Patient improved significantly and regained the ability to walk as the inflammatory reaction subsided. The altered sensations around his knee and leg were recovered. No recurrence of pyogenic spondylitis or psoas abscess was observed. At six weeks follow-up, the pyogenic spondylodiscitis was healed significantly with good clinical and radiological improvement.

Figure 1: Magnetic resonance images of the lumbar vertebra before surgery. T2-weighted magnetic resonance imaging a. L3-4 level, b. sagittal view, and c. coronal magnetic resonance imaging showing vertebral abscess.
Our patient was placed prone on a Jackson Table. Endoscopic procedure was performed under general anaesthesia. Level marked under fluoroscopic guidance and endoscopic portal was made such that endoscope with its working channel landed on spino-laminar junction of L3 on right side (Figure 2,3). L3 hemilaminectomy was carried out with the help of drill sparing adequate amount of pars and facet. Dorsal epidural space was reached, the dural sac with the corresponding traversing nerve root identified and gently retracted away to reach the ventral epidural abscess. Under clear endoscopic vision epidural abscess was cleared completely freeing the dura and nerve roots (Figure 4). The material was sent for Culture sensitivity and HPE.A piece of disc was also removed which was found to be friable.
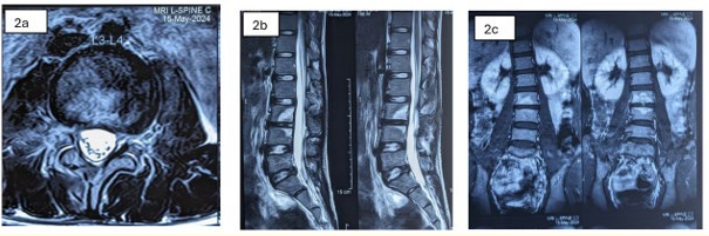
Figure 2: Magnetic resonance images of the lumbar vertebra at 6 weeks after surgery. a Axial , b sagittal and c coronal T2-weighted magnetic resonance imaging showing the marked improvement of the abscess status with neural elements free of compression.
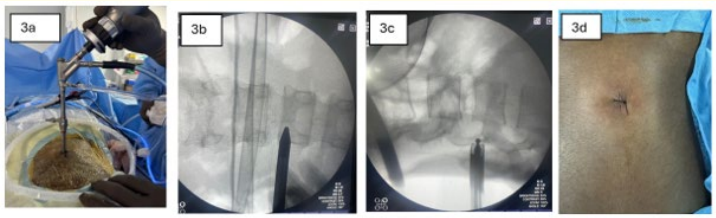
Figure 3: 3a, image of spine endoscopy being performed; 3b, docking point for endoscope marked over skin under fluoroscopy, 3c, L3 lamina being drilled, 3d, surgical port closed with single non absorbable suture.
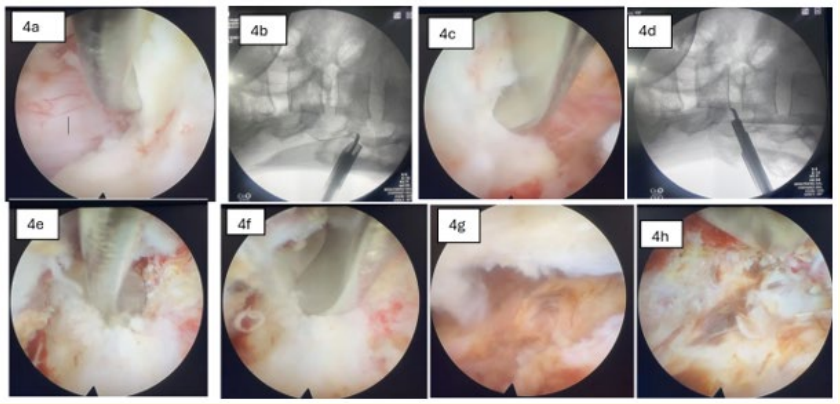
Figure 4: Intra operative endoscopic and fluoroscopic images (3 O clock position of the above images corresponds to Cranial & 9 O clock to caudal directions) 4a, upper most end of L3 lamina after removal of most of the L3 hemilamina on left side; 4b,intra op fluoroscopy confirming extent of laminectomy; 4c & d , L4 laminar edge towards caudal direction with corresponding fluoroscopic image; 4e, endoscopic visualisation eroded lower end plate of L3; 4f, L3-L4 disc; 4g, visualisation of ventral epidural abscess 4h, after clearing the ventral epidural abscess visualising beyond midline.
Pyogenic spondylitis/spondylodiscitis is one of most common causes for manifestation of epidural abscess. When an abscess is small, antibiotic therapy alone will suffice; however, when the abscess becomes large, drainage becomes mandatory. Percutaneous drainage under CT or echo guidance is commonly used for the drainage of abscesses; drainage might fail in many cases, especially in those with multiloculated abscess cavities or with thick tenacious pus [5]. In such cases open surgery might become necessary. We used posterior interlaminar endoscopic approach to reduce the invasiveness of surgery to benefit the patient in terms of less blood loss, less post op pain, early mobilisation and avoidance of implants. There are some reports on the posterolateral percutaneous endoscopic surgery for the treatment of pyogenic spondylitis [6,7] and the case series demonstrated that endoscopic approach provided early pain relief along with faster clearance of spinal infection.
Our case demonstrated that interlaminar endoscopic approach is very effective in treating epidural abscess cases. Interlaminar approach is easier as we can appreciate the anatomy well with negligible chance for Intraoperative complications. It is effective as one can easily access the epidural space and can-do better job in clearing the granulation tissue/formed pus etc.., under clear endoscopic vision.
The advantage of Endoscopy in comparison to either drainage under CT or echo guidance is that the abscess can be irrigated directly with a large amount of water and complete clearance of even formed abscess is possible with the help of endoscopic instruments. This contributes to immediate pain relief due to significant volume reduction of the abscess with excellent decompression of neural elements. Follow up MRI at done after 6 weeks of surgery showed that the abscess was almost completely diminished (Figure 2).
However, some precautions need to be taken in Interlaminar endoscopic approach especially while retracting the dural sac to access the ventral epidural abscess to avoid undue pressure and stretch on the dural sac and traversing nerve root. In general, ventral epidural abscesses are difficult to drain by traditional open surgery, whereas endoscopic approach enables us to approach the site easily and safely. This procedure can even be performed under local anaesthesia. Patients with pyogenic spondylitis are generally in an immunosuppressive state and the condition can potentially be life threatening at times. This procedure could be a treatment option for patients in a poor general condition and also in those where general anaesthesia is considered highly risky. Six weeks of antibiotic therapy is recommended for the treatment of pyogenic spondylitis [11]. We administered antibiotic therapy for 6 weeks after surgery, which led to a reduction in the inflammatory reaction and significant clinical improvement of our patient.
Posterior Interlaminar endoscopy is safe and effective technique to manage ventral epidural abscesses enabling the complete removal of the abscess leading to faster recovery. It is advantageous to the patient as there is less blood loss, less post operative pain and shorter hospital stay. Sometimes surprises may await us as in this case, our provisional diagnosis was tubercular spondylodiscitis owing to the symptoms and radiology, but it turned out to be acute pyogenic abscess from Staph aureus infection. So, tissue diagnosis is always important and should not be missed to deliver effective treatment for the patient.
Copyright: © 2024 Sukumar Sura., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.